Management of Scar Contracture of the Fingers with Percutaneous Needle Aponeurotomy and Fat Lipofilling
Wael Naeem Thabet Aziz1, Walaa Anis Mansour1 and Mohamed Farouk2*
1Division of Plastic Surgery, Department of General Surgery, Faculty of Medicine, Cairo University, Egypt
2Department of Plastic Surgery, Faculty of Medicine, Beni Suef University, Egypt
- *Corresponding Author:
- Dr. Mohamed Farouk
Department of Plastic Surgery
Faculty of Medicine
Beni Suef University, Egypt
Tel: +96599845476
E-mail: drfarouk@hotmail.com
Received Date: July 01, 2021; Accepted Date: July 21, 2021; Published Date: July 28, 2021
Citation: Aziz WNT, Mansour WA, Farouk M (2021) Management of Scar Contracture of the Fingers with Percutaneous Needle Aponeurotomy and Fat Lipofilling. J Aesthet Reconstr Surg Vol.7 No.4:32.
Abstract
Background: Scar contractures of the fingers represent a major functional and aesthetic burden to many patients with hand injury. Managing such condition is often challenging and various techniques have been proposed, with flap-based techniques being the conventional options. Percutaneous Needle Aponeurotomy (PNA) combined with lipofilling represent a novel, non-invasive method for managing scar contractures.
Methods: This prospective study included 10 patients with scar contractures of the fingers who were managed with PNA and lipofilling at a single center from March 1st, 2015 till March 1st, 2016. Six patients had postburn scars and 4 patients had post-traumatic scarring.
Results: All patients had significant improvement in contractures postoperatively at the median follow-up, the mean improvement of contracture was 21 degrees (± 9 degrees) for the MP joint, and 31 degrees (± 12 degrees) for the PIP joint. Functional improvement was recorded in 6 out of 8 patients (75%), and cosmetic improvement was reported by 9 out of 10 patients (90%).
Conclusion: PNA with lipofilling is a novel, safe and effective means for managing scar contractures of the hand.
Keywords
Rigottomies; Post-burn scar; Scar contracture; Percutaneous needle aponeurotomy
Introduction
The hand is a crucial element for the proper functioning of an upper limb, both sensory and motor. Hand injury represents up to 10% of hospital emergency room visits [1,2]. Proper knowledge of hand anatomy and physiological function - including grips, opposition, and fine motor skills - combined with experience in physical examination of the hand is essential for appropriate management and for cutting down morbidity and disability rates [3,4].
Hand contracture constitutes a major form of disability and is defined as an inability to perform the full range of hand movement due to permanent shortening of the muscles and/or joints [5]. Scar contractures following burn injury (postburn contractures), in particular, represent a surgical dilemma that often necessitate multiple interventions and the supplementation with physical therapy [6]. Excessive scarring may involve the healing of deeper tissues after high-degree burns; this often begins as puckering but can advance to thick bands of hypertrophic scarring that may restrict or preclude joint movement and permanently impair its function [7]. Other causes of scar contractures of the hand include mechanical and chemical trauma [8].
Severity rating of postburn contracture of the hand has been proposed: grade I includes cases with symptomatic tightness but no visible anatomical changes, grade II includes cases with mild decrease in motion range, grade III includes cases with functional defects and mild change in architecture, and grade IV includes cases with severe functional defects and major architectural change [9]. The conventional primary treatment modality has long been surgical release with graft or flap coverage, with the latter including a variety of options such as split-thickness or full-thickness skin grafts, Z-plasties, cross-finger flaps, local transposition flap, radial forearm flap, ulnar artery flap, Baker’s flap, or abdominal flap [10]. Muscle, tendon, and/or joint capsule procedures may also be required [11].
Percutaneous needle aponeurotomy (PNA) has recently been popularized with the rise of non-invasive procedures for the management of contractures [12]. The technique was proven safe, effective, and cost-efficient in managing hand contractures, especially Dupuytren’s contracture [12-14]. Dupuytren’s contracture is a relatively common, bilateral proliferation of the fibrous tissue in the hand that occurs in the elderly and leads to progressive disabling contracture of the fingers - most often the ring and little fingers [15]. Recently, the use of PNA associated with lipofilling has been proposed for usage beyond Dupuytren’s contracture, such as in cases with postburn contractures of the hand [16]. The goal of the procedure is both functional rehabilitation of the affected finger by releasing the scar tissue together with cosmetic improvement through the lipofilling [17]. If proven effective, the technique would disregard the need for invasive flap reconstruction with all accompanying risks and would provide a better aesthetic outcome [16].
In this study, we examine the feasibility, efficacy, and safety of PNA and lipofilling in managing scar finger contracture.
Research Methodology
Study population
This prospective work included patients with scar contractures of the fingers presenting to our care between the periods of March 1st, 2015 till March 1st, 2016. The study adhered to the tenets of the declaration of Helsinki and no identifying information was used. Informed consent was obtained from all patients for the use of their deidentified case details in the study.
Our inclusion criteria included patients with scar contractures resulting from mechanical, chemical, or thermal trauma, limited to one hand, with 50 degrees or less of contracture in the metacarpophalangeal (MP) joint and 60 degrees or less of the proximal interphalangeal (PIP) joint, with mild to moderate limitation of motility. We excluded patients with degenerative, idiopathic, or inflammatory contractures including those with Dupuytren’s contracture, rheumatoid arthritis, thyroid disease, and other pathologies with soft tissue involvement. We also excluded patients who underwent prior surgery or were unfit for surgery such as those with absolute need for anticoagulation medication or those with debilitating general conditions.
Pre-operative preparation
All cases were subjected to detailed history taking including onset and mode of trauma and duration of deficit. Patients also underwent full clinical examination of the hand including assessment of the number of involved fingers, the surface area of affection, the identity of involved joints, the extent of contracture and extension deficit in the involved fingers using goniometry and expressed in degrees, the skin condition, the grip function and motion range and three-dimensional architectural evaluation of the involved tissue. Wherever appropriate, magnetic resonance imaging (MRI) of the hand was obtained to assess structural integrity of the tissue.
Surgical technique
All procedures were done in the operating room under local anesthesia (mix of saline, lidocaine 2%, and epinephrine 1/200,000). The procedure was conducted in line with the description of Khouri et al. [16] Initially, liposuction was carried out from the donor site (abdomen, thighs, or flanks depending on the patient’s preference of where excess fat is located) using a 12- hole cannula with suction negative pressure of 25 mmHg, after which the fat was allowed to sit and sediment. The fat aspirate is then injected at a slow rate over the defect by a fine needle with an even distribution to the point that just puts the restrictive tissue under tension. PNA is then carried out using an 18-gauge hypodermic needle. Predetermined directional nicks are made with the assistance of a skin hook to exert more tension in the third dimension. Multiple punctures (2 mm in depth each) are made with each puncture followed by an oscillatory motion to release more tissue and produce the final honeycomb pattern. Care is taken so as not to create too large gaps where fat grafts would pool and fail.
Post-operative care
Patients were discharged on the same day of the procedure with a prescription of oral antibiotics (co-amoxiclav) and an antiinflammatory and analgesic agent (ibuprofen 600 mg 3 times/ day). They were instructed to keep the hand elevated during the initial 48 hours after the surgery and to avoid any excessive gripping or hand-soiling procedures. Patients were followed up on the first week, first month, and 6th month following the procedure. The primary outcome measured was improvement in the degree of contracture for the joints of the finger. Secondary outcomes included cosmetic appearance, functional improvement, and complication rates.
Results
Our study included 10 patients with scar contracture of the fingers. Sjx of the participants (60%) were males and 4 (40%) were females. All our patients were middle aged, the mean (± SD) of the patients was 31.5 (± 12.6) years, with a range of 17- 51 years. Table 1 demonstrates the demographic and clinical characteristics of our patient group.
| Variables | N=10 | |
|---|---|---|
| Age (years) | Mean ñ SD | 31.5 ñ 12.6 |
| Range | 17 - 51 | |
| Gender | ||
| Male | n (%) | 6 (60) |
| Female | n (%) | 4 (40) |
| Occupation | ||
| Laborer | n (%) | 3 (30) |
| Housewife | n (%) | 3 (30) |
| Student | n (%) | 2 (20) |
| Mechanic | n (%) | 1 (10) |
| Unemployed | n (%) | 1 (10) |
| Hand Affected | ||
| Dominant | n (%) | 7 (70) |
| Non-dominant | n (%) | 3 (30) |
| Mode of Injury | ||
| Burn | n (%) | 6 (60) |
| Mechanical | n (%) | 4 (40) |
Table 1: Major demographic and clinical characteristics of our patient group (n=10).
The mode of injury was a burn in 6 (60%) of the patients and mechanical trauma in 4 (40%) of the patients. All the patients with mechanical trauma were males. All patients were medically free. The dominant hand was affected in 7 patients (70%) while the non-dominant hand was affected in 3 patients (30%). The duration from the onset of injury till presentation to our care ranged from 4 to 26 months (median 10 months).
All patients in our cohort had only one hand affected, with 6 patients (60%) having two fingers affected, 2 patients (20%) having one finger affected, and 2 patients (20%) having three fingers affected. The little finger was affected in 6 patients (60%), the ring finger in 5 patients (50%), the middle finger in 2 patients (20%), and the index finger in 2 patients (20%). The MP joint was affected in all ten patients (100%), and the PIP joint was affected in 6 patients (60%). The mean degree of contracture of the MP joint measured by goniotomy was 45 degrees (± 18 degrees), while that of the PIP joint was 58 degrees (± 28 degrees). Functional impairment of the hand was recorded in 8 patients (80%), and cosmetic dissatisfaction was reported by all patients (100%). Table 2 demonstrates the preoperative characteristics of the patients.
| Variable | N=10 | |
|---|---|---|
| Laterality | ||
| Unilateral | n (%) | 10 (100) |
| Bilateral | n (%) | 0 (0) |
| Number of Fingers | ||
| One | n (%) | 2 (20) |
| Two | n (%) | 6 (60) |
| Three | n (%) | 2 (20) |
| Finger Affected | ||
| Little | n (%) | 6 (60) |
| Ring | n (%) | 5 (50) |
| Middle | n (%) | 2 (20) |
| Index | n (%) | 2 (20) |
| Degree of Contracture | ||
| MP Joint | Mean (ñ SD) | 45 (ñ 18) |
| Range | 25 - 65 | |
| PIP | Mean (ñ SD) | 68 (ñ 28) |
| Range | 45 - 90 | |
Table 2: Pre-operative characteristics of the patients (n=10).
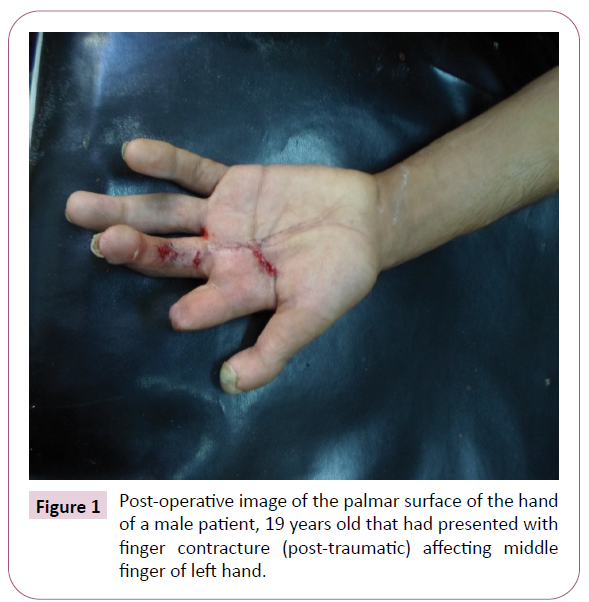
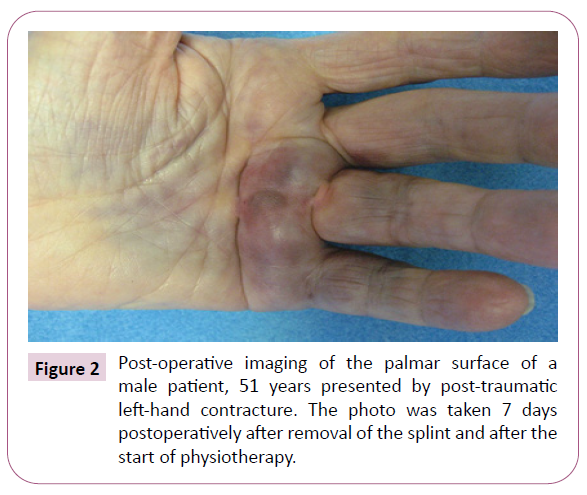
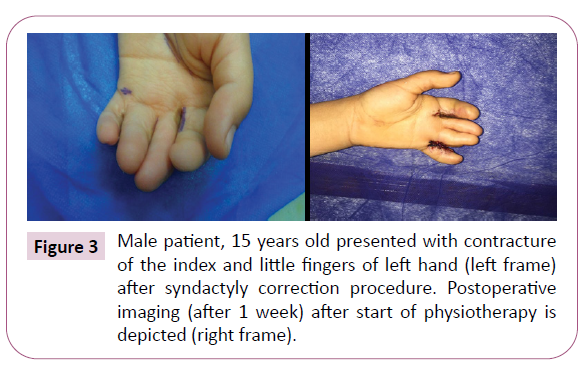
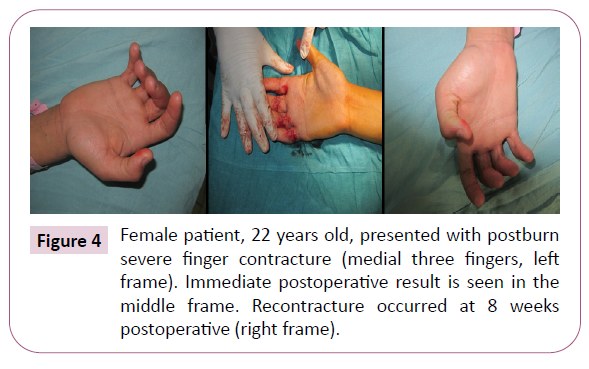
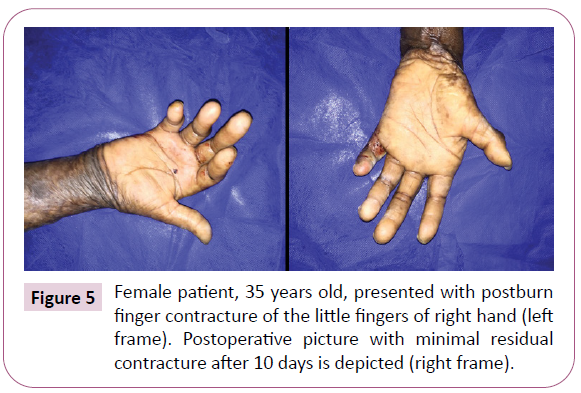
The mean duration of the procedure was 42.3 minutes (SD ± 17.6 minutes). No intraoperative complications were noticed in any of the patients. Figures 1-5 demonstrates some preoperative and postoperative imaging of a sample of our patient group. The median follow-up interval was 3 months (range: 2-6 months). At the median follow-up mark point, the mean improvement of contracture was 21 degrees (± 9 degrees) for the MP joint and 31 degrees (± 12 degrees) for the PIP joint. Functional improvement was recorded in 6 out of 8 patients (75%), and cosmetic improvement was reported by 9 out of 10 patients (90%).
Regarding postoperative complications, hematoma was seen in 3 patients (30%), and re-contracture occurred in 4 patients (40%), with a mean onset of 11 weeks postoperatively. We encountered no cases of postoperative infection.
Discussion
In this work, we describe our experience with PNA and lipofilling in managing scar contractures of the fingers. We report excellent results with significant improvement in contracture degree, cosmetic improvement, and functional gain in most of our patients. The technique also proved safe with minimal complications reported.
Our results are comparable to those of previous studies. Badois et al. [18] originally described needle fasciotomy for the management of Dupuytren’s contracture. They reported no major complications with the procedure, with only a skin break occurring in 16% of the patients. Von Pess et al. [19] recently reported results of the largest cohort of finger contracture patients that underwent PNA, with an immediate postoperative correction of 99% in the MP joint and 89% in the PIP joint. Our population group differs than that of the Dupuytren’s contracture group, with the latter affecting the elderly population. Limited studies are available describing PNA with or without lipofilling in scar contractures of the fingers. Khouri et al. [16] reported their experience in managing scar contractures of different body sites in 31 patients using PNA with lipofilling. The technique was optimal for managing the condition with minimal complications. Wider meshed areas had more successful tissue gain. Our study is, however, novel in describing experience with PNA and lipofilling with limitation to scar contractures of the hand. The only drawback that could be perceived regarding the procedure in our patient group was re-contracture. Re-contracture is a major issue to all interventions for scar contractures described in the literature, with occurring rates of up to 90%.
Conclusion
In our experience, only 40% of the patients experienced recontracture. Being easy to do and with a low cost, re-operating in those patients using the same technique is feasible with excellent expected outcomes. Strength to our work is the prospective study design. Limitations to our work include the small sample size and the non-comparative nature of the study. It would be useful for future studies to compare flap-based technique to PNA with lipofilling regarding contracture improvement, complication rates, cost, duration of recovery, and cosmetic improvement. In conclusion, PNA with lipofilling is a safe and effective means for managing scar contractures of the hand.
References
- Larsen CF, Mulder S, Johansen AMT, Stam C (2004) The epidemiology of hand injuries in The Netherlands and Denmark. Eur J Epidemiol 19: 323-327.
- Trybus M, Lorkowski J, Brongel L, Hľadki W (2006) Causes and consequences of hand injuries. Am J Surg 192: 52-57.
- Neumeister MW, Brown RE (2003) Mutilating hand injuries: Principles and management. Hand Clin 19: 1-15.
- Sorock GS, Lombardi DA, Hauser RB, Eisen EA, Herrick RF, et al. (2002) Acute traumatic occupational hand injuries: type, location, and severity. J Occup Environ Med 44: 345-351.
- Clavet H, Hébert PC, Fergusson D, Doucette S, Trudel G (2008) Joint contracture following prolonged stay in the intensive care unit. Can Med Assoc J 178: 691-697.
- Goel A, Shrivastava P (2010) Post-burn scars and scar contractures. Indian J Plast Surg 43: S63-S71.
- Fufa DT, Chuang SS, Yang JY (2014) Post-burn contractures of the hand. J Hand Surg Am 39: 1869-1876.
- Hegge T, Henderson M, Amalfi A, Bueno RA, Neumeister MW (2011) Scar contractures of the hand. Clin Plast Surg 38: 591-606.
- Brown M, Chung KC (2017) Post-burn contractures of the hand. Hand Clin 33: 317-331.
- Sunil NP, Ahmed F, Jash PK, Gupta M, Suba S (2015) Study on surgical management of post burn hand deformities. J Clin Diagn Res 9: PC06-PC10.
- Saleh Y, El-Shazly M, Adly S, El-Oteify M (2008) Different surgical reconstruction modalities of the post-burn mutilated hand based on a prospective review of a cohort of patients. Ann Burns Fire Disasters 21: 81-89.
- Herrera FA, Benhaim P, Suliman A, Roostaeian J, Azari K, et al. (2013) Cost comparison of open fasciectomy versus percutaneous needle aponeurotomy for treatment of Dupuytren contracture. Ann Plast Surg 70: 454-456.
- Foucher G, Medina J, Navarro R (2003) Percutaneous needle aponeurotomy: Complications and results. J Hand Surg Am 28: 427-431.
- Cheng HS, Hung LK, Tse WL, Ho PC (2008) Needle aponeurotomy for Dupuytren’s contracture. J Orthop Surg 16: 88-90.
- Townley WA, Baker R, Sheppard N, Grobbelaar AO (2006) Dupuytren’s contracture unfolded. Bmj 332: 397-400.
- Khouri RK, Smit JM, Cardoso E, Pallua N, Lantieri L, et al. (2013) Percutaneous aponeurotomy and lipofilling: a regenerative alternative to flap reconstruction? Plast Reconstr Surg 132: 1280-1290.
- Khansa I, Harrison B, Janis JE (2016) Evidence-based scar management: how to improve results with technique and technology. Plast Reconstr Surg 138: 165S-178S.
- Badois FJ, Lermusiaux JL, Masse C, Kuntz D (1993) Non-surgical treatment of Dupuytren disease using needle fasciotomy. Rev du Rhum 60: 808-813.
- Pess GM, Pess RM, Pess RA (2012) Results of needle aponeurotomy for Dupuytren contracture in over 1,000 fingers. J Hand Surg Am 37: 651-656.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences