Caring For Areola-Papillary Complex Grafts in Breast Surgery
José Humberto Cardoso Resende
DOI10.4172/2472-1905.100033
José Humberto Cardoso Resende*
Alfredo Nasser College (UNIFAN) Goiania-GO and Federal University of the State of Rio de Janeiro (UNIRIO), Brazil
- *Corresponding Author:
- José Humberto Cardoso Resende
UNIFAN, Goiania-GO, Brazil
Tel: (62) 3094-9494
Fax: (62) 3094-9714
E-mail: jresen99@hotmail.com
Received Date: November 16, 2017; Accepted Date: November 22, 2017; Published Date: December 5, 2017
Citation: Resende JHC (2017) Caring For Areola-Papillary Complex Grafts in Breast Surgery. J Aesthet Reconstr Surg. 3:10. doi: 10.4172/2472-1905.100033
Keywords
Areola; Nipples; Breasts; Mammary gigantoplasty; Areola-papillary complex
Introduction
Few cases and few techniques use the grafting of the areolapapillary complex. This procedure is used for cases where it is impossible to reimplantation through scrapings for fear of necrosis by the distance between the areola of the breast in the preoperative period and the ideal point of reimplantation called "Point A". The study aims to highlight the care when preparing the recipient area after the mammary plastic, at the site of reimplantation as a free graft and the donor part that is the areola-papillary complex, with perfect decortication of the areola amputated for subsequent grafting [1]. All this care is aimed at avoiding possible suffering and even partial or total necrosis of the grafted areola-papillary complex.
Material and Method
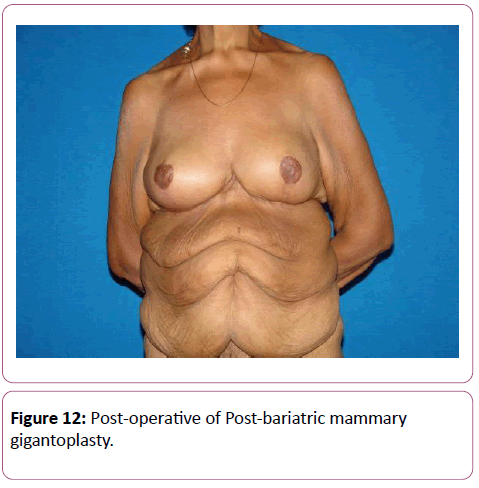
We observed our last thirty (30) cases operated by the "Resende Technique", where the amputations of the giant breasts with more than 5 kg of extirpation were used on each side. The indications were intended for women who had already lost weight from 10 to 20 kg and could not undergo bariatric surgery due to the size of their breasts and the anesthetic risks caused by thoracic suffocation in the supine position for a long surgical time [2-5].
Since the areola-papillary complexes had incompatible distances for the use of flaps to enable reimplantation, the graft was the best indication.
The surgical sequence of the chosen technique is:
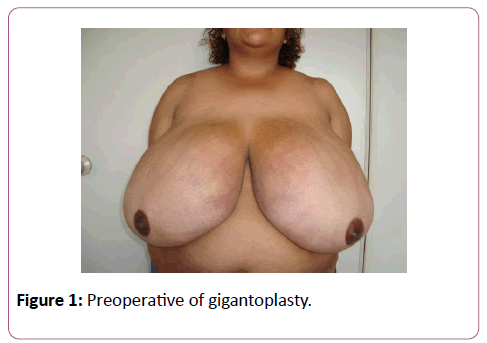
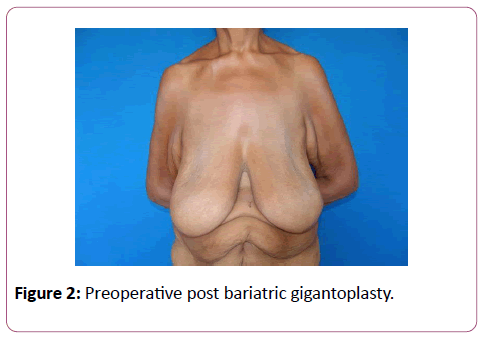
1. Foot observation of the obese giant breasts or nipple with excess skin and long distance of the areola-papillary complex after bariatric surgery (Figures 1 and 2).
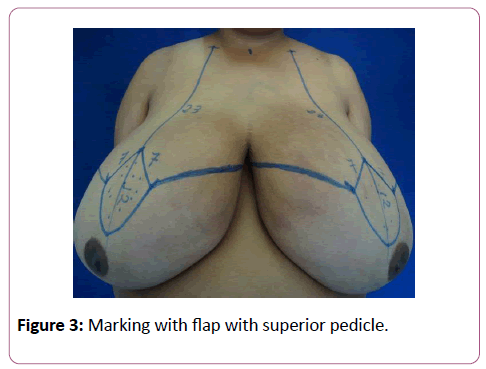
2. Marking of the ideal "A" point that varies from 20 to 22 centimeters of the right and left clavicles, in a para-median line passing from the middle of the clavicle to 7 cm from the outer thrust to the giant breast nipple (Figure 3).
3. Marking the "W", where points B and C are 10 cm apart.
4. Marking the line below the mammary line to the sides of the breasts, right and left.
5. Union of the "B" point to the end line of the inframammary line and "C" in the same way in the medial part.
6. The important thing is to think about what will stay and forget the amount that will be amputated.
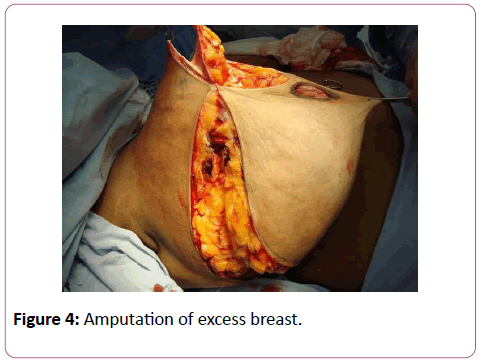
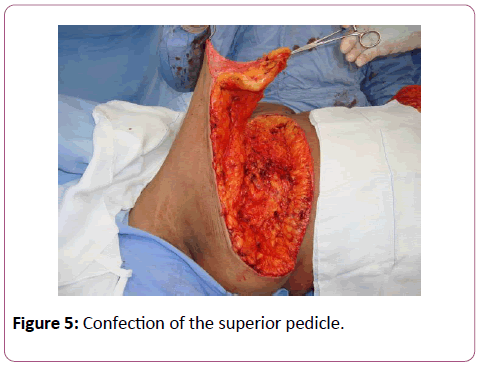
7. Finishing the marking (Figure 4), incising the lines carefully with hemostasis, first amputating the areolas that were previously marked with medium areolotomes. Then, remove all excess tissue, leaving 12 cm long and 1.5 cm thick flap in oval form with an upper pedicle on both sides (Figure 5).
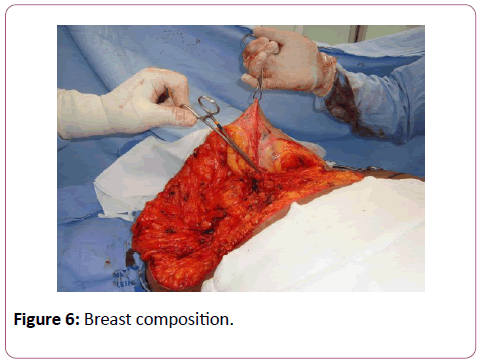
8. The next step is to take off the tissues at the top of the large dorsal muscle as placing silicone prosthesis which wills actually the decorticated pedicle flap left will be placed during the amputation of the excesses.
9. With the flap fixed in the pectoralis major muscle, the breast and posterior conventional suture of the skin are composed in the total of the incisional wounds (Figure 6).
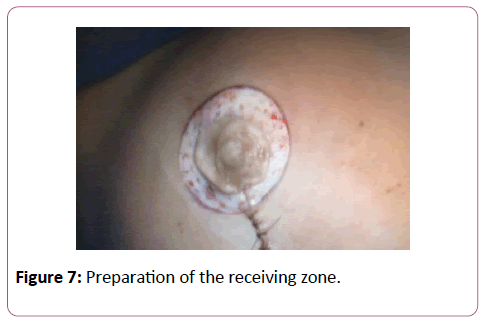
10. New marking using medium areolotome in the ideal point for the composed breast. Remember that in this technique, there will also be in the future what we call "scale", natural breasts fall. Remove the skin to make the receiving area of the areolar graft that will come [6-8] (Figure 7).
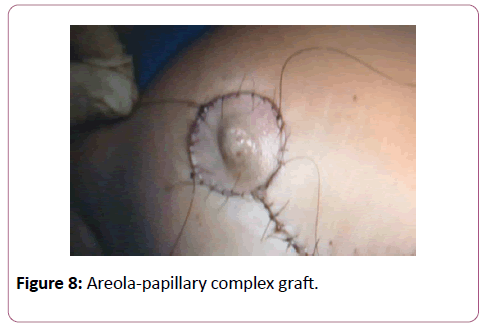
11. The amputated areola-papillary complex will undergo perfect decortication with scissors until translucent and later implanted in the receiving zone already prepared (Figure 8).
12. Brown healing for 4 (four) days with ointment and wet in saline solution (Figure 9).
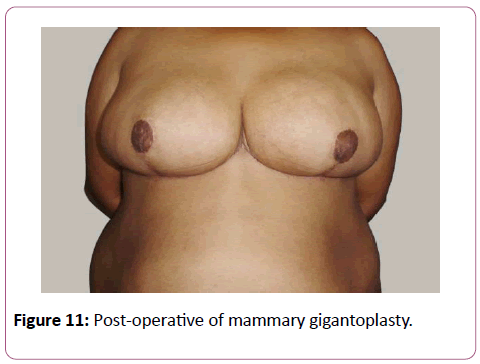
13. Post-operative (Figures 10-12).
Discussion
Many surgeons attempted to seize areolas whose pedicels had a great distance from their reimplantation. The necrosis rate was great because in flaps we must respect the proportions 1:1; 2:1; 3:1. In all cases where the ratio between base and height is greater than 3:1, prior autonomization is needed, since the terminal part of the necrotic graft. Based on these proportions, in special cases, we have to indicate the grafts of the areola- papillary complexes [9,10]. The reason for the study is to point out that if the decortication of the complex to be grafted is not perfect and translucent, there may be cases of suffering or even graft necrosis.
Results
Only two cases of the 30 observed had small sufferings on the sides of the grafts and one case of partial necrosis of the left papilla. All cases after six months were acceptable and only one case had to be tattooed after one year of surgery to reestablish the perfect contour of the areola.
References
- Hammond D, Khuthaila D, Kim J (2007) The Skate flap purse-string technique for nipple- areola complex reconstruction. Plast Reconstr Surg 120: 399-406.
- Shestak K, Nguyen T (2007) The double opposing periareola flap: a novel concept for nipple- areola reconstruction. Plast Reconstr Surg 119: 473-80.
- Di Lamartine J, Cintra Junior R, Daher J, Cammarota MC, Galdino J, et al. (2013) Reconstrução do complexo areolopapilar com double opposing flap. Rev Bras Cir Plast 28: 233-40.
- Anton LE, Hartrampf CR (1991) Nipple reconstruction with local flaps: star and wrap flaps. Perspect Plast Surg 5: 67.
- Nakagawa T, Yano K, Hosokawa K (2003) Cryopreserved autologous nipple-Areola complex transfer to the reconstructed breast. Plast Reconstr Surg 111: 141-7.
- Monteiro D (1995) Secure dressing after nipple-areola reconstruction. Ann Plast Surg 35: 220.
- Hyman J, Newman M, Gayle L (2005) Composite syringe dressing after nipple-areola reconstruction. Plst Reconstr Surg 116: 340-1.
- Bunchman H, Larson D, Huang T, Lewis SR (1974) Nipple and areola reconstruction in the burned breast. The ‘double bubble’ technique. Plast Reconstr Surg 54: 531-6.
- Losken A, Mackay GJ, Bostwick J 3rd (2001) Nipple reconstruction using the C-V flap technique: a long term evaluation. Plast Reconstr Surg 108(2): 361-9.
- Tanabe HY, Tai Y, Kiyokawa K, Yamauchi T (1997) Nipple-areola reconstruction with a dermal fat flap and rolled auricular cartilage. Plast Reconstr Surg 100(2): 431-8.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences