Frequency and Pattern of Nasal Septal Deviation and Outcome of Surgery in Elective Rhinoplasty Patients
Seyed Esmail Hassanpour 1* and Shahin Behjoo 2
Seyed Esmail Hassanpour* and Shahin Behjoo
Department of Plastic Surgery, 15 khordad Educational Hospital, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
*Corresponding Author:
Dr. Seyed Esmail Hassanpour
Professor of Plastic Surgery
Department of Plastic Surgery, 15 khordad Educational Hospital
School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Tel: +989122958078
E-mail: Hassanpour1394@sbmu.ac.ir
Received Date: August 04, 2020; Accepted Date: September 16, 2020; Published Date: October 23, 2020
Citation: Hassanpour SE, Behjoo S (2020) Frequency and Pattern of Nasal Septal Deviation and Outcome of Surgery in Elective Rhinoplasty Patients. J Aesthet Reconstr Surg Vol.6 No.3:14
DOI: 10.36648/2472-1905.6.3.64
Abstract
Introduction: Nasal septal deviations(NSD) play a crucial role in functional nasal breathing and unrecognized deviations stand as the primary reason for failed rhinoplasty outcomes. Although nasal septal deviation is quite common in general population but its frequency and dominant patterns varyin different studies, especially in patients presenting for aesthetic rhinoplasty. Current study addresses this issue and also evaluates clinical outcome of our septoplasty technique for each type of NSD which may have practical implications for diagnosis and management purposes. Methods: In a prospective study 101 consecutive patients presenting with aesthetic nasal deformity with or without problem in nasal breathing entered the study from June 2018 to December 2019 and operated at 15thKhordad Plastic Surgery Center, Tehran, Iran. Patients were asked to complete the Rhinoplasty Health Inventory and Nasal Outcomes (RHINO) questionnaire before and after surgery which stands as a standard subjective point of reference for both aesthetic and functional rhinoplasty outcome. Results: Most patients underwent formal septorhinoplasty by open approach and were followed up ranging from 12 to 64 weeks after surgery. Significant nasal obstruction was diagnosed in 55 patients according to preoperative assessment and paranasal sinus CT scan was performed in about two thirds of the patients. The overall frequency of NSD was 69 cases(68.3 %) with the most common type being septal tilt (33.3%),followed by C or reverse C type in anteroposterior plane (31.8%) with dominant external deviation to the right side of the patient. Septal spurs followed by craniocaudal plane deviations were observed less frequently. The difference between preoperative and postoperative RHINO scores ranged from −5 to +66, with a mean difference of 29.5±16.1 which translates into a significant improvement in both aesthetic and functional outcome in the majority of patients. Also technical aspects of our septoplasty technique is reviewed briefly. Conclusion: Stepwise approach to diagnosis and surgical management of each type of nasal septal deviations is an important and integral part of any rhinoplasty procedure and has a significant impact on both the clinical outcome and patient satisfaction.
Keywords
Nasal septal deviation; Types of septal deviation; Septoplasty technique; Functional rhinoplasty; RHINO scale
Introduction
Nasal septal deviation (NSD) plays a central role in nasal obstructive symptoms, aesthetic appearance of the nose, increased nasal airway resistance, and sometimes snoring [1]. Consequently, a comprehensive assessment of the nasal septum serves an essential role in preoperative planning, re-establishing function, and overall cosmetic outcome. Septal deviations play a crucial role in functional nasal breathing. Unrecognized internal nasal septal deviations stand as the primary reason for failed rhinoplasty outcomes due to its pivotal role in migration and further deviation of nasal bones and lateral cartilages.
Although nasal septal deviation (NSD) is quite common in the general population but its precise frequency remains unknown. Different studies show different results with some articles reporting as high as 75 to 80 percent [2-4]. Not surprisingly the frequency may be higher in patients requesting aesthetic rhinoplasty. This variability is in part due to different approaches to the diagnosis and/or study in different population of patients and absence of subjective obstructive symptoms in many cases.
On the other hand assessment of pattern and severity of nasal obstruction and quantification of NSD as well as efficacy and outcomes of treatment in rhinoplasty is a matter of great debate. This may be due to lack of consensus in terms of approach to the diagnosis, verifying the precise location, quantifying the degree of deviation, and assessing its clinical impact on patients. Consequently various classification systems has been developed for description of nasal septal deviation, a summary of the subject is covered by Teixeira et al. [5].
Also for outcome assessment a variety of objective and subjective measures have been used with different success rate. A well-recognized criticism of objective outcome measures in rhinoplasty is the frequent and often significant divergence between objectively quantifiable measurements and subjective patient-reported outcomes [6].
As a result, subjective quality-of-life (QOL) instruments have assumed an increasingly prevalent role in the assessment of outcomes after nasal surgery [7,8] This is intuitive to cosmetic nasal surgery as patient satisfaction is the most critical indicator of a successful outcome but is also equally as applicable to functional rhinoplasty. Therefore the reference tool for this study was also based primarily on subjective QOL queries.
The objective of this study is to examine the frequency and prevalent types of nasal septal deviation and also determine the clinical outcome of our septoplasty technique for each type in elective rhinoplasty patients. This in turn may have practical implications for management purposes which will be addressed in the study discussion.
Patients and Methods
In a prospective study consecutive patients presenting to plastic surgery clinic at 15th of Khordad Plastic Surgery Center with aesthetic nasal deformity with or without problem in nasal breathing were enrolled. All patients were consented for the study using an informed consent document reviewed and approved by Research Ethics Board, Shahid Beheshti University of Medical Sciences (SBMU), Tehran, Iran.
Exclusion criteria comprised of patients younger than 17 years of age, severe and refractory cases of rhinosinusitis, patients with underlying craniofacial anomalies including cleft lip nose deformity, history of medical comorbidities not fit for surgery and mentally unstable patients with unrealistic expectations from surgery.
After exclusion of above groups 101 patients were entered in the study, gathering the data prospectively by consecutive enrolment of patients. The study period extended from June 2018 to December 2019during which time admission and surgeries were performed by the senior author (SEH) and the plastic surgery team. Patients were followed for a minimum of 3 months postoperatively.
After enrolment a detailed patient history including history of nasal trauma, previous nasal surgery, airway complaints and allergies was obtained. Complaints of nasal obstruction were further clarified as whether symptoms occurred during quiet or heavy inspiration or both and also if the obstruction was constant or intermittent in nature.
Rather than complete external examination with respect to nasal and facial features, focus was made on internal exam with anterior rhinoscopy and direct visualization of the anterior third of the nasal cavity, including the external and internal nasal valves, septum, and turbinates. The septum was also evaluated for pattern of deviation and perforation. A PNS CT scan was not performed routinely but selectively and based on three indications: presence of obstructive symptoms, history of nasal trauma or the presence of overt external nasal deviation.
Patients enrolled in the study were asked to complete the The Rhinoplasty Health Inventory and Nasal Outcomes (RHINO) Questionnaire, a 10-item inventory which evaluates outcome in three health domains including physical, mental, and social well- Being [9]. This form was completed on 3 separate occasions: (1) preoperatively at the consultation visit, (2) preoperatively on the day of surgery and (3) postoperatively at least 3 months after surgery. The RHINO instrument is demonstrated in Figure 1.
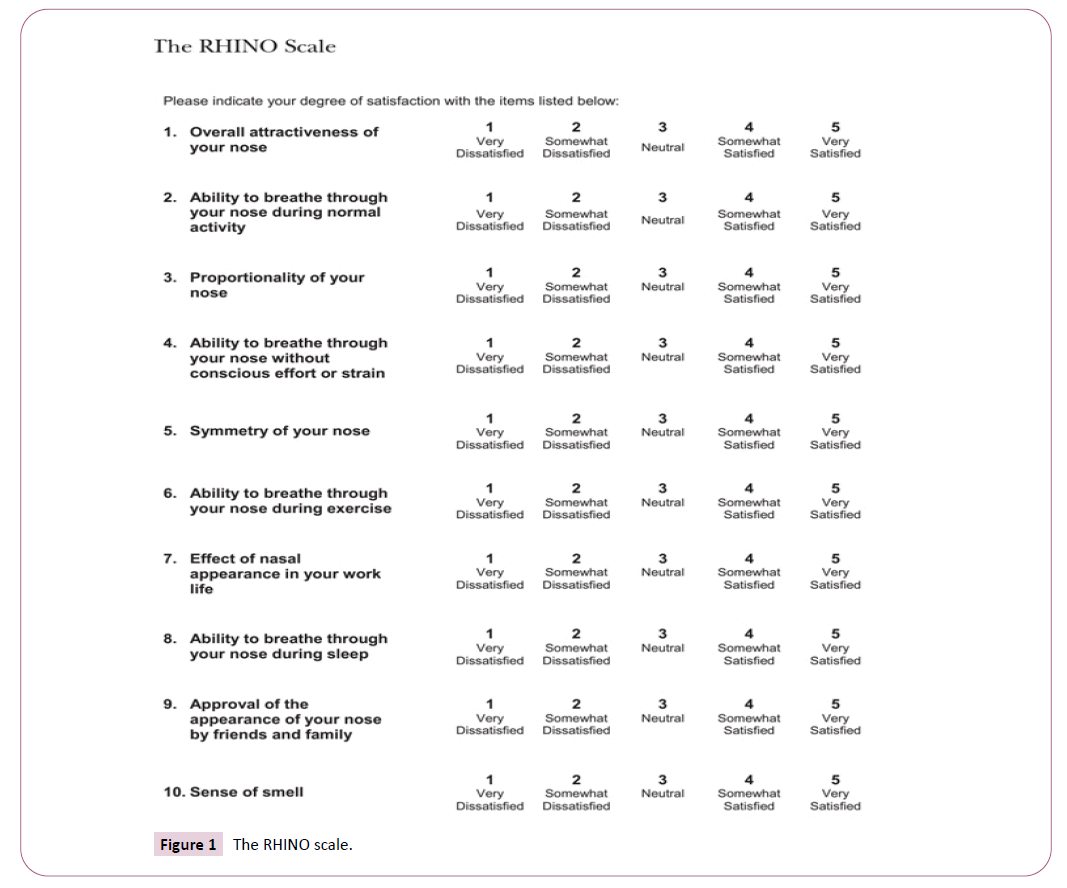
Figure 1: The RHINO scale.
Statistical analysis was completed using SPSS version 22.0 (IBM Corp., Armonk, NY, USA). Test-retest reliability was assessed via Pearson’s correlation coefficient.
Surgery was performed basically on a day care setting under general anaesthesia. Most patients were operated by classic open approach septorhinoplasty. Septoplasty procedure was individualized on each patient according to the type and severity of NSD and external nasal deformity. Our preferred approach to management of septal deviation was based on classification by Guyuron et al. [10] which classifies NSD to six types, summary of which is shown in Figure 2.
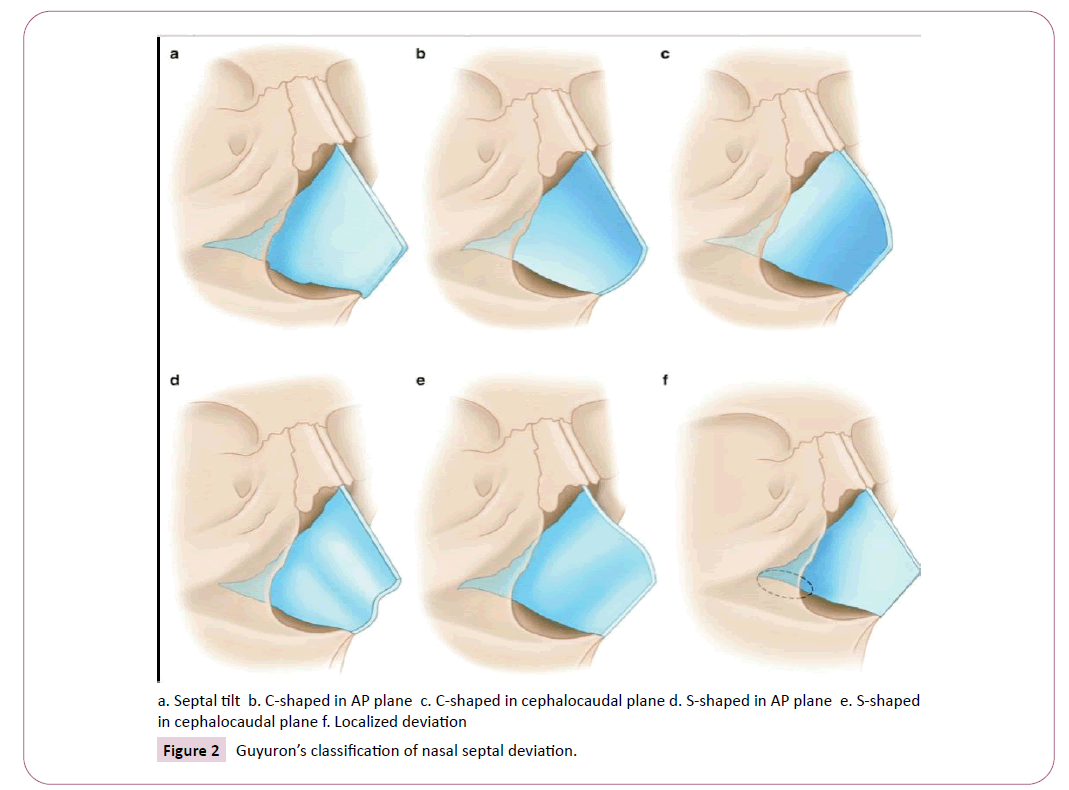
Figure 2: Guyuron’s classification of nasal septal deviation.
Results
101 patients were included in this study which consisted of 78 female and 23 male patients with a mean age of 29.2 years (Tables 1 and 2). All 101 patients contributed in the study follow-up. However eighty four patients (83.1%) attended the postoperative follow-up visits at timely intervals in person. The remaining 17 patients were contacted and interviewed by phone calls. Followup time ranged from 12 to 64 weeks, with an average of 25 weeks. Technical aspects of septoplasty are summarized in Table 3 and are described in a stepwise approach with more detail in the discussion of the article.
Table 1 Patient data.
Table 2 Age distribution of studied patients.
Table 3 Summary of operative septoplasty sequence.
26/934.6
25.7/8.9Septum to ANS fixation4645.5Maxillary crest/ANS osteotomy2221.7Spreader graft unilateral98.9Spreader graft bilateral5857.4Autospreader flap1413.8Septal rotation suture87.9Conchal cartilage graft54.9Rib cartilage graft10.99 Nasal bone OsteotomyMedial1110.8Lateral101100
Based on preoperative examination, various degrees of obstructive symptoms were noted in 32 patients. Paranasal sinus CT scan was performed in 67 patients based on obstructive symptoms (32 cases), history of nasal trauma (11 cases) or the presence of overt external nasal deviation (19 cases) and secondary operation (5 cases). 58 out of these 67 cases showed distinct nasal septal deviation (NSD) on CT scan which translates into 86.5%. The number of NSD cases in this subgroup was almost consistent with intraoperative findings (n=60 or 89.5%) (Figure 3).
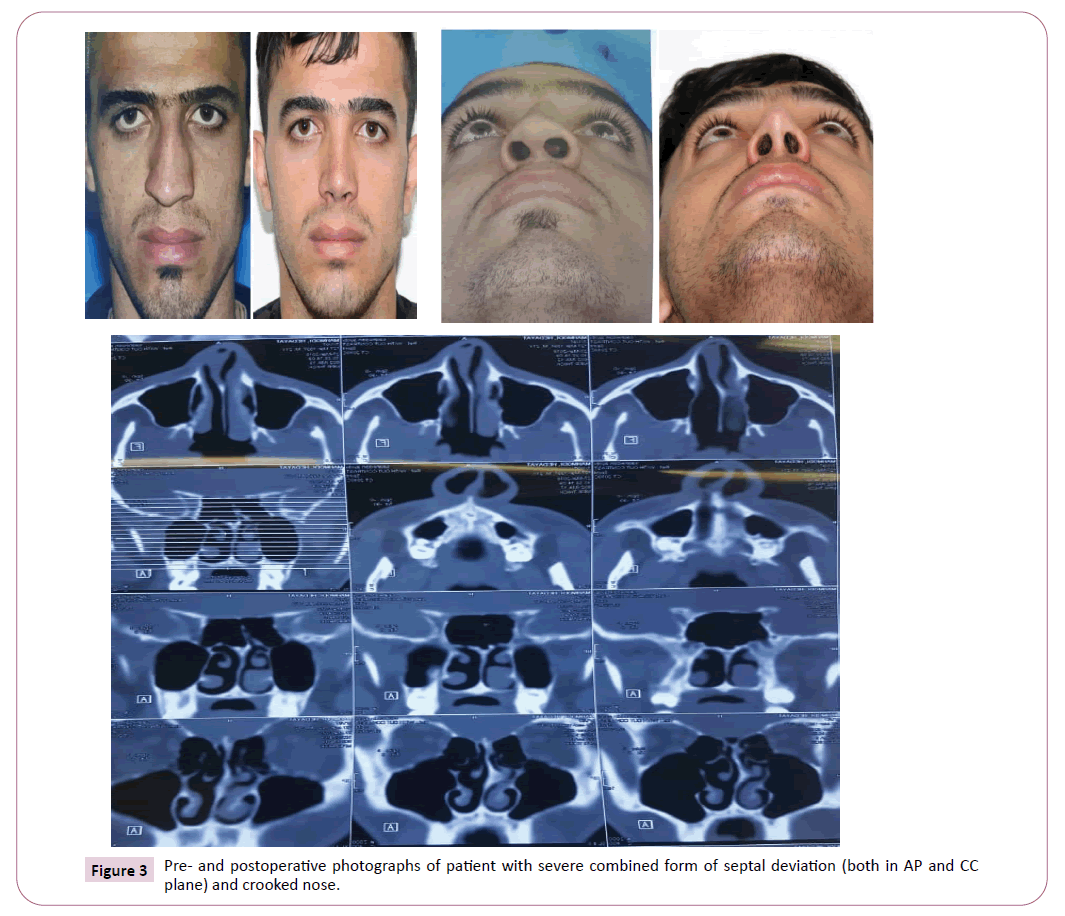
Figure 3: Pre- and postoperative photographs of patient with severe combined form of septal deviation (both in AP and CC plane) and crooked nose.
AP: Anteroposterior, CC: Craniocaudal, NSD: Nasal Septal Deviation
MLSS: Modified L-Strut Septoplasty; SG Spreader Graft; ASF Autospreader Flap
SRS Septal Rotation Suture; MC: Maxillary Crest
In remaining 34 patients without CT scans there were 11 cases which showed mild to moderate degrees of NSD (26.4%). Therefore the overall frequency of NSD was 69 cases (68.3%). The most common type of NSD was septal tilt observed in 23 patients (33.3%) with no significant structural curvature of the septum, but tilted to right side in 15 and to left side in 8 patients (according to external deformity). Major NSD types in decreasing order of frequency were C shape in anteroposterior plane (31.8%), S-shape with two opposing curves in AP plane (8.6%) followed by septal spurs and deformities in craniocaudal dimension which is summarized in Table 4.
Table 4 Frequency and main features of nasal septal deviation types along with main septoplasty techniques and differential RHINO score.
Septal Tilt 23 (33.3%) •No intrinsic septal curve but dislodgment from maxillary crest
•Most internally to left and externally to right
•Best viewed on axial CT •Closed /open
•Modified L-strut septoplasty
•Septal release/
•ANS suture fixation +38.4 P<0.001 C shaped (AP) 22 (31.8%) •Associated with vomerine plate deviation ,dorsum deviated to one side
•Most cases presenting as reverse C type pointing to the right of patient
•Best viewed on axial CT •Open
•Mod. L-strut septoplasty
•ANS/MC osteotomy
•Vertical scoring concave (unilateral )
•SG/ASF
•Septal rotation suture +28.04
P<0.001
C shaped (CC) 5 (7.2%) •C or reverse C shaped curve of the dorsum
•Best viewed on coronal CT •Open
•Mod L-strut Septoplasty
•ANS/MC osteotomy Horizontal Scoring concave
•SG /ASF +24
P=0.03 S shaped (AP) 6 (8.6%) •Two opposing curvatures in AP plane
•External deviation of dorsum to one side
•Best viewed on axial CT •Open
•L-Strut Septoplasty
•Vertical Scoring (Bilateral )
•ANS/MC osteotomy
•SG /ASF +25.5
P=0.002
S shaped (CC) 2 (2.9%) •S or reverse S- type curve in CC plane with the same curve of dorsum
•Best viewed on coronal CT •Open
•MLSS
•Horizontal Scoring (Bilateral)
•ANS/MC osteotomy
•SG /ASF) +15.5
P=0.141 Localized/Combined types 11 (15.9%) •Septal spur (localized NSD):functional
•Combined types: variable presentation •Closed /Open
•Variables +37.4
P<0.001
Although not symptomatic, maxillary sinusitis was discovered incidentally in three of CT examinations, for which the operation was deferred to after medical therapy. Concha bullosa was observed in 21 (31.3%) of the patients’ scans.
Of the 101 nasal surgeries, 8 cases (7.9%) were performed for pure functional indications, 17 cases (16.8%) for aesthetic indications, and 76 patients (75.1%) for a combination of functional and aesthetic indications. 11 patients (10.8%) had a documented history of prior nasal fracture. Most patients were primary cases with a combined functional and aesthetic indication for surgery (Table 1).
Variable forms of septoplasty/SMR was performed in 88 cases (87.1%) in a stepwise approach. Operative septoplasty technique included standard sub-mucoperichondrial dissection and a modified L-frame septoplasty which included localized spurs or wedge shaped excision of posterocaudal septum or deviated part of the septum (69% ), and septal reconstruction, septal repositioning at midline and fixation to ANS (52.1%), scoring of the L-frame on the concave side (58%) and placement of spreader grafts (76%) or auto-spreader flaps ( 13%) as necessary. Five patients underwent harvest of conchal cartilage and one of rib cartilage for grafting purposes in secondary cases. Nasal bone osteotomies and other steps were also individualized based on the type of deformities which is summarized in Table 3.
Most patients were discharged home on a day care setting and visited on 2nd and 7thpostoperative days for removal of nasal pack and splint respectively and supervised taping was continued as necessary. There were no surgical complications or readmission/ reoperation identified in the study period. At 3 months, patients were visited for post-operative photography and the final completion of the RHINO Questionnaire.
A paired samples t-test was performed comparing the averaged preoperative RHINO scores with the postoperative RHINO score, demonstrating a statistically significant increase in scores postoperatively (P<0.001). The mean preoperative averaged RHINO score was 46.2 â?? 12.3 when compared with a mean postoperative RHINO score of 75.7 ± 14.1. The difference between preoperative and postoperative scores ranged from −5 to +66, with a mean difference of 29.5 ± 16.1.
Discussion
Results of this study emphasize the importance of patient history and clinical examination in the diagnosis of nasal septal deviation (NSD). Elicitation of history of nasal trauma and obstructive symptoms combined with comprehensive examination (both external and via anterior rhinoscopy) precluded the need for further investigation including CT scans in about 95 percent of patients. Interestingly absence of obstructive symptoms did not correlate with absence of anatomic deviation, possibly because most patients had no previous point of comparison. To date numerous authors have categorized SND based on different points of view.
The first attempts to systematize septal distortions were given as early as 1958 by Cottle who defined four groups of “septal deviations”: subluxation, large spurs caudal deflection and tension septum. In 1987, Mladina of Croatia was the first to make a comprehensive classification [11,12]. He also described a seventh type, which presents a combination of some of the previous six types.
Mladina types of SD are divided into two main groups: so-called vertical deformities (Types 1, 2, 3 and 4), and horizontal ones (types 5 and 6). Vertical deformities have the longer axis in a vertical plane, i.e., they concern the unilateral crook (s) that can be imagined as a result of the force acting against the nasal septum in an antero-posterior direction. The horizontal deformities, however, have a longer axis in the horizontal plane, i.e., they are crooked as if the force against the septum has been acting from superior to inferior. This classification gained popularity mainly among otolaryngologists.
In 1999, Guyuron published his suggestions, promoting six major types which, seemed to be more user friendly than Mladina’s [13]. Guyuron suggested the following types: septal tilt, anteroposterior C, antero-posterior S, cephalo-caudal S, cephalo-caudal C, and wide spurs. This classification, as for that described by Mladina, includes six types of NSD.
Guyuron’s classification gained much more popularity among plastic surgeons worldwide. Overall, both classifications describe almost the same deformities but in “different languages”. However in this study we used Guyuron’s classification but included combined forms in the sixth group and not into a separate class.
On the other hand external nasal deformities and internal septal deviations exist symbiotically. Findings of anteroposterior C-shaped deviation correlated with an external deviation on the opposite side of the internal deviation while a cephalocaudal C-shaped deviation usually presented as a visible C-shaped external deformity. Our findings suggest that reverse C type septal deviation translating to right sided external deviation of the dorsum is the most prevalent type (after septal tilts) rather than the C type itself as reported by Guyuron and others [14-20]
From a technical viewpoint we used a modified stepwise approach to septoplasty starting with removal of only a posterocaudal wedge of the septum necessary for correction of deviation preserving as much septal cartilage as possible. This is in contrast to standard L-strut concept that leaves 10 to 15 mm of septum anteriorly and caudally and we believe our modification confers more stability to nasal framework.
After wedge excision the remainder of the posterocaudal septum is easily disengaged from the perpendicular plate, the vomerine groove, and anterior maxillary crest as needed. The deviated portion of the cartilaginous septum, vomer and perpendicular plate were removed as needed and prior to repositioning of the septum, it is imperative to ensure that the anterior nasal spine is in the midline; so osteotomy of ANS and maxillary crest must be considered. In selected cases with excision of large septal segments partial replacement of straight bone and crushed cartilage was performed and dead space closed by through and through gut sutures.
If above measures did not result in straightening the septum, L-frame was scored strategically in the opposite direction of septal curve on the concave surface. This meant vertical scoring in anteroposterior (26 cases) and horizontal scoring in cephalocaudal septal deviations (9 cases). In S shaped deviations bilateral scoring was done again on each concave side. In more refractory cases the deviated anterior septum was incrementally straightened by a septal rotation suture (8 cases) (Figure 4).
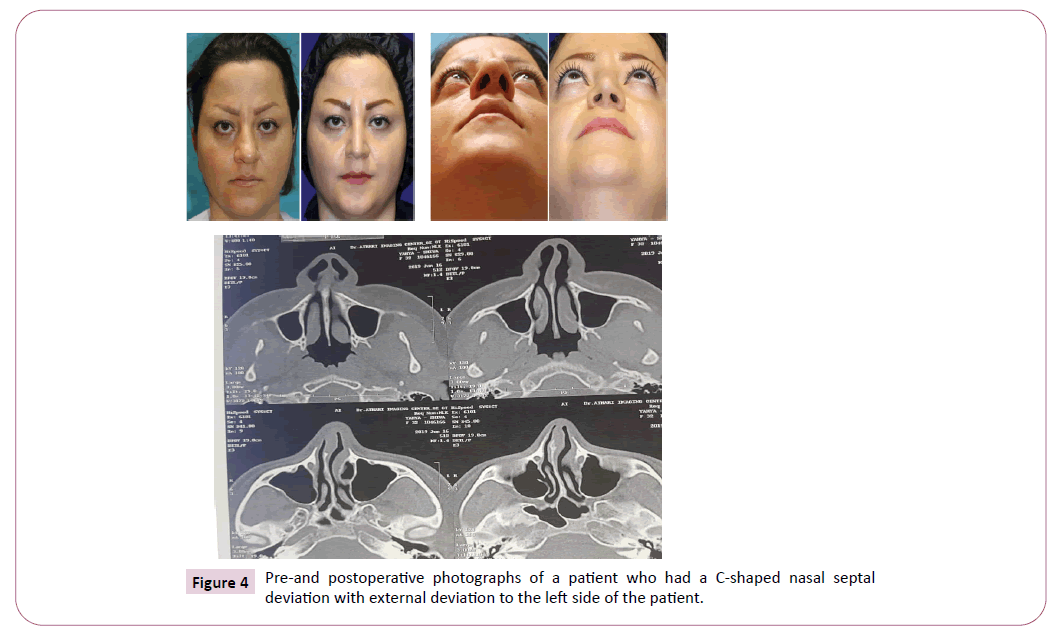
Figure 4: Pre-and postoperative photographs of a patient who had a C-shaped nasal septal deviation with external deviation to the left side of the patient.
Spreader grafts were used primarily to widen the midvault or correct the deviation or to reconstruct dorsal aesthetic lines [17-20] including 58 bilateral and 9 unilateral cases. In 14 cases, the upper lateral cartilages were used as autospreader flaps, maintaining the patency and integrity of the internal valves and restore contour of the dorsal aesthetic lines.
For correction of the external deformities it is helpful to divide the nose into thirds. Deviation of the upper third usually results from fractured nasal bones. Accurately identifying upper third deformities remains important, as correction of the septum alone typically fails to change the cosmetic appearance of the nose. Such deformities require osteotomies of the nasal bones for proper alignment and approximation of bony vault [21-25] which was performed universally in all of the studied patients (Table 3).
However, the septum influences the middle and lower thirds of the nose to a greater degree especially on the latter. When imagining the biomechanics of the nose and septum, the quadrangular cartilage acts like a ridge board on a roof with the lateral cartilages functioning as the rafters. Consequently, an unstable quadrangular cartilage leads to unstable lateral cartilages contributing to external deformity or collapse [17-20].
Regarding outcome assessment there are no standardized measures for assessing the aesthetic or functional outcomes following rhinoplasty. Various authors have proposed different methods including image analysis, measurement tools, and computer programs, to assess these outcomes [21-24].
Currently, the gold standard instrument for functional nasal surgery is the NOSE scale, as first described by Stewart et al. [7,9]. However this instrument focuses on the assessment of nasal obstructive symptoms alone, and its application is relatively limited with primarily aesthetic or combined functional/aesthetic indications. The ROE scale is a complementary quality of life instrument initially developed and validated by Alsarraf et al. [8,9] with a focus on aesthetic outcomes after nasal surgery. In this study, we have used RHINO a unified scale introduced by Lee et al. assessing both functional and aesthetic patient-reported outcomes after rhinoplasty. This instrument has demonstrated a high level of reliability and validity [9].
A distinct advantage of RHINO scale is the ability to differentiate between functional and aesthetic outcome based on the scores for relevant questions. As pointed before, the difference between preoperative and postoperative scores ranged from -5 to +66, with a mean difference of 29.5 ± 16.1 indicating a high level of satisfaction in the majority of patients. However three patients in this study expressed ambivalence regarding their surgical outcome (two patients with no change and one patient with minus 5 RHINO score after nasal surgery). Interestingly, in the latter patient when viewing the functional items in isolation, his score was increased from a preoperative average of 26 to a postoperative score of 35. However, his aesthetic score decreased from a preoperative average of 28 to a postoperative score of 14. Overall, the patient related that his improvement in nasal obstruction was counterbalanced by his disappointment with his aesthetic appearance.
Rhino score was significantly improved in all 6 types of NSD with highest degree in septal tilt (+38.4) and lowest in S shaped NSD (+15.5); although in the latter group the difference was statistically not significant (P=0.14) .
Therefore a unidimensional QOL instrument would not have revealed a comprehensive or accurate assessment of the patients´ overall self-reported outcomes and satisfaction with surgery. This again emphasizes why a unified functional and aesthetic scale is critical for the assessment of surgical outcomes after rhinoplasty [26]. Relative limitations of this study may be the sample size and limited time for follow up of enrolled patients. Also loss of personal contribution of some patients in follow up visits can compromise the results.
Conclusion
Precise knowledge regarding both internal and external patterns of nasal septal deviation is an important and integral part of any rhinoplasty procedure and has a significant impact on both the clinical outcome and patient satisfaction. A stepwise approach to diagnosis and surgical management of septal deviations is recommended in all patients presenting for aesthetic and functional rhinoplasty.
References
- Hsia JC, Camacho M, Capasso R (2014) Snoring exclusively during nasal breathing: a newly described respiratory pattern during sleep. Sleep Breathing 18: 1: 159-164.
- Higuera S, Lee EI, Cole P, Hollier LH, Stal S (2007) Nasal trauma and the deviated nose. Plast Reconstr Surg 120: 7: 64S-75S.
- Rohrich RJ, Gunter JP, Deuber MA, Adams Jr WP (2002) The deviated nose: optimizing results using a simplified clas- sification and algorithmic approach. Plast Reconstr Surg 110: 6: 1509-1523,
- Parrilla C, Artuso A, Gallus R, Galli J, Paludetti G (2013) The role of septal surgery in cosmetic rhinoplasty. Acta Otorhinolaryngol Ital 33: 3: 146-153.
- Teixeira J, Certal V, Edward T (2016) Nasal septal deviations: A systematic review of classification systems. Plast Surg Int.
- Lam DJ, James KT, Weaver EM (2006) Comparison of anatomic, physiological, and subjective measures of the nasal airway. Am J Rhinol 20: 463-470.
- Stewart MG, Witsell DL, Smith TL, Yueh B (2004) Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg 130: 157-163.
- Alsarraf R, Larrabee WF Jr, Anderson S (2001) Measuring cosmetic facial plastic surgery outcomes: a pilot study. Arch Facial Plast Surg 3: 198-201.
- Matthew KL, Most SP (2016) A comprehensive quality-of-life instrument for aesthetic and functional rhinoplasty: The RHINO Scale. Plast Reconstr Surg Glob Open 4: 2: e611.
- Guyuron B, Uzzo CD, Scull H(1999) A practical classification of septonasal deviation and an effective guide to septal surgery. Plastic and Reconstructive Surgery 104: 7: 2202-2209.
- Mladina R (1987) The role of maxillary morphology in the development of pathological septal deformities. Rhinology 25: 3: 199-205.
- Mladina R, Cuji E, Subari M, Vukovi K (2008) Nasal septal ´deformities in ear, nose, and throat patients: an internationalstudy. Am J Otolaryngol Head Neck Med Surg 29: 2: 75-82.
- Lee JW, Baker SR (2013) Correction of caudal septal deviation and deformity using nasal septal bone grafts. JAMA Facial Plast Surg 15: 2: 96-100.
- Guyuron B, Behmand RA (2003) Caudal nasal deviation. Plast Reconstr Surg 111: 2449-2457.
- Gunter JP, Rohrich RJ (1988) Management of the deviated nose: The importance of septal reconstruction. Clin Plast Surg 15: 43-55.
- Byrd HS, Salomon J, Flood J (1998) Correction of the crooked nose. Plast Reconstr Surg 102: 2148-2157.
- Hassanpour SE, Heidari A, Moosavizadeh SM, Tarahomi MR, Goljanian A, et al. (2016) Comparison of Aesthetic and Functional Outcomes of Spreader Graft and Autospreader Flap in Rhinoplasty. World J Plast Surg 5(2): 133-138.
- Constantian MB (1994) The incompetent external nasal valve: Pathophysiology and treatment in primary and secondary rhinoplasty. Plast Reconstr Surg 93: 919-931.
- Sheen JH (1984) Spreader graft: A method of reconstructing the roof of the middle nasal vault following rhinoplasty. Plast Reconstr Surg 73: 230-239.
- Chand MS, Toriumi DM, Landecker A (2007) Surgical management of the nasal airway. Quality Medical 909.
- Hilger PA, Webster RC, Hilger JA (1983) A computerized nasal analysis system. Arch Otolaryngol 109: 653-661.
- Courtiss EH, Goldwyn RM (1983) The effects of nasal surgery on airflow. Plast Reconstr Surg 72: 9-21.
- Okur E, Yildirim I, Aydogan B (2004) Outcome of surgery for crooked nose: an objective method of evaluation. Aesthetic Plast Surg 28: 203-207.
- Mojallal A, Ouyang D, Saint-Cyr M (2011) Dorsal aesthetic lines in rhinoplasty: a quantitative outcome-based assessment of the component dorsal reduction technique. Plast Reconstr Surg 128: 280-288.
- Motamed S, Saberi A, Niazi F, Molaei H (2017) Complications of Internal Continuous and Perforating External Osteotomy in Primary Rhinoplasty. World J Plast Surg 6: 2: 164-169.
- World Health Organization (1948) Constitution of the World Health Organization. Geneva: WHO, Switzerland.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences
