The Safety and Efficacy of Helium-Based Plasma for Cutaneous Resurfacing and Subdermal Tightening
Keith Sweitzer1*, Zaidal Obagi2, Tia Rahman2, Peter F. Koltz3 and Frank Barone4
1Division of Plastic and Reconstructive Surgery, University of Rochester, Rochester, New York, USA
2College of Medicine and Life Sciences, University of Toledo, Toledo, Ohio, USA
3Cosmetic and Reconstructive Plastic Surgery Unit, St. Luke’s Hospital, Toledo, Ohio, USA
4Evolv Plastic Surgery & Aesthetics, Toledo, Ohio, USA
- *Corresponding Author:
- Dr. Keith Sweitzer, MD
Department of Surgery
University of Rochester
601 Elmwood Ave. Rochester, NY 14642, USA
E-mail: Keithsweitzer6@gmail.com
Received Date: August 09, 2021; Accepted Date: September 01, 2021; Published Date: September 08, 2021
Citation: Sweitzer K, Obagi Z, Rahman T, Koltz PF, Barone F (2021) The Safety and Efficacy of Helium-Based Plasma for Cutaneous Resurfacing and Subdermal Tightening. J Aesthet Reconstr Surg Vol.7 No.5:40.
Abstract
Background: Helium gas passed through an electrically-charged retractable surgical blade creates cold-atmospheric plasma, which produces a precise, instantaneous thermal and electrophysiological effect involving rapid tissue heating and cooling. Such surgical devices have already been approved by the FDA for cutting, coagulation and ablation. They have also been studied for use on cutaneous diseases, such as superficial carcinomas and rhinophymas, due to their significant tissue-modifying effects. We present a case series using a helium laser for off-label use in skin rejuvenation and deep tissue contraction.
Objectives: The primary objective was to test the capability of a helium-based plasma device as a facial resurfacing tool and to document its beneficial and adverse effects.
Methods: Four patients of Fitzpatrick Skin Types II and III underwent facial resurfacing using a helium-based plasma device (Renuvion®) under either p.o sedation or general anesthesia. Platelet-rich plasma (PRP) was applied to three of the four patients after the procedure. Nanofat/fat injection was additionally performed on two of the patients (one with and one without PRP) during the procedure.
Results: Effective and deep skin rejuvenation was achieved using the helium device in all four patients. Deep rhytid effacement, pigment correction, and cutaneous tightening was dramatic and, in our experience, superior to comparable procedures, such as CO2 lasers or chemical peels. Skin tightening and elasticity improvement is most likely a result of subdermal and deep dermal remodeling from helium’s unique effects on dermal fibroblasts. Prolonged erythema was the most commonly seen complication.
Conclusion: We found helium-based facial resurfacing to be a safe and effective method for skin rejuvenation and deep tissue contraction. Further analysis with a larger power and continued long-term follow-up, alongside studies further investigating the mechanisms of ionized helium and prevention of prolonged erythema, are ongoing.
Keywords
Subdermal tightening; Helium plasma; Resurfacing
Introduction
Facial rhytids, tissue laxity, and cutaneous surface damage are among the key signs of aging, and are often the targets of facial resurfacing procedures. Although mechanical, chemical, and energy-based technologies have been utilized in the past for skin rejuvenation, developing a resurfacing technology that effectively and safely treats deeper facial rhytids and more severe photoaging has been problematic due to potential complications such as unwanted deep or adjacent tissue thermal injury and potential wound healing complications. To decrease this thermal spread, we used an off-label device that combines heliumbased plasma with a monopolar radiofrequency signal, causing an instantaneous heating and near-simultaneous cooling effect, greatly reducing thermal spread within tissue compared to traditional CO2-based lasers.
By providing precise energy delivery, the risks of adjacent tissue thermal injury are decreased. Additionally, unlike various other laser techniques that target chromophores such as water, hemoglobin, or melanin to achieve their specific therapeutic effects, helium-based energy is not chromophore-dependent, thereby overcoming many limits of patient selection [1].
Case Series
We present four cases of facial resurfacing utilizing the Renuvion® device (Apyx Medical Corporation). While helium-based technology is FDA-cleared for cutting, coagulation and ablation of soft tissue, skin resurfacing and subdermal tissue contraction are considered off-label uses.
The Renuvion® Device
The Renuvion system utilizes a unique plasma energy technology that passes inert helium gas through an acrylic perspex tube containing an electrically charged needle and retractable surgical blade. A 2mm-diameter microplasma is then created when radiofrequency (RF) current is applied to the needle in the presence of the helium gas and air. The plasma energy produced is considered ‘cold’ atmospheric plasma or non-thermal plasma because only a small percentage (0.1%) of the helium gas is ionized unlike ‘thermal’ plasmas created from other gases which require higher currents for ionization and result in significantly higher plasma temperatures. The cold atmospheric plasma produced by the helium-based plasma laser results in a precise and instantaneous dual thermal and electrophysiologic effect with rapid tissue heating and cooling. This unique system consists of an electrosurgical generator unit, an attached pressurized helium tank as the gas source, and a handpiece, with a retractable blade and a hand or foot pedal activator. The handpiece blade, which can be extended for electrosurgical cutting with very minimal tissue thermal effect, was used in the retracted position for the controlled ablation and coagulation in this resurfacing study.
The generator is used to control the helium gas flow rate and the amount of electrical RF energy (power) independently. An optional pulse mode is available, although it was not used in the treatments of the patients in this report. For the patients undergoing facial resurfacing in this series, helium flow was set at either 3 or 4 L/min and power settings were utilized at 20%, 30%, or 40% depending on the area being treated, the extent of skin damage, and subsequent treatment plan.
Methods
Patient selection
The four patients in this case report were in good health and without active medical problems or history of any active dermatological condition or treatment. None of the patients had a recent history of any resurfacing procedure or treatment. The patients in this report had either Fitzpatrick Type II or III as determined by history and examination, but they were not explicitly selected for this criterion as plasma laser energy transfer is not dependent on chromophores. However, all four patients were interested in reducing generalized signs of cutaneous photoaging, including facial rhytids, laxity, dyschromia, and solar actinic damage.
Clinical protocol
Patients #1 and #2 were treated in an office facility with oral sedation and local anesthetics with tumescent infiltration. Patients #3 and #4 received treatment at a credentialed outpatient surgical facility under general anesthesia due to plans of simultaneous fat harvesting and grafting in addition to heliumbased plasma resurfacing.
Patients 1 and 2
A 67- year and 53-year old females
Upon arrival at the office one hour prior to treatment, patients were given oral sedation (Percocet 10mg/Valium 10mg). The surgical site was then cleaned with Hibiclens® antiseptic solution. Facial nerve blocks were performed. Facial resurfacing was performed in aesthetic unit patterns. A forced air chiller and smoke evacuator were utilized at all times during treatment. The generator was set as follows: helium gas flow at 3L or 4L/ min, and power setting at 20%, 30%, or 40%. Power settings depended on the area of skin involved, the treatment plan, and the severity of rhytids or skin solar damage and elastosis: 20% for eyelids, periphery and lip vermilion, 30% for central face, cheeks, forehead, and earlobes, 40% for perioral, nose, or deep rhytids/ damage. Deeper rhytids and more problematic areas were treated with two to three passes of the laser, or until the targets were visibly effaced.
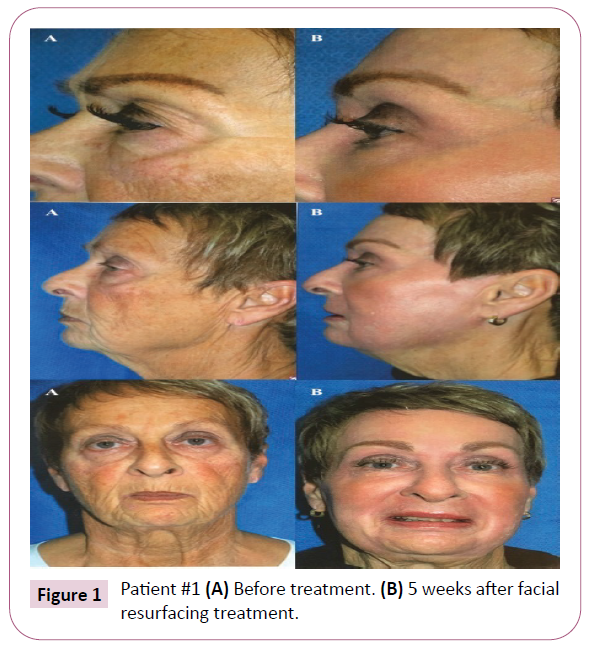
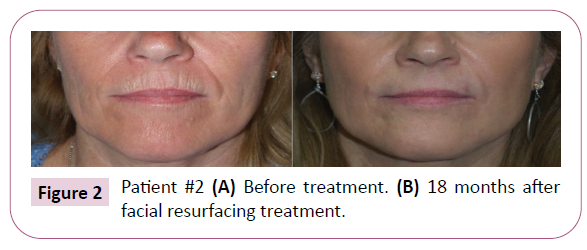
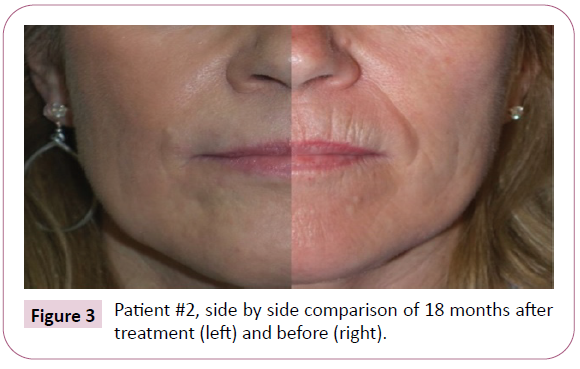
High density (4-5X) platelet-rich plasma (PRP) was applied topically as well as injected intradermally once the treatment was finished. Chilled slurry of copper peptide complex mixed with viscous 4% lidocaine was applied topically for any post-treatment discomfort. A polyurethane semi-occlusive adhesive mask was then applied to all areas treated except the eyes, nostrils, and mouth and was left in place for three to four days. Bacitracin ointment was applied to any exposed areas, and continuous ice compresses for 48-72 hours was recommended to patients. Each patient’s results are displayed in Figures 1, 2 and 3.
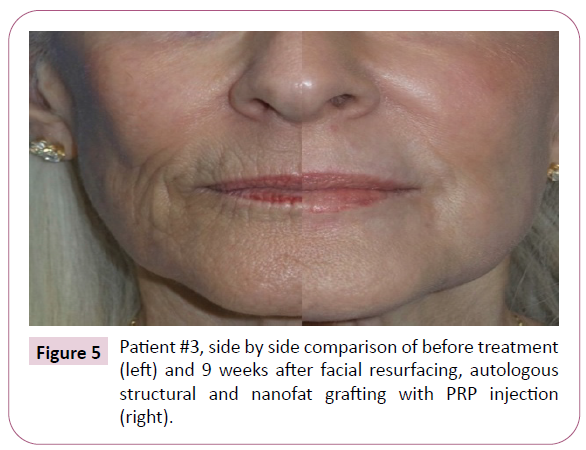
Patient 3
A 74-year-old female
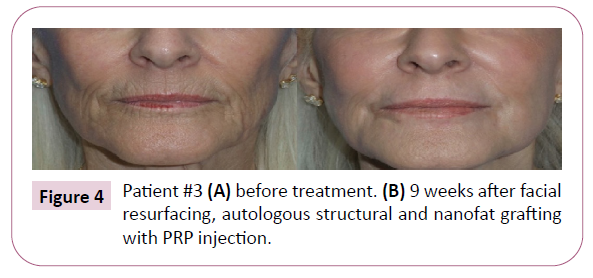
Methods were performed exactly as above except for the use of general anesthesia without nerve block. Similar plasma settings were used except for one additional pass was done at 80% for particularly deep perioral rhytids. Fat was harvested from posterior lateral thigh and abdomen with low-energy ultrasonic liposuction at 40% variable settings with tumescent fluid (25 cc 1% lidocaine and 1:1,000,000 epinephrine in one-liter Ringer’s lactate) and low aspiration pressure (13-14 mmHg). One half of the harvested fat, approximately 50 cc, was processed with collagenase to obtain a cellular stromal vascular fraction (cSVF) to enrich fat grafts. The cSVF and high density (4-5X) PRP were combined with 60cc of structural fat grafts for panfacial volume augmentation. Approximately 20 cc of PRP-enriched nanofat (Nanotransfer™ Generation I) stem cell enrichment was injected intradermally to perioral area, forehead, lateral eyelids, and forehead rhytids [2]. Results in Patient 3 are demonstrated in Figures 4 and 5.
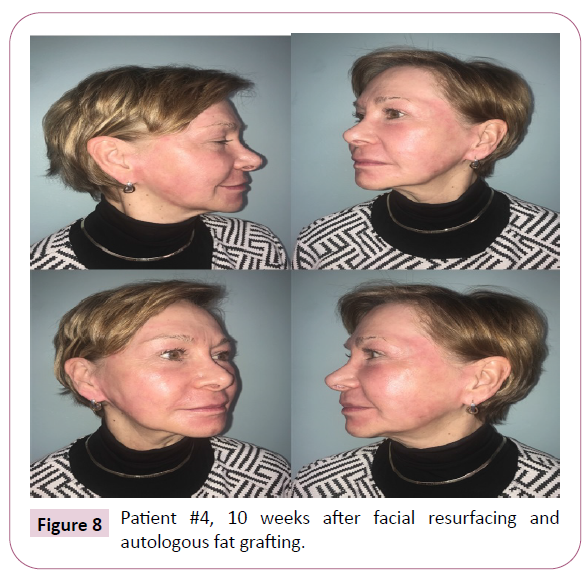
Patient 4
A 65-year-old female
After induction of general anesthesia, tumescent solution containing 25cc of 1% lidocaine with 1:100,000 epinephrine in 1000 cc of normal saline was infiltrated into the subcutaneous tissues of the intended treatment area of the abdomen. A 4mm exploded tip basket cannula was used to harvest fat, which was first transferred to Telfa and abdominal (ABD) pads for processing. The processed fat was then transferred to 3 cc syringes for fat injection. Stab incisions were made at the nasal vestibule just inside the nostrils, the oral commissures, the orbital rims, and temporal regions, all bilaterally. Panfacial fat grafting was distributed based on tissue volume needs.
Attention was then directed to resurfacing of the facial skin. The upper and lower eyelids were addressed with one pass of the plasma device 20% power with 2 liters of helium gas flow. The forehead, nose, cheeks, and lower-third of the face down to the mandibular border were treated at 30% power with 3 liters of flow. The perioral region and its deeper rhytids were treated at 40% power with 4 liters of flow. A second pass around the mouth at 20% power and 2 liters of flow was done until tissue response was deemed sufficient. After cleaning the skin, a polyurethane mask was customized to fit the patient, and a mildly-compressive netting was applied over the dressing. Patient 4’s results are exhibited in Figures 6-8.
Results
Plasma, as the fourth state of matter, has demonstrated multiple unique mechanisms to exert its effects on cells. Laroussi discusses how medical plasmas operate in the “goldilocks” range of temperature, hot enough to make reactive oxygen species (ROS) out of gaseous states which then cause downstream signaling effects, but cool enough to leave tissue unharmed. By rapidly heating the tissues, thermal damage secondary to slower heating processes, such as with traditional lasers, is reduced with the use of helium plasma technology [3]. The level of ROS generated intracellularly by plasma is not believed to reach a threshold high enough to cause apoptosis or membrane damage in normal tissues, but high enough to trigger such cytokinestimulating signaling cascades [4,5]. Helium plasma has been shown to accelerate the multiplication of certain cells in vitro by increasing extracellular levels of the cytokines PPARγ and IL-6 [6-8]. Of significance, IL-6 is a cytokine involved in cell migration and tissue regeneration, while PPARγ promotes an antiinflammatory pathway to modulate fibroblastic activity. From its cytokine-activating effects, helium-induced plasma was noted to upregulate myofibroblasts, which secrete collagen and contract, actions that both promote wound healing and skin tightening [4,5]. We hypothesize that helium-generated plasma’s effects on fibroblasts and growth factors contribute to the observed resurfacing benefits.
While the effects of ROS activation on fibroblasts, causing contracture, can take days-to-weeks to observe the full response, the thermal component of helium resurfacing provides nearinstantaneous contraction of collagen in the dermis and its fibroseptal network, leading to immediately visualized results [9]. Studies have shown that the triple-helical structure of collagen first enters a transitional state followed by a denatured formation as it is subjected to rising temperatures, with the average collagen fiber contracting and shrinking about 65% when denatured [9-11]. This device heats tissues to temperatures of 85° to 90°C within 0.04 to 0.08 seconds, which results in immediate denaturization and significant collagen contraction, without unnecessarily heating the full thickness of the dermis or damaging surrounding tissues [9,11,12].
Discussion
In our case series, we demonstrated effective use of heliumbased plasma for facial resurfacing. Using a single procedure, patients achieved dramatic recovery in the areas of cutaneous surface damage and soft tissue laxity, two key signs of aging. This is an alternative resurfacing treatment option that allows for deep dermal penetration with a strong safety profile relating to pigmentary or scarring changes in the skin. Particularly notable improvement in the periorbital, perioral, and forehead areas with dramatic reduction in rhytids and correction of pigmentation were observed in our cohort. As stated previously, it is worth mentioning that plasma lasers are chromophore-independent – in other words, they do not depend on particular particles for energy conversion. When comparing this to other laser techniques, such as CO2 lasers which target water as its main chromophore, plasma lasers are able to distribute its energy in a more uniform manner within the target dermal area. This property is beneficial for localizing therapy with more thermal control while minimizing destruction associated with chromophore mediation [1].
It was noted in all our cases that patients had post-operational erythema lasting a week longer on average compared to deep resurfacing using CO2 lasers [13,14]. We believe this is due to the increased inflammation created by the fibroblast and tissue response to helium-s timulated intracellular ROS. Immediate tissue contraction secondary to the thermal response of collagen was seen, and patients were followed for up to four years, one of whom shows that the effects are maintained long-term, and no skin cancers or skin breakdown was noted throughout this time. In our experience, the immediate application of the semi-occlusive polyurethane mask after treatment was extremely effective in reducing discomfort, providing initial wound protection, and minimizing dressing changes for the patient. Furthermore, the postoperative erythema was concealable with makeup after 2-3 weeks and resolved entirely within 2-3 months. All four of our patients displayed immense satisfaction with their results.
Conclusion
We believe helium-based plasma, in addition to its other offlabel potential in subdermal tissue contraction, can be used as an extremely effective facial resurfacing option for appropriately selected and prepared patients. Through the unique effects of helium-based plasma and RF on collagen and intracellular signaling, the small zone of injury caused by the plasma reduces unintended thermal damage of surrounding tissues. Moreover, the contraction of underlying skin and soft tissue, as well as comprehensive improvement in photoaging, was observed in our series that exceeds the effects of other current resurfacing procedures in our experience. Future, larger studies investigating the exact helium plasma-RF cellular interaction and designing improved wound care to address post-treatment erythema are currently ongoing.
References
- Janik JP, Markus, JL, Al-Dujaili Z, Markus RF (2007) Laser resurfacing. Semin Plast Surg 21: 139-146.
- Bi HS, Zhang C, Nie FF, Pan BL, Xiao E (2018) Basic and clinical evidence of an alternative method to produce vivo nanofat. Chin Med J 131: 588-593.
- Laroussi M (2009) Low temperature plasmas for medicine. IEEE Trans Plasma Sci 37: 714-725.
- Brun P, Pathak S, Castagliuolo I, Palù G, Brun P, et al. (2014) Helium generated cold plasma finely regulates activation of Human fibroblast-like primary cells. PLoS ONE 9: e104397.
- Kapadia R, Yi JH, Vemuganti R (2008) Mechanisms of anti-inflammatory and neuroprotective actions of PPAR-gamma agonists. Front Biosci 13: 1813-1826.
- Chen SS, Wright NT, Humphrey JD (1997) Heat-induced changes in the mechanics of a collagenous tissue: Isothermal free shrinkage. J Biomech Eng 119: 372-378.
- Wirtz M, Stoffels I, Dissemond J, Schadendorf D, Rosesch A (2018) Actinic keratoses treated with cold atmospheric plasma. J Eur Acad Dermatol Venereol 32: e37-e39.
- Wende K, Bekeschus S, Schmidt A (2016) Risk assessment of a cold argon plasma jet in respect to its mutagenicity. Mutat Res/Genet Toxicol Environ Mutagen 798-799:48-54.
- Duncan DI (2019) Helium plasma-driven radiofrequency in body contouring. In: Salgado AA (ed). The Art of Body Contouring. Intech Open.
- Huang G, Li F, Zhao X, Ma Y, Li Y, et al. (2017) Functional and biomimetic materials for engineering of the three-dimensional cell microenvironment. Chem Rev 117: 12764-12850.
- Arunachalam SP, Rossman PJ, Arani A, Lake DS, Glaser KJ, et al. (2017) Quantitative 3D magnetic resonance elastography: Comparison with dynamic mechanical analysis. Magn Reson Med 77: 1184-1192.
- Paul M, Mulholland RS (2009) A new approach for adipose tissue treatment and body contouring using radiofrequency-assisted liposuction. Aesthetic Plast Surg 33: 687-694.
- Sarnoff D, Gotkin H, Doerfler B (2018) The safety of laser skin resurfacing with the microablative carbon dioxide laser and review of the literature. J Drugs Dermatol 17: 1157-1162.
- Trelles MA, Mordon S, Svaasand LO, Mellor TK, Rigau J, et al. (1998) The origin and role of erythema after carbon dioxide laser resurfacing. A clinical and histological study. Dermatol Surg 24: 25-29.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences