Skin Sparing/Reducing Mastectomy, Expander/Implant-Based Breast Reconstruction and Timing of Inflation Initiation
Bishara Atiyeh, Fadel Chahine, Nazareth Papazian and Hamed Janom
DOI10.4172/2472-1905.100009
American University of Beirut Medical Center, Beirut, Lebanon
- *Corresponding Author:
- Fadel Chahine
American University of Beirut Medical Center
Beirut, Lebanon
Tel: +961-5-956936
E-mail: fmchahine@msn.com
Received date: December 03, 2015; Accepted date: December 30, 2015; Published date: December 31, 2015
Citation: Atiyeh B, Chahine F, Papazian N. Skin Sparing/Reducing Mastectomy, Expander/Implant-Based Breast Reconstruction and Timing of Inflation Initiation. J Aesthet Reconstr Surg. 2016, 1:9. doi: 10.4172/2472-1905.10009
Abstract
Expander/implant-based breast reconstruction is currently the most commonly performed breast reconstruction technique. Most of these reconstructions are a two-stage process. After insertion of a tissue expander it is conventionally recommended to wait 10-14 days postoperatively before initiation of expansion that will usually require 6-8 weeks for completion. However, with immediate reconstruction following skin sparing/reducing mastectomy (SSM/SRM), these recommendations for initiation and rate of expansion may be questionable. Whenever ample skin flaps are enough to provide proper skin envelope for the reconstructed breast, the limiting factor to expansion initiation is the assurance of good skin flaps vascularity in the immediate post-operative period. This is usually clinically obvious, within 2-3 days at which time expansion can be initiated safely and may be completed quickly in a short time. Restoring breast mound as soon as possible minimizes post-mastectomy disfigurement and associated psychological burden.
We present our experience with one stage breast reconstruction with early and rapid expansion of Becker permanent expanders. We feel that with this expansion approach, the two-stage procedure may not be necessary; instead, one stage reconstruction with a permanent Becker expander/implant is possible and can have an aesthetically pleasing outcome.
Keywords
Skin sparing mastectomy; Breast reconstruction; Early expansion
Introduction
With evidence supporting great benefits of reconstruction following mastectomy across patient-reported outcomes, breast reconstruction is now considered an essential and integral aspect of breast cancer patients’ management and care [1]. Breast Reconstruction can be performed immediately or in a delayed setting. Various techniques each associated with different risks and benefits are available ranging from implant-based approach to autologous tissue - pedicled or free flap – reconstruction, to tissue engineering with external vacuum-based pre-expansion and fat transfer. Despite reported higher risk of reconstructive failure and surgical-site infection compared with autologous reconstruction, expander/implant-based breast reconstruction is currently the most common breast reconstruction technique performed because of shorter operative times and diminished donor-site morbidity compared to autologous tissue options. Most of these reconstructions are a two-stage process. Initially a tissue expander is inserted, followed subsequently by serial inflations that stretch the skin and stimulate tissue growth. Once the expansion is completed, the expander is removed after a maintenance period (the period for which the tissue is held at a certain strain) of at least 3-4 months and replaced by a definitive saline or gel-filled implant [1-5]. For this type of reconstruction, it is conventionally recommended to wait 10- 14 days post-operatively before initiation of expansion that will continue typically on a weekly basis, for a period of 6–8 weeks till completion. The amount of filling is controlled by visual inspection of skin color, capillary refill, and simple palpation of the stretched skin. Based on wound healing parameters and principles, some have suggested even a longer waiting period of at least 6 weeks before initiation of inflation [4,6]. The concept is deceptively simple, yet in reality it may have serious complications and yield poor results [7].
For delayed implant-based breast reconstruction where local tissues are contracted and scarred, a delay period before initiation of expansion and a slow rate of expansion are probably indicated to avoid wound dehiscence and expander extrusion. However, with immediate reconstruction following the increasingly popular skin sparing/reducing mastectomy (SSM/SRM), these recommendations for initiation and rate of expansion may be questionable. Whenever ample skin flaps are enough to provide proper skin envelope for the reconstructed breast, direct to implant single stage immediate (DISSI) reconstruction is emerging as a valid reconstruction technique [8-10]. Whenever a two-stage approach is chosen if the mastectomy skin flaps are judged not to be healthy enough to support a full-sized implant right away [11], the limiting factor to expansion initiation is the assurance of good skin flaps vascularity in the immediate post-operative period. This is usually clinically obvious, within 2-3 days at which time expansion can be initiated safely and may be completed quickly in a short time.
We present our experience with immediate one stage breast reconstruction with early and rapid expansion of Becker permanent expanders. We feel that with this expansion approach, the two-stage procedure may not be necessary; instead, a one stage reconstruction with a permanent Becker expander/implant is possible and can have an aesthetically pleasing outcome.
Materials and Method
Eight patients undergoing skin-sparing/reducing mastectomy (SSM/SRM) and immediate breast reconstruction (IBR) with permanent expanders from May 2014 till May 2015 are included in this study.
One patient required unilateral and 7 required bilateral mastectomy for a total of 15 operated breasts. Mean age of the patients was 50 (range 29–70). Mean BMI was 20.76 (range 18.01–28.28); All patients except one had a healthy BMI less than 25. Regarding smoking history, only one patient was a smoker, not exceeding 20 cigarettes per day. All patients were relatively healthy with no history of diabetes or any other co-morbidity that would impair wound healing. One patient with previous partial mastectomy and radiotherapy presented with tumor recurrence and necessitated total mastectomy. Another patient had preoperative neo-adjuvant chemotherapy. Histopathological diagnosis was lobular carcinoma in situ (LCIS) in a single patient while the remaining seven patients had ductal carcinoma in situ (DCIS) and early stage invasive ductal carcinoma with axillary nodes involvement in two of them necessitating axillary lymph nodes dissection. Seven mastectomies (Six to the right breast and one to the left breast) were performed prophylactically for patients with unilateral breast cancer and high risk for development of contralateral carcinoma. Axillary lymph node dissection was performed in 2 patients, one because of positive sentinel lymph node biopsy; the second patient had a large tumor and had received pre-operative neo-adjuvant chemotherapy. Eventually in this patient, the excised lymph nodes were free of tumor.
A Becker permanent expander (SiltexTM Contour Profile® Becker 35, Cohesive IITM) was used for reconstruction in all patients (Table 1). All implants were placed in a dual plane, sub-pectoral superiorly and subcutaneous inferiorly. Laterally the implant was covered with the serratus fascia to prevent lateral displacement. A native dermal barrier was created as previously described [8,10] and reinforced the vertical lower pole suture line whenever mastectomy was performed by a circumvertical approach. Closed suction drainage was used in all patients and antibiotics were administered and continued until drain removal.
| Patient ID | BMI | Age | Diagnosis | Surgery | SiltexTM Contour Profile® Becker 35, Cohesive IITM |
|---|---|---|---|---|---|
| RTD | 20.45 | 70 | Left Breast DCIS | Bilateral Mastectomy Left SLNB IBR |
290 cc 100cc silicone 190cc saline |
| DPF | 18.3 | 54 | Left Breast LCIS | Bilateral Mastectomy Left SLNB IBR |
325 cc 110cc silicone 215cc saline |
| CRS | 18.01 | 42 | Left Breast Infiltrating Ductal CA | Bilateral Mastectomy, Left ALND IBR |
255 cc 90cc silicone 165cc saline |
| WGM | 22.6 | 58 | Left Breast Infiltrating Ductal CA | Bilateral Mastectomy Left SLNB IBR |
565 cc 195cc silicone 370cc saline |
| MFS | 18.8 | 56 | Left Breast Recurrent Infiltrating Ductal CA | Bilateral Mastectomy Left SLNB IBR |
365cc 125 cc silicone 240cc saline |
| CJY | 20.95 | 29 | Left Breast Infiltrating Ductal CA | Bilateral Mastectomy Left SLNB IBR |
325 cc 110cc silicone 215cc saline |
| LKS | 18.75 | 31 | Left Breast Infiltrating Ductal CA | Left Mastectomy Left SLNB IBR |
255 cc 90cc silicone 165cc saline |
| TBC | 28.28 | 60 | Right Breast Infiltrating Ductal CA Neo-adjuvant Chemotherapy |
Bilateral Mastectomy Right ALND IBR |
365cc 125 cc silicone 240cc saline 60cc over-inflation |
LCIS: Lobular Carcinoma In-Situ
IBR: Immediate Breast Reconstruction
SLNB: Sentinel Lymph Node Biopsy
ALND: Axillary Lymph Node Dissection
Table 1: List of patients included in the study with their initial diagnosis, surgery performed and size f expander used for immediate breast reconstruction.
Since most patients were not operated at a university hospital, no institutional review board (IRB) approval was necessary. All patients signed an informed consent pre-operatively after details of the procedure were explained to them. The analysis was performed in compliance with the Helsinki Declaration.
Results
50cc of saline were injected in all implanted expanders intraoperatively. Expander inflation was resumed usually on the 3rd post-operative day and repeated every 3 days. Inflation was completed usually within 2-3 weeks. The recommended amount of saline was injected in all patients except in one patient in whom the bilateral expanders were over inflated by 60cc of saline. All patients tolerated the inflation protocol well; Drains were usually removed within 2 weeks whenever output was less than 25cc/24 hrs on 2 consecutive days. No complications of wound dehiscence or infection were encountered.
Discussion
In recent years, awareness of breast cancer treatment has risen dramatically. It is obvious that with better understanding of breast cancer disease and advancements in technology, surgical techniques, and new treatment modalities, women can expect nowadays better outcomes [11,12]. Nevertheless, diagnosis of breast cancer invariably leads to changes in patient-reported outcomes (PROs), specifically significant depression, anxiety, and mood disturbances [13].
The impact of the disease and subsequent treatment modalities on patients’ quality of life is being increasingly recognized [14]. Besides the obvious concerns over health and longevity, breast cancer patients are apprehensive about their appearance following a disfiguring operation. Self-perception of body image appears to be the most important factor determining quality of life after mastectomy. This perception may impact their social, personal, and sexual relationships [14,15]. With the prospect of breast reconstruction, emotional and physical results of breast cancer currently are very different from what they were in the past particularly for younger women for whom physical appearance carries more significance. Breast reconstruction in its various forms offers patients great benefits in body image, self-esteem, sexual function, and quality of life [11-13]. While autologous reconstruction patients are reported to be more esthetically satisfied with their reconstruction as compared to implant reconstruction, it is important to note that both have in the final analysis similar general satisfaction. Nevertheless, early improvements in health-related quality of life (HRQoL) domains have been reported with implant reconstruction as compared to autologous reconstruction within the first 9 months postoperatively [13,16].
The extent to which cosmetic outcomes affect the quality of life of breast cancer patients remains unclear. In fact patients' body image perception does not coincide with what surgeons consider to be an optimal reconstruction with good symmetry, nevertheless, understanding the psychological burden of the disease is crucial for comprehensive patient-specific care. Even though superior surgical cosmetic outcomes do not seem to strongly translate into improved quality of life and that there is no consensus about whether postoperative quality of life differs according to type of surgery, deterioration of HRQoL scores in nonreconstructed patients can be seen as early as 1 month following mastectomy while significant benefits can be appreciated within 3–6 months in patients undergoing reconstruction. Moreover, HRQoL scores differ greatly between patients undergoing delayed or immediate reconstruction. In contradistinction to immediate reconstruction, delayed reconstruction patients are more likely to develop acute emotional and psychological sequelae secondary to ablative surgery. Delayed reconstruction patients, however, demonstrate continued gains in HRQoL scores with the progress of their reconstruction reaching with time levels of immediate reconstruction patients. This highlights the impact of an absent breast mound on decreased HRQoL of patients [13-15].
There is no one-size-fits-all approach to breast reconstruction. Although autologous tissue breast reconstruction has some long-term advantages, women may still choose to avoid complex surgery and prefer an implant-based immediate breast reconstruction. In fact more women currently are having implantbased than autologous reconstructions. With skin sparing/ reducing mastectomy, ample, thicker and well-vascularized skin flaps made direct to implant single stage immediate (DISSI) breast reconstruction a viable option with gratifying results and definite benefits to the patients. In the event of an expanderbased reconstruction, single or two-stage, restoring the breast mound and the patient’s perception of body image as soon as possible following mastectomy cannot be over emphasized. Thus unnecessary delay in that regard must be strongly avoided.
Understanding and consciously addressing viscoelastic tissue dynamics is essential. As a basic law of the mechanics of materials, when a tissue is loaded with a force such as expansion, it produces a stress that causes the tissue to deform. However, it has been shown experimentally that both conventional expansion and rapid expansion have similar effects on biomechanical properties of expanded tissues in terms of stress-strain, elastic and plastic deformation, stiffness, compliance, resilience, and creep deformation. Improvement in biomechanical properties with effective reduction in the stretch-back ratio and maximal surface area gain can be observed only with extension of the maintaining period. It was concluded therefore that rapid expansion with an extended maintaining period could be an acceptable option in clinical practice [17,18]. In another experimental study in the dog model, it was demonstrated that issue expansion with an accelerated regimen of 2 weeks did not have any deleterious effects when compared with a conventional tissue expansion regimen of 6 weeks [19]. Moreover, the reported few soft tissue changes that occur during rapid tissue expansion in contradistinction to epidermal hypertrophy, decreased dermal, muscle, and adipose thickness observed with conventional expansion, though mostly return to pre-expansion state over time [20], is an additional argument in favor of rapid expansion whenever technically feasible.
Our results clearly demonstrate that with skin sparing/reducing mastectomy and expander-based reconstruction, early and rapid expansion can be performed safely and effectively. In standard tissue expansion procedures, delay before initiation of expansion is recommended to reduce the risk of wound dehiscence and expander extrusion. Since the main rational for implanting an expander is to avoid applying excessive tension on mastectomy skin flaps in the immediate postoperative period not to expand and recruit more skin for reconstruction, expansion may be initiated within 2-3 days postoperatively once secure and adequate flap vascularity has been confirmed. Compared to standard expansion protocol, final breast contour can be achieved within 2-3 weeks with early and rapid inflation.
It is obvious that separation of the implant from the suture line is necessary in order to avoid extrusion should skin edge necrosis and wound dehiscence occur. The question raised is total muscle coverage of the implant really necessary? In fact, it is not; on the contrary, it may be detrimental to the final aesthetic outcome [10]. With total muscle coverage, early and rapid expansion may not be possible; moreover expansion potential of the lower implant pole is restricted resulting in blunting of the infra-mammary and lateral mammary folds and leading to a rounded highriding breast with exaggerated upper-pole fullness. For superior aesthetic outcomes with lower pole fullness and some degree of ptosis, subcutaneous or dual plane placement of the implant is preferable as this provides adequate cosmetic appearance with appropriate distribution of volume between superior and inferior as well as medial and lateral aspects of the breast [21-24]. An acellular dermal matrix (ADM) or a dermal barrier may be used instead to cover and protect the lower implant pole. Another theoretical disadvantage of delaying inflation initiation time is that sometimes when placing a deflated expander in the pocket, the expander’s footprint may contract or become distorted. If a mature capsule is allowed to form in such situations, full display of the expander profile may be prevented.
Indications for performing immediate breast reconstruction in the likelihood of post-mastectomy radiotherapy are still not very clear and conflicting opinions are expressed in the literature. There is an agreement however that post-mastectomy radiation therapy adversely affects both implant-based and autologous tissue breast reconstruction and that even with modern radiation delivery techniques, any type of breast reconstruction can distort the chest wall and may interfere with the ability to treat targeted tissues without excessive exposure of the heart and lungs [25,26]. These facts must necessarily be taken into consideration and inferior cosmetic results with 40% complication rate and 15% extrusion rate associated with prosthetic breast reconstruction and radiotherapy must be balanced with undeniable benefits of immediate reconstruction and early restoration of the breast mound. Recent evidence suggests however that irradiation to the tissue expander has been associated with acceptable capsular contracture rate and revision rates have been less than expected indicating that immediate tissue expander/implant reconstruction is a reasonable surgical option in the setting of post-mastectomy radiation therapy [27].
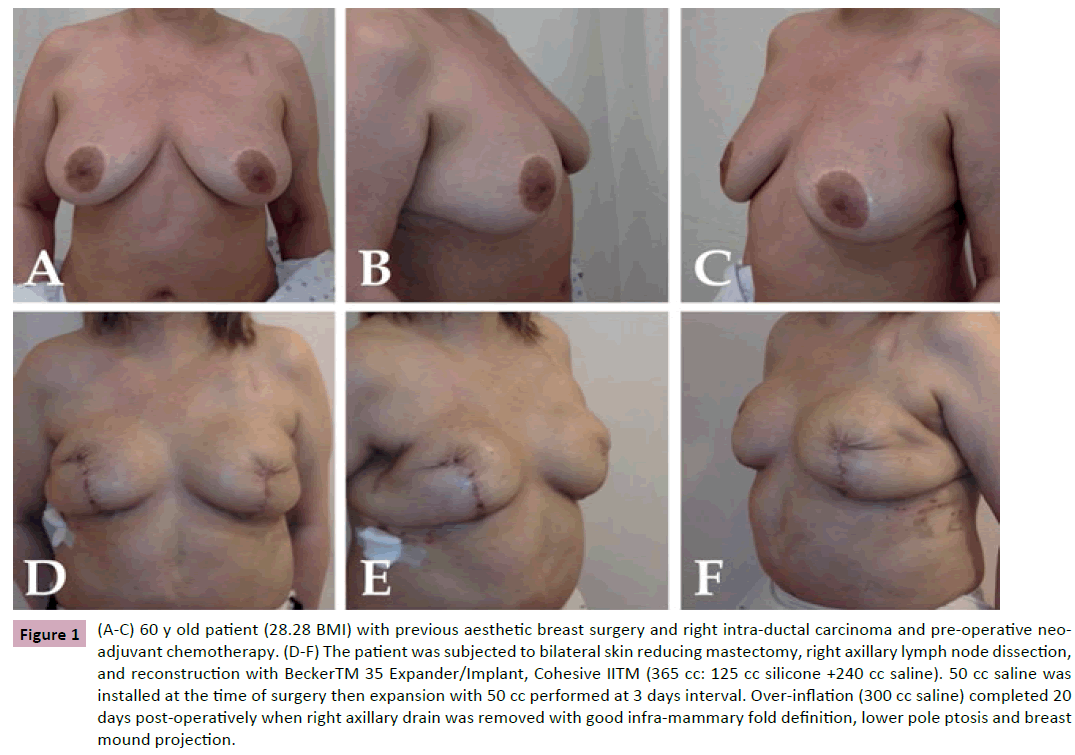
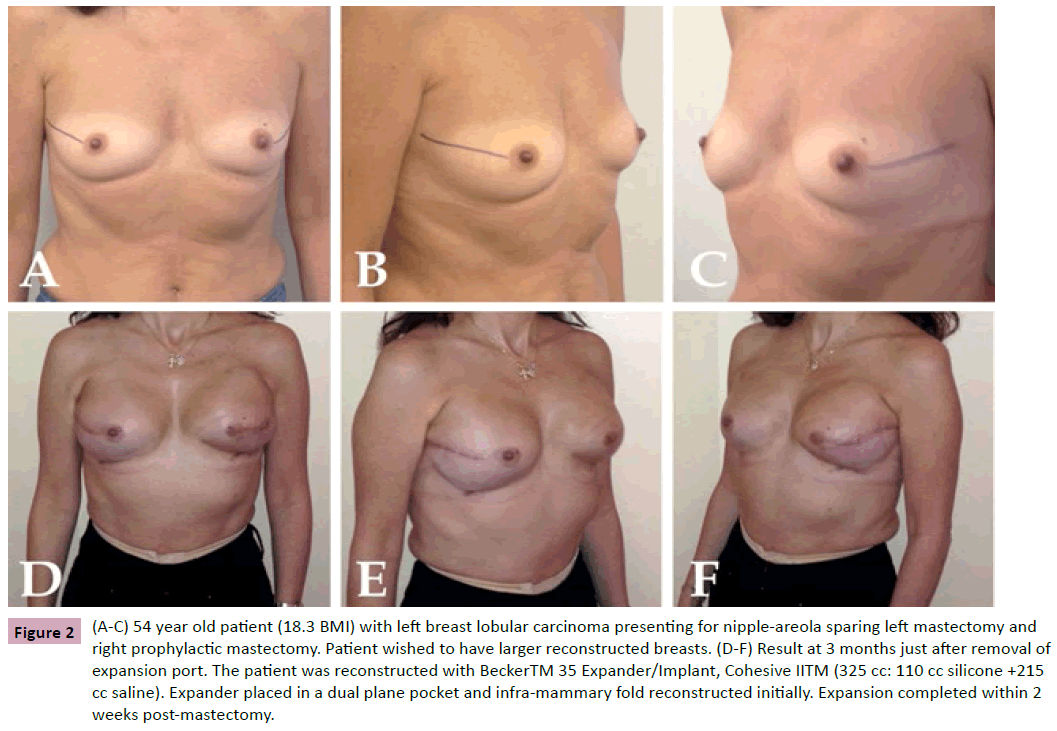
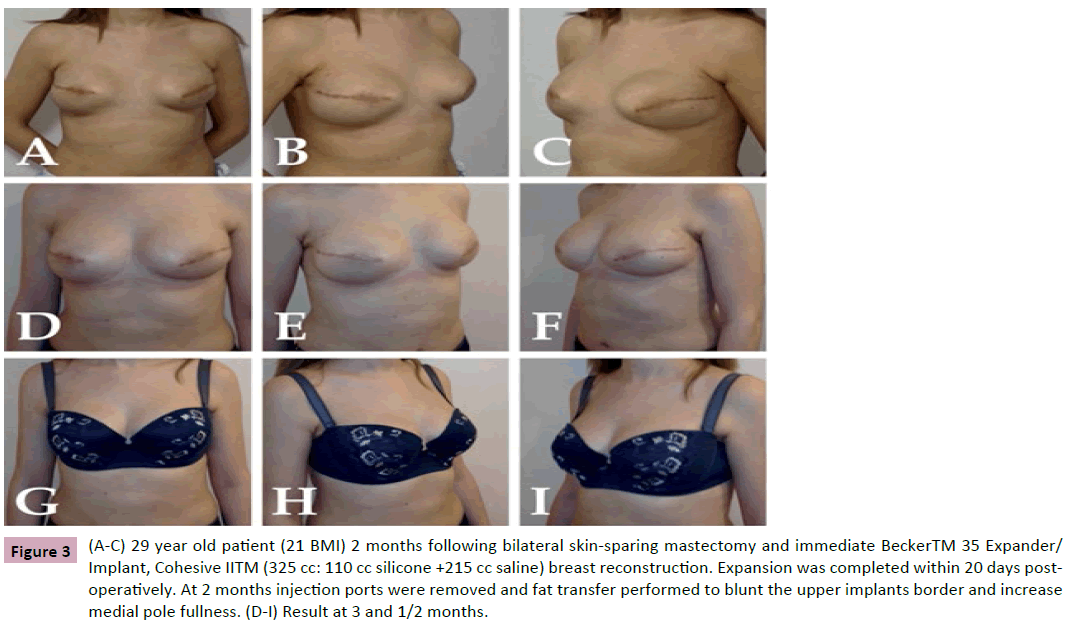
It must be noted though that when choosing to perform one stage reconstruction with a Becker permanent expander/implant, it is imperative to recognize that once the permanent expander is positioned, it cannot be adjusted at a later date, as in twostage expander/prosthesis reconstructions; thus it is essential that the infra-mammary fold be reconstructed initially and secured to the chest wall. The pectoralis major muscle has also to be completely released inferiorly and then secured to prevent superior migration [28] (Figure 1 and 2). Worth mentioning in this context that recent evidence suggests that loss of projection by an average of 21% is the norm by three months post-implant exchange in the two-stage technique. This is probably due to stress relaxation induced histologic and biochemical changes in epithelial proliferation, collagen synthesis, and recovery from expansion-induced tissue ischemia [5]. Similar loss of projection has not yet been reported with the one-stage technique. Regardless of this fact, simple lipomodelling for refinement of breast reconstructive surgery is becoming nowadays an accepted modality. It is being used to improve the cosmetic and aesthetic appearance of the breast following implantbased reconstructions and correct post-radiotherapy breast deformities. Following any type of breast reconstruction, it allows sculpturing and reshaping of the reconstructed breast, thereby achieving symmetry and enhancing softness and a natural feel [29] (Figure 3). Unfortunately, full potentials of this modality have not yet been fully explored; undeniably we feel it will make expander/implant breast reconstruction a more attractive option in a variety of clinical situations.
Figure 1: (A-C) 60 y old patient (28.28 BMI) with previous aesthetic breast surgery and right intra-ductal carcinoma and pre-operative neoadjuvant chemotherapy. (D-F) The patient was subjected to bilateral skin reducing mastectomy, right axillary lymph node dissection, and reconstruction with BeckerTM 35 Expander/Implant, Cohesive IITM (365 cc: 125 cc silicone +240 cc saline). 50 cc saline was installed at the time of surgery then expansion with 50 cc performed at 3 days interval. Over-inflation (300 cc saline) completed 20 days post-operatively when right axillary drain was removed with good infra-mammary fold definition, lower pole ptosis and breast mound projection.
Figure 2: (A-C) 54 year old patient (18.3 BMI) with left breast lobular carcinoma presenting for nipple-areola sparing left mastectomy and right prophylactic mastectomy. Patient wished to have larger reconstructed breasts. (D-F) Result at 3 months just after removal of expansion port. The patient was reconstructed with BeckerTM 35 Expander/Implant, Cohesive IITM (325 cc: 110 cc silicone +215 cc saline). Expander placed in a dual plane pocket and infra-mammary fold reconstructed initially. Expansion completed within 2 weeks post-mastectomy.
Figure 3: (A-C) 29 year old patient (21 BMI) 2 months following bilateral skin-sparing mastectomy and immediate BeckerTM 35 Expander/Implant, Cohesive IITM (325 cc: 110 cc silicone +215 cc saline) breast reconstruction. Expansion was completed within 20 days postoperatively. At 2 months injection ports were removed and fat transfer performed to blunt the upper implants border and increase medial pole fullness. (D-I) Result at 3 and 1/2 months.
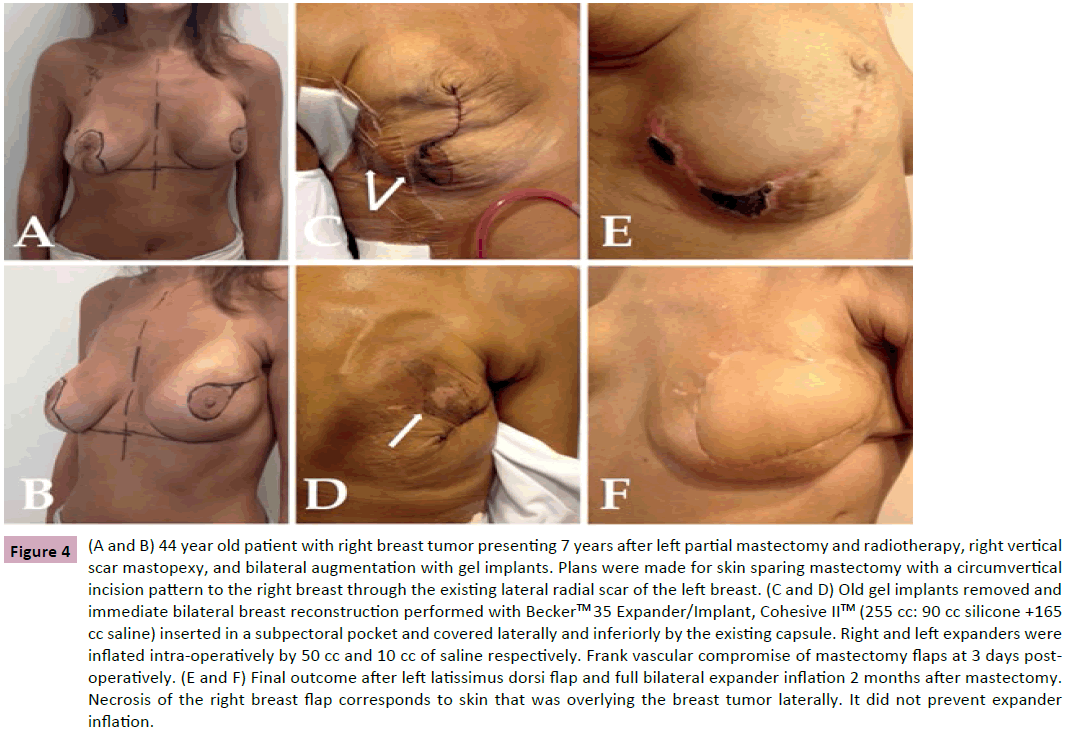
This study is however limited by being none comparative. It is also a retrospective evaluation of a small number of patients with relatively short follow up. Since writing this initial preliminary report, 3 additional cases were performed (1 unilateral and 2 bilateral reconstructions). One patient, a heavy smoker, presented with right breast tumor 7 years after left partial mastectomy and radiotherapy, right mastopexy, and bilateral breast augmentation. She underwent bilateral mastectomy and immediate reconstruction was achieved with permanent expander bilaterally since she has refused other reconstruction alternatives. Partial ischema of the thin mastectomy flaps bilaterally was suspected the following day and became evident 3 days following surgery. The unfortunate complication encountered in this patient was however of no consequence regarding the final reconstruction outcome. Ischemic skin of the right breast was treated conservatively while ischemic portion of the previously irradiated left mastectomy flap was debrided after full demarcation and replaced with a latissimus dorsi flap. Despite a limited delay, expansion could then be initiated achieving uneventful and satisfactory outcome 5 weeks following mastectomy (Figure 4). This complicated case illustrates nevertheless feasibility and safety of early and rapid inflation for expander/implant-based breast reconstruction even in complex clinical situations. It justifies as well whenever vascularity of skin flaps is in doubt, the insertion following skin-sparing mastectomy of a permanent expander instead of insertion of a gel implant that is technically possible.
Figure 4: (A and B) 44 year old patient with right breast tumor presenting 7 years after left partial mastectomy and radiotherapy, right vertical scar mastopexy, and bilateral augmentation with gel implants. Plans were made for skin sparing mastectomy with a circumvertical incision pattern to the right breast through the existing lateral radial scar of the left breast. (C and D) Old gel implants removed and immediate bilateral breast reconstruction performed with BeckerTM 35 Expander/Implant, Cohesive IITM (255 cc: 90 cc silicone +165 cc saline) inserted in a subpectoral pocket and covered laterally and inferiorly by the existing capsule. Right and left expanders were inflated intra-operatively by 50 cc and 10 cc of saline respectively. Frank vascular compromise of mastectomy flaps at 3 days postoperatively. (E and F) Final outcome after left latissimus dorsi flap and full bilateral expander inflation 2 months after mastectomy. Necrosis of the right breast flap corresponds to skin that was overlying the breast tumor laterally. It did not prevent expander inflation.
Conclusion
Breast reconstruction by tissue expansion is an important technique in the armamentarium of the reconstructive surgeon but should be used carefully and thoughtfully [7]. It is obvious that volume and interval of expansion may vary between surgeons and wound type and depend on physical findings and patient comfort [30]. This must be balanced however with the desire to achieve a breast mound as soon as possible to minimize post-mastectomy disfigurement and associated psychological burden. With skin sparing/reducing mastectomy, there is no skin shortage, and the rational for implanting a tissue expander is not to expand skin but to secure flap vascularity in the immediate postoperative period. With proper skin incisions, implantation pocket, and wound closure, expander inflation can be safely initiated few days following mastectomy and can be completed within the normal recovery period of mastectomy in 2-3 weeks. We have modified our expander inflation strategy and started applying this rapid protocol since May 2014 without so far any inflation related complications.
It goes without saying that proper patient selection, thorough preoperative planning, meticulous technique, and the ability to modify the reconstructive plan for each patient based on clinical response to tissue expansion are critical factors to achieve the desired breast reconstruction outcome [30]. Several questions remain however unanswered. Additional comparative studies are certainly needed to evaluate the long-term outcome of this reconstructive approach.
References
- Tsoi B, Ziolkowski NI, Thoma A, Campbell K, O'Reilly D, et al. (2014) Safety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: a systematic review and meta-analysis. Plast Reconstr Surg 133: 234-249.
- Alderman A, Gutowski K, Ahuja A, Gray D (2014)Postmastectomy Expander Implant Breast Reconstruction Guideline Work Group. ASPS clinical practice guideline summary on breast reconstruction with expanders and implants. Plast Reconstr Surg134:648e-655e.
- Khouri RK, Rigotti G, Khouri RK Jr, Cardoso E, Marchi A, et al. (2015) Tissue-engineered breast reconstruction with Brava-assisted fat grafting: a 7-year, 488-patient, multicenter experience. PlastReconstrSurg135:643-658.
- Tepole AB, Gosain AK, Kuhl E (2012) Stretching skin: The physiological limit and beyond. Int J Non Linear Mech47:938-949.
- Mioton LM, Jordan SW, Kim JY (2015) A prospective analysis of dynamic loss of breast projection in tissue expander-implant reconstruction. Arch PlastSurg42:309-315.
- Paek LS, Giot JP, Tétreault-Paquin JO, St-Jacques S (2015) The impact of postoperative expansion initiation timing on breast expander capsular characteristics: a prospective combined clinical and scanning electron microscopy study. PlastReconstrSurg135:967-974.
- Collis N, Sharpe DT (2000) Breast reconstruction by tissue expansion. A retrospective technical review of 197 two-stage delayed reconstructions following mastectomy for malignant breast disease in 189 patients. Brit J PlastSurg53:37–41.
- Atiyeh BS, Abbas J, Costagliola M (2012) Dermal Barrier For Immediate Prosthetic Breast Reconstruction. Rev Bras Cir Plást27:630-635.
- Atiyeh B, Dibo S, Zgheib E, Abbas J (2014) Skin sparing/skin reducing mastectomy (SSM/SRM) and the concept of oncoplastic breast surgery. Int J Surg12:1115-1122.
- Ibrahim AE, Atiyeh BS, Dibo SA, Sarhane KA, Abbas JS (2012) De-epithelialized Dermal Barrier for a Safe Immediate Prosthetic Breast Reconstruction post Circumvertical Skin Sparing/Reducing Mastectomy (SSM/SRM). Eur J PlastSurg :787-793.
- Breast reconstruction after mastectomy.American Cancer Society, USA.
- Albornoz CR, Bach PB, Mehrara BJ (2013) A paradigm shift in U.S. Breast reconstruction: Increasing implant rates. PlastReconstrSurg131:15–23.
- Chao LF, Patel KM, Chen SC, Lam HB, Lin CY, et al. (2014) Monitoring patient-centered outcomes through the progression of breast reconstruction: a multicentered prospective longitudinal evaluation. Breast Cancer Res Treat 146:299-308.
- Kim MK, Kim T, Moon HG, Jin US, Kim K, et al. (2015) Effect of cosmetic outcome on quality of life after breast cancer surgery. Eur J SurgOncol41:426-432.
- Eltahir Y, Werners LL, Dreise MM, van Emmichoven IA, Jansen L, et al. (2013) Quality-of-Life Outcomes between Mastectomy Alone and Breast Reconstruction: Comparison of Patient-Reported BREAST-Q and Other Health-Related Quality-of-Life Measures. Plast Reconstr Surg 132:201e-209e.
- Alderman AK, Kuhn LE, Lowery JC, Wilkins EG (2007)Does patient satisfaction with breast reconstruction change over time? Two-year results of the Michigan Breast Reconstruction Outcomes Study. J Am Coll Surg 204:7-12.
- Zeng YJ, Xu CQ, Yang J (2003) Biomechanical comparison between conventional and rapid expansion of skin. Br J PlastSurg56:660–666.
- Vegas MR, Martin Del Yerro JL (2013) Stiffness, compliance, resilience, and creep deformation: understanding implant-soft tissue dynamics in the augmented breast: fundamentals based on materials science. Aesthetic Plast Surg 37:922–930.
- Mustoe TA, Bartell TH, Garner WL (1989) Physical, biomechanical, histologic, and biochemical effects of rapid versus conventional tissue expansion. Plast Reconstr Surg83:687-691.
- Johnson TM, Lowe L, Brown MD, Sullivan MJ, Nelson BR (1993) Histology and physiology of tissue expansion. J DermatolSurgOncol19:1074-1078.
- Li FC, Jiang HC, Li J (2010) Immediate breast reconstruction with implants after skin-sparing mastectomy: a report of 96 cases. Aesthetic PlastSurg34:705-710.
- Colizzi L, Agostini T, Pascone C, Gandini D, Pantaloni M, et al. (2010)Adermomuscular pocket provides superior coverage of the implant in skin-reducing mastectomies. Aesthetic PlastSurg34:675-677.
- Nava MB, Cortinovis U, Ottolenghi J, Riggio E, Pennati A, et al. (2006) Skin-reducing mastectomy. PlastReconstrSurg118:603-610.
- Bayram Y, Kulahci Y, Irgil C, Calikapan M, Noyan N (2010) Skin reducing subcutaneous mastectomy using a dermal barrier flap and immediate breast reconstruction with an implant: a new surgical design for reconstruction of early-stage breast cancer. AesthPlastSurg34:71–77.
- Lam TC, Hsieh F, Boyages J (2013) The effects of postmastectomy adjuvant radiotherapy on immediate two-stage prosthetic breast reconstruction: a systematic review. PlastReconstrSurg 132:511-518.
- Kronowitz SJ1, Robb GL (2009) Radiation therapy and breast reconstruction: a critical review of the literature. PlastReconstrSurg124:395-408.
- Ho AL, Bovill ES, Macadam SA, Tyldesley S, Giang J, et al. (2014) Postmastectomy radiation therapy after immediate two-stage tissue expander/implant breast reconstruction: a University of British Columbia perspective. PlastReconstrSurg134:1e-10e.
- Farace F, Faenza M, Bulla A, Rubino C, Campus GV (2013)Is mammary reconstruction with the anatomical Becker expander a simple procedure? Complications and hidden problems leading to secondary surgical procedures: a follow-up study. J PlastReconstrAesthetSurg66:741-746.
- Bonomi R, Betal D, Rapisarda IF, Kalra L, Sajid MS, et al. (2013) Role of lipomodelling in improving aesthetic outcomes in patients undergoing immediate and delayed reconstructive breast surgery. Eur J Surg Oncol39:1039-1045.
- LoGiudice J, Gosain AK (2003) Pediatric tissue expansion: Indications and complications. J Craniofac Surg14:866–872.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences