A Brief History of Tissue Expansion and Lessons from Using a Novel Reverse Tissue Expansion Technique: A Case Review
J. Sarah Crowley and Marek Dobke*
Department of Surgery, Division of Plastic Surgery, UC San Diego School of Medicine, San Diego, CA, USA
- *Corresponding Author:
- Dr. Marek Dobke
Department of Surgery, Division of Plastic Surgery
UC San Diego School of Medicine, 200 West Arbor Drive
San Diego, CA 92103-8890, USA
Tel: +6195436084
E-mail: mdobke@health.ucsd.edu
Received Date: September 15, 2020; Accepted Date: October 28, 2020; Published Date: November 11, 2020
Citation: Crowley JS (2020) A Brief History of Tissue Expansion and Lessons from Using a Novel Reverse Tissue Expansion Technique: A Case Review. J Aesthet Reconstr Surg Vol.6 No.3:15
DOI: 10.36648/2472-1905.6.3.65
Abstract
Background: The tissue expander is made up of an inflatable balloon that is inserted into a pocket of tissue. It undergoes inflation to stretch out the overlying tissue envelope through gradual expansion. We describe a method of using tissue expanders in down-sizing overly augmented breasts through gradual deflation of tissue expanders, in what we call reverse tissue expansion.
Methods: The patient is a 49-year-old woman who had undergone prior bilateral breast augmentation with 1200 cc saline implants. She had associated neck pain and underwent implant exchange to 800 cc implants. She presented to us for consultation as she desired further reduction in implant size due to continued pain. She had a significantly stretched skin envelope and a smaller implant exchange would require a bilateral mastopexy. However, the patient did not want the scars of a mastopexy. We discussed with her a technique of placing tissue expanders with gradual deflation taking advantage of tissue recoiling and subsequent replacement with smaller implants.
Results: Once the expanders were deflated to appropriate size, they were removed and 345 cc silicone implant exchange was performed successfully without need for bilateral mastopexy. Patient was satisfied with the aesthetic results and resolution of her pain.
Conclusion: We describe a unique method of using tissue expanders in a reversal method through gradual deflation. Through this method of utilizing tissue recoiling, we were able to avoid creating additional scarring with mastopexy incisions. To the best of our knowledge, this method has not been previously described and appears worthy to consider in similar situations.
Keywords
Tissue expansion; Breast augmentation
Introduction
The concept of the expansile and elastic nature of human skin and soft tissues has been described for thousands of years in tribal customs and in the history of medicine, as early as 25 BC- 50 AD when Celsus described stretching the skin to approximate skin flaps to facilitate wound closure [1-3]. Throughout the ensuing years there has been documentation of lengthening bone and also serial excisions with expansion of skin through prolonged tension [4,5]. In 1957, Neumann reconstructed a partially avulsed ear by placing a posterior auricular subcutaneous rubber balloon that he gradually inflated with air over a period of two months. Through this innovative method, he expanded the surrounding skin and was able to reconstruct the ear with “like with like” tissue. In 1967 Gibson and Kenedi definitively explained the biomechanical properties of skin under tension [6]. They were the first to describe the concepts of “creep” as a constant load that is applied to skin causing an increasing amount of skin extension over time, as well as the concept of “stress-relaxation” or the force required to maintain skin stretched out at a fixed length that decreases overtime [6]. Skin under tension can be permanently stretched three to four times its original length and thus could facilitate closures of wounds with tissue deficit [6].
Almost twenty years later, Radovan and Austad independently invented the silastic saline-filled temporary tissue expander [7,8]. In 1976 Radovan began using the expander for reconstruction in post-mastectomy defects. Since then, the tissue expander has revolutionized reconstructive plastic surgery and is used in almost every part of the body. Tissue Expanders allow expansion of the surrounding soft tissues and reconstruction with tissue of the same color, texture, hair-bearing qualities and innervations [9]. Today we know that there are histological changes and biological growth that the soft tissues undergo while being mechanically stretched. While the skin is being expanded, the epidermal thickness increases, there is hyperpigmentation, the dermis layer becomes thinner, a dense fibrous capsules forms around the implant, and there is increased angiogenesis due to temporary hypoxia [10]. However, all of these changes gradually return back to normal preoperative state over 4-6 weeks after the expander is removed [9].
We used these various concepts of tissue recoiling and contractility to implement an innovative method of reverse tissue expansion in our patient who did not want to undergo mastopexy following smaller implant exchange.
Case Presentation
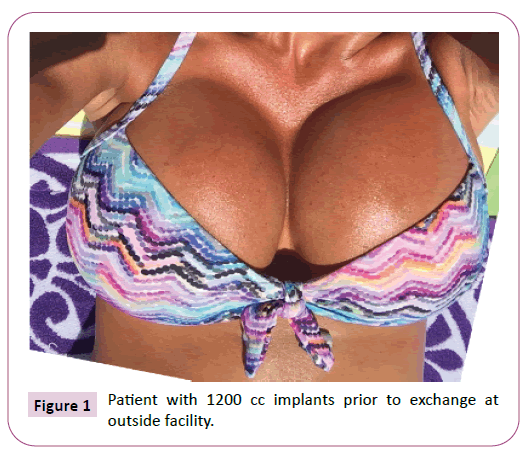
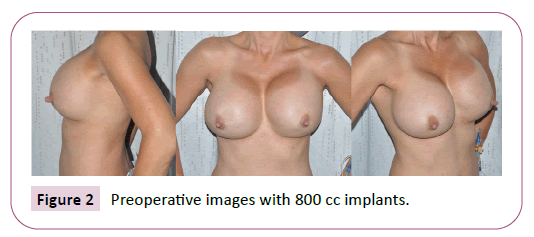
At the time of presentation, our patient was a 48-year-old healthy woman with negative past medical history who presented to us with concern for large implants that were causing her pain. She had a history of undergoing prior breast augmentation at an outside facility with custom made 1200 cc saline implants (Figure 1). These caused her significant neck and back pain. For cervical spine instability and derangements she underwent spine C4-C6 fusion surgery. Mammary implants were eventually exchanged to lighter and smaller 800 cc implants in 2015 prior to her presentation. However, she continued to have back pain that was not amenable to physical therapy, massage therapy, steroid injections and pain medications. Other than neck problems she was healthy and had no other medical problems. She was a non-smoker and there was no history of breast cancer in her family. Physical examination revealed a petite frame with a BMI of 21.4. She had soft bilateral breast implants without evidence of contractures. Breast measurements for the Right breast were sternal notch to nipple-25 cm, nipple to inframammary fold- 7 cm, nipple areolar complex- 4.3 cm and for the Left breast sternal notch to nipple- 25 cm, nipple to inframammary fold 8 cm, and nipple areolar complex- 4 cm. Her pinch test was >2 – 2.5 cm. She had no evidence of striae and had very good skin tone, quality and elasticity (Figure 2).
She was interested in exchanging her implants to smaller implants as the 800 cc implants continued to cause her discomfort and cervicobrachial pain. We discussed with her multiple options including implant removal alone, single stage implant removal with mastopexy or implant removal with exchange to a smaller implant. We did counsel her that given the significant amount of stretch on her tissues, removal of the implant alone or changing alone to a smaller implant would cause folding, a flattened appearance and contour deformity that would not be aesthetically pleasing. In order remove the excess skin and tissues that had been chronically stretched, we recommended a mastopexy along with implant exchange. However, the patient did not want new external incisions for a mastopexy. Additionally, she was concerned about the possibility of continued back pain with even a smaller implant. We discussed with her a novel technique of removing her implants and replacing with tissue expanders filled to a similar amount and then gradually deflating the tissue expanders over several months while allowing her skin and soft tissue envelope to contract in. In this manner, the patient could stop the deflation at the new desired size of the implant as well as evaluate what size and implant weight would alleviate her back pain, while obviating the need for new scars.
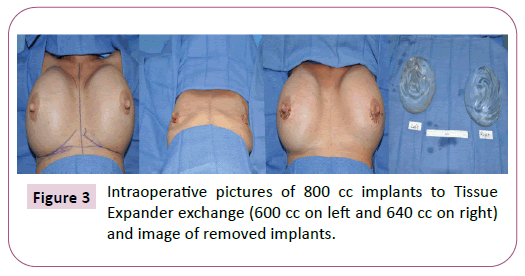
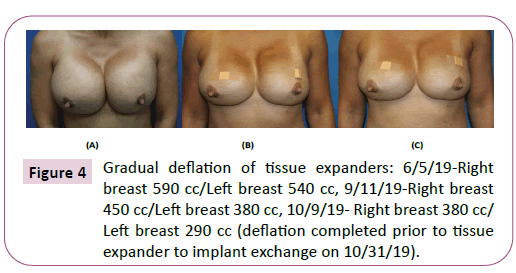
Our patient underwent removal of bilateral subglandular 800 cc silicone implants on 5/13/2019. Incisions were made through her previous inferior peri-areolar scars. Implants were found to be intact (Mentor) (Figure 3). We chose textured tissue expanders that were transversely matching the dimension of the internal pocket, 15 cm. The expander was 14 cm in vertical height projection. Small capsulotomies were made at the 9 o’clock position on the right and 3 o’clock position on the left as radial incisions approximately 4 cm long. The tissue expanders were filled to 100 cc ex vivo, and then to 600 cc in vivo on the left and 640 cc in vivo on the right for symmetrical effect. Then over the next 6 months, she proceeded to undergo gradual deflation taking advantage of tissue recoiling. She had 40-60 ccs removed from each tissue expander at each visit. During the gradual deflation it was noted that the recoiling effect was not symmetrical and by the time deflation was completed the left expander contained 290 cc and the right 380 cc. They were deflated carefully evaluating symmetry between each breast (Figure 4).
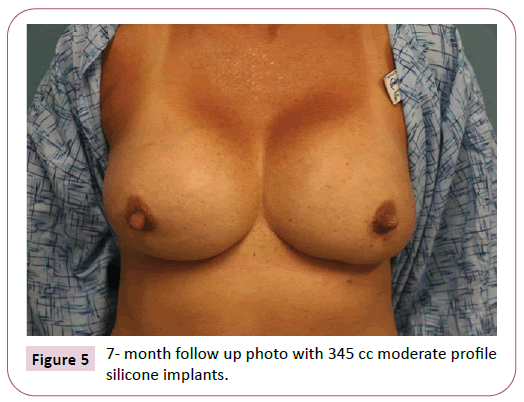
Then she underwent subsequent removal of the tissue expanders on 10/31/19, along with bilateral capsulotomy and capsulorrhaphy-to ensure”medial” implant position and reduce lateral projection. Tissue expanders were then replaced with 345 cc moderate profile silicone implants bilaterally without need for mastopexy with patient satisfactory outcome. Capsulorrhaphy was used to decrease the breast width size bilaterally. The patient is very happy with her results and also has neck/back pain relief (Figure 5).
Discussion
Our case review describes an innovative way to utilize tissue expanders, and to the best of our knowledge, has not been previously described elsewhere. Our patient had a significantly stretched skin envelope due to over-sized implants, much in the way the skin quality would be after use of a tissue expander. However, by utilizing the ability of expanded tissue to revert back to normal gradually over time, we were able to decrease the size of her breasts in a controlled manner, through gradual tissue expander deflation, or what we refer to as “reverse tissue expansion.”
When performing a Pubmed search for “reverse tissue expansion” there were a few articles that described similar concepts to our case review. Cutrignelli et al. describes in his series of 24 patients, Breast Reconstruction with Fat Grafting “Reverse Tissue Expansion, a technique that also uses a tissue expander. The described method uses a tissue expander following mastectomy that is then filled to desired expansion. The expander is then deflated by approximately 100-150 cc of saline, with the same amount fat grafted to the breast. This procedure is then repeated with 6-month intervals until the tissue expander is fully deflated and removed with a final 60 cc of fat grafted to take up the space of the removed expander [11]. The use of the tissue expander allows for fewer surgical steps as the expander allows for a greater volume of fat to be engrafted and the “consensual volumetric increase of the receiving site.”
Fabiocchi et al. also describes a very similar technique of tissue expander deflation and fat grafting in their paper “Reverse Expansion”: A New Technique of Breast Reconstruction with Autologous Tissue in 57 patients. They compare their technique to external tissue expansion with the BRAVA system. Preexpansion allows for increased graft-to-capacity ratio, decreased ischemia and allows for improved survival of grafted fat [12].
Ibrahim et al. describes a unique technique of “reverse tissue expansion” for post-surgical thigh scar revisions. Instead of expanding tissues to make excess skin, the authors describe a method of deflating skin through liposuction to allow for excess available skin at sites that require scar revision. The authors advocate for liposuction to create excess tissue, rather than tissue expanders to avoid multiple operations and office visits. Teo et al.’s technique of “reverse tissue expansion” describes a method of compression bandaging 2-4 weeks prior to excision of lower extremity soft tumor excisions in elderly patients. There is decreased elasticity in elderly patients and compression bandaging results in reduction of calf volume but allows the skin envelope to remain static which creates skin laxity and easier closure of the wound following tumor excision [13].
Our method describes a unique method of deflating tissue expanders for planned smaller implant exchange, but there are limitations. In our case we used textured tissue expanders, as our operation was completed prior to the recall of textured expanders and implants by the FDA. Although as of date there are no documented cases of Anaplastic Large Cell Lymphoma (ALCL) secondary to textured tissue expanders, there is a potential risk given that all cases of ALCL have been associated with textured implants. Another limitation is that during deflation, tissue recoiling was not symmetrical between both breasts and asymmetry was noted in terms of the amount of fluid removed at each time. Deflation had to be carefully monitored between each breast for symmetry and the amount changed at each visit. Our technique would need to be applied in the future with modifications.
Conclusion
Our described method of reverse tissue expansion is best indicated for patients with good dermal quality, elasticity without striae and with appropriate nipple position in order to allow for appropriate skin recoiling and contraction with continued deflation of the tissue expanders. Through this method we were able to avoid creating additional scarring with mastopexy incisions. To the best of our knowledge, our unique method has not been previously described elsewhere and should be considered in similar situations and patient demographics with potential modifications.
References
- Yank WB (1945) Meets native. Natl Geogr 88.
- Bennett RG, Hirt M (1993) A history of tissue expansion. Concepts, controversies, and complications. J Dermatol Surg Oncol 19(12): 1066-1073.
- Patterson TJS (1977) The Zeiss Index and history of plastic surgery. BRJ 2:1.
- Wilfrid JSP (1948) Serial Excision. Br J Plast Surg 1: 117-118.
- Jordan CJ, Goldstein RY, McLaurin TM, Grant A (2013) The evolution of the Ilizarov technique: part 1: the history of limb lengthening. Bull Hosp Jt Dis 71(1): 89-95.
- Gibson T, Kenedi RM. Biomechanical properties of skin. Surg Clin North Am. 1967;47(2): 279-294.
- Austad ED, Rose GL (1982) A self-inflating tissue expander. Plast Reconstr Surg. 70(5): 588-594.
- Radovan C (1982) Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg 69(2): 195-208.
- Agrawal K, Agrawal S (2012) Tissue regeneration during tissue expansion and choosing an expander. Indian J Plast Surg 45(1): 7-15.
- Pasyk KA, Argenta LC, Hassett C (1988) Quantitative analysis of the thickness of human skin and subcutaneous tissue following controlled expansion with a silicone implant. Plast Reconstr Surg 81(4): 516-523.
- Cutrignelli MDA, Armenio A, Maiorella A, Porcelli G, Nardulli ML, et al. (2018) Breast Reconstruction with Fat Grafting Using “Reverse Tissue Expansion”. Plast Reconstr Surg Global Open 6(2): 1.
- Fabiocchi L, Semprini G, Cattin F, Dellachiesa L, Fogacci T et al. (2017) 'Reverse expansion': A new technique of breast reconstruction with autologous tissue. J Plast Reconstr Aesthet Surg 70(11): 1537-1542.
- Teo I, Cairns S, Stephenson AJ (2014) Reverse tissue expansion. Ann R Coll Surg Engl 96(3): 239.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences