Treatment of Malar Festoons by a Multifactorial Surgical Approach
1Department of Ophthalmology, Philadelphia College of Osteopathic Medicine, Philadelphia, PA
2Department of Oculoplastic & Orbital Surgery Wills Eye Hospital, Philadelphia, PA
3Department of Ophthalmology, Lankenau Medical Center, Wynnewood, PA
- *Corresponding Author:
- Dr. Brian M. Smith
Department of Ophthalmology
Philadelphia College of Osteopathic Medicine
4190 City Avenue, Philadelphia, PA 19131.
E-mail: briansm@pcom.edu
Received Date: October 28, 2021; Accepted Date: November 12, 2021; Published Date: November 19, 2021
Citation: Smith BM, Bonaffini SG, Chatha U, Carrasco J (2021) Treatment of Malar Festoons by a Multifactorial Surgical Approach. J Aesthet Reconstr Surg Vol.7 No.6:44.
Abstract
Background: Periorbital changes are one of the earliest detectable signs of aging. Malar pathology with chronic edema, redundant skin and orbicularis, commonly described as festoons can present alongside a variety of lower eyelid pathology. Festoons present a challenge as they can exacerbate existing lower eyelid pathology and often recur after surgical treatment. The treatment of festoons thus must be multifaceted and address both the periorbital area and mid-face.
Objective: The authors report a case series of their approach for the surgical treatment of festoons by lower lid tightening, direct compression, and excision of the affected malar region. This rejuvenates the midface by minimizing tension and reducing downward forces on the lower eyelid while restoring a smooth contour from the lower eyelid to the cheek.
Methods: Twelve eyes of six patients with festoons were treated with lower lid tightening, direct compression, and direct excision of the affected malar region.
Results: All patients had successful results with this multifactorial surgical approach to affected malar region without any major complications. Patient and surgeon were satisfied with the results with minimal to no visible scar.
Conclusion: Our case series suggests that lower lid tightening, direct compression, and direct excision of the affected malar region is an effective, predictable, and safe therapy.
Keywords
Festoon; Malar; Direct excision; Mid-face; Lower eyelid; Multifactorial; Cosmetic; Aesthetic; Rejuvenation; Oculoplastic
Introduction
Periorbital rejuvenation is amongst the most commonly requested aesthetic procedures due to its early detection and onset in the third decade of life [1-3]. Malar pathology with chronic edema, redundant skin and orbicularis muscle, and festoons often presents concurrently and can present with a variety of lower eyelid pathology such as lid retraction and ectropion. Festoons are cascading redundancy of lax skin and orbicularis muscle below the infraorbital rim in the malar region that may or may not contain ptotic or herniated fat and edema [2]. Malar mounds are different from festoons and not the subject of this article. Severe festoons can cause difficulty with near vision tasks due to visual field obscuration on downgaze and decrease self-confidence by conveying an exhausted appearance [3]. Malar festoons often present a persistent challenge for surgeons due to their diverse pathophysiology, variability in severity, and rate of recurrence, which has led to difficulty in developing a universal surgical standard in the treatment of malar festoons.
Although in many ways beneficial, the development of minimally invasive techniques to address the malar region has further complicated the management of festoons. However, surgical management still remains the gold standard for severe festoons despite no universal gold-standard surgical technique for all patients. Due to the varying severity of pathology in each patient, the surgical approach is often personalized. Techniques such as blepharoplasty, direct excision, and midface lifts are commonly utilized to restore a graceful appearance to the periorbital and malar regions in the surgical management of malar festoons [1-7].
Given the diverse pathophysiology that contributes to malar festoons, a multifactorial surgical approach that addresses the varying degrees of pathology in both the periorbital and malar regions should generate a lasting and successful aesthetic rejuvenation. A novel technique that leads to an effective, predictable, and safe therapy for such a complex clinical challenge would generate better outcomes for patients requesting periorbital rejuvenation and lead to a more universally accepted surgical treatment for malar festoons. The authors report the results of a case series of their successful approach to the surgical treatment of malar festoons through a multifaceted technique of lower lid tightening, direct compression, and excision of the affected malar region.
Methods
Lower lid tightening, direct compression and excision of the affected malar region is indicated in patients with festoons which cannot be treated with minimally invasive techniques or lower lid tightening alone. Patients who exhibit descent of the midface, including malar flatness, festoons or malar bags, elongation of the lower eyelid skin, concomitant ptosis of the fat pad are ideal candidates for this procedure.
Twelve eyes of six consecutive patients presenting with bilateral festoons and lower lid abnormalities underwent a multifactorial surgical approach for the correction of their malar pathology from July 2017 to October 2020. Lower lid tightening, direct compression and direct excision of the affected malar region were performed in the same surgical setting for all patients. The patient population consisted of four Caucasian males and two Caucasian females and ranged in age from 53 to 84 years of age. The average patient age was 66.5 years of age. All patients gave informed consent for periorbital rejuvenation surgery and written consent was provided, by which patients agreed to the use and analysis of their data and photographs for this study. Institutional review board approval was not indicated due to the retrospective nature of the case series. All procedures followed were conducted in accordance with the Declaration of Helsinki.
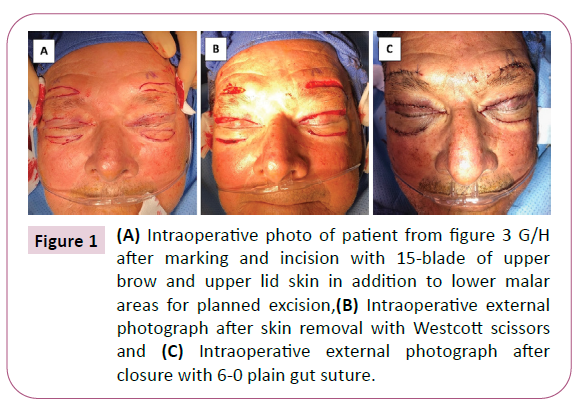
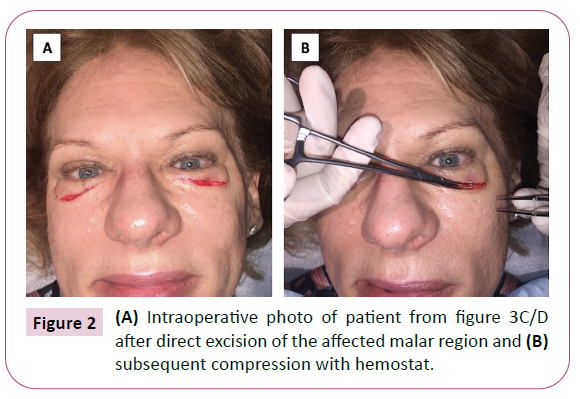
Consecutive patients presenting for evaluation of lid abnormalities including malar festoon with edema, entropion, and ectropion were evaluated in the office to determine the best individualized surgical approach. In an effort to decrease risks of anesthesia, patients were offered a one stage, multifactorial approach for their pathology in which the festoon lesion and edema were addressed at the time of their lower lid surgery. On the day of surgery, patients were evaluated in the pre-operative area while sitting upright. Markings were made in an ellipsoid fashion along the edges of the malar festoon with the patient in the upright position. The patient was prepped and draped in the usual sterile ophthalmic fashion with the patient reclined. Approximately 3-5cc of local anesthetic solution (2% lidocaine with 1:100,000 epinephrine) was injected into the lower eyelid and malar region. A #15 blade was used to create an incision along the marked lines of the festoon or malar edema. A hemostat was then used to clamp under the skin, orbicularis, and edematous tissue of the festoon for approximately 30 seconds and subsequently excised using forceps and Westcott scissors (Figures 1 and 2). Hemostasis was obtained by using bipolar cautery and gel-foam soaked in thrombin. Interrupted fixed 5-0 vicryl sutures were placed through the skin at the nasal, central, and temporal edges of the incision. The skin wound was then reapproximated using running 6-0 plain sutures. After the malar festoons were surgically excised the patient’s lower lid pathology was reassessed and the lateral canthus was tightened with 5-0 vicryl or 5-0 PDS to prevent postoperative ectropion.
Figure 1: (A) Intraoperative photo of patient from figure 3 G/H after marking and incision with 15-blade of upper brow and upper lid skin in addition to lower malar areas for planned excision, (B) Intraoperative external photograph after skin removal with Westcott scissors and (C) Intraoperative external photograph after closure with 6-0 plain gut suture.
Results
Twelve eyes of six patients underwent successful aesthetic periorbital rejuvenation for lower lid abnormalities and malar festoon via a multifactorial surgical approach comprising lower lid tightening, direct compression, and excision of the affected malar region. The average length of the festoon excision procedure ranged from 60-90 minutes. Post-operative appointments were scheduled for 2 weeks, 4 weeks, and 12-16 weeks. The longest post-operative follow up was 2 years and 9 months. Sutures were removed at the first post-operative appointment. All patients were given topical ophthalmic ointment to apply to incisions at bedtime until the tube was finished. Postoperatively, they were instructed to use artificial tears two to four times daily, cold compresses four times a day for the first week, and warm compresses twice a day for the following two weeks.
All six patients had good symmetry and position of the eyelids at their initial postoperative visit (Figure 3). (A) An 84-year old male displaying prominent festoons and bilateral upper lid dermatochalasis obstructing the superior visual field preoperatively. Patient underwent lower lid tightening, direct compression, and excision of the affected malar region to address the festoons, as well as a bilateral upper lid blepharoplasty to address the bilateral upper lid dermatochalasis, in addition to a sub-orbicularis oculi fat lift to address the vertical descent of the malar region. (B) Postoperative external photograph displays improvement of malar region, minimal scarring, and more youthful appearance of the upper lid with normalization of youthful contour. (C) A 53-year-old female displaying bilateral lower lid ectropion and prominent festoons. Patient underwent ectropion repair of bilateral lower lids as well as lower lid tightening, direct compression, and excision of the affected malar region to address the festoons. (D) Post-operative external photograph shows improved contour of the lower lids with resolution of the bilateral ectropion as well as improvement of the malar region with minimal scarring. (E) A 66-year-old male displaying visually significant bilateral upper lid ptosis, prominent festoons, and bilateral lower lid ectropion. Patient underwent ectropion repair of bilateral lower lids, as well as lower lid tightening, direct compression, and excision of the affected malar region to address the festoons. (F) Postoperative external photograph shows improved contour of the lower lids with resolution of the bilateral ectropion, resolution of upper lid ptosis, and improvement of the malar region with minimal scarring. Due to non-resolving erythema the patient was placed on Keflex 500 twice daily and noted resolution without complication. (G) A 69-year-old male displaying visually significant ptosis with bilateral upper lids in addition to dermatochalasis and prominent festoons. Patient underwent ptosis repair of the upper lids via external levator advancement, bilateral upper lid blepharoplasty, and bilateral direct brow lift. Lower lid tightening, direct compression and excision of the affected malar region was performed to address the festoons. (H) Postoperative external photographs show resolution of upper lid ptosis and dermatochalasis with youthful restoration to the contour of the upper eyelids. Resolution of the edema was noted with improvement in appearance. (I) A 65-yearold female displaying prominent festoons. Patient underwent lower lid tightening, direct compression, and excision of the affected malar region was performed to address the festoons. (J) Resolution of the edema was noted with improvement in appearance. (K) A 61-year-old male displaying prominent festoons. Patient underwent ptosis repair of the upper lids via external levator advancement, bilateral upper lid blepharoplasty, and bilateral direct brow lift. Patient underwent lower lid tightening, direct compression, and excision of the affected malar region was performed to address the festoons. (L) Postoperative external photographs show resolution of upper lid ptosis and dermatochalasis with youthful restoration to the contour of the upper eyelids. There was minimal to no residual scarring following the excision of the malar festoons with this multifactorial surgical approach. All patients were satisfied with the aesthetic appearance of their malar region and reported improvement of their ocular symptoms from lower eyelid pathology.
Most patients had mild edema of the upper or lower lids at the initial postoperative encounter, which was resolved by 4 weeks postoperatively. In the event of residual edema, intralesional doxycycline 10 mg/ml could be considered for sclerosing, but this was not necessary for any patients who underwent this technique. One patient had mild erythema on the left lower lid incision at the initial postoperative appointment. He was empirically treated with Keflex 500 mg twice a day by mouth to cover for potential infection of the incision. The erythema was resolved at the second postoperative visit.
Discussion
The etiology of malar festoons is multifactorial. The combination of senility, hereditary laxity, and gravity have been described to cause a downward descent of tissues superior to the orbicularis retaining ligament (ORL) and orbicularis muscle over the tension of a taut zygomaticocutaneous ligament (ZCL) [1-3,7]. The cephalad attenuation of the ORL allows for these tissues to hang and create the classical appearance of festoons. Due to the relative impermeability of the malar septum (MS), chronic edema and ptotic fat may also exacerbate changes in the affected malar region by stretching the overlying skin [2,8]. The complex pathophysiology had led to difficulty developing a standard approach to the surgical management of festoons. Many surgical techniques such as extended blepharoplasty, mid-face lifting, and direct excision have been described in the literature to successfully address malar festoons [1,2]. There is no consensus as to which procedure offers the best results.
Each of these techniques addresses a different mechanism in the process of festoon formation. Extended blepharoplasty utilizes a skin muscle flap technique with dissection below the orbital rim to release the retaining ligaments [2]. This procedure targets the ligamentous component of festoons but can lead to persistent and recurrent festoons from incomplete release and suspension of the ZCL and MS [2,3,6]. Blepharoplasty does not address extensive ptosis or cutaneous redundancy in the malar region, which may leave an undesirable aesthetic result [2,3].
Mid-face lifting ensures proper release of the retaining ligaments through the elevation, release, and reset of the malar septum. This approach offers the ability to correct extensive orbicularis and fat ptosis, while also improving the permeability of the malar septum to resolve edema [2,5,8]. Mid-face lifting may not be indicated based upon the individual patient’s degree of pathology, requires a much longer recovery time compared to other techniques and risks temporary or permanent damage to the sensory and facial nerve branches [2,5].
In the literature, there appears to be some consensus that direct excision of the festoon is the best surgical procedure in addressing skin redundancy [2,4,8]. This approach is limited by lower lid tension and does not address ptotic orbicularis or fat. Surgeons are often hesitant to utilize direct excision due to the possibility of scar formation in the malar region resulting in an undesirable cosmetic outcome, despite reports of minimal to no residual scar in varying racial pigmentations [1,2,4]. Einan- Lifshitz A, et al. [4] utilized one stage multi-step approach to the management of malar festoons where they initially used a lidtightening technique prior to direct excision to reduce the rate of lower lid and ocular complications. Their technique directly addressed the redundant skin through direct excision but differs from our approach by not utilizing any direct compression of the festoon with a hemostat prior to its removal.
Our technique offers the ability to address skin redundancy, ptotic orbicularis and edema of festoons in one procedure, while minimizing lower eyelid complications and recovery time. Direct hemostat compression of the festoon is a vital component of this multifactorial approach because it addresses the underlying pathology of lymphedema and distention of orbicularis leading to the formation of the malar festoon. The authors also believe it reduces postoperative residual edema and ecchymosis, providing a positive aesthetic outcome. The hemostatic compression helps to clamp off the leaky lymphatics/chronic lymphedema and creates an internal scar which forms a barrier preventing fluid from recollecting in the malar region.
A prospective study comparing the different surgical techniques used to treat malar festoons may be necessary to determine if there is a single best approach to the surgical management of malar festoons. Since a prospective study would be logistically challenging in aesthetic surgery, surgeons should be proficient in a variety of techniques to address festoons so that they may individualize their surgical approach to each patient’s varied level of pathology.
The authors of this article believe that due to the varied etiology of malar festoons, their multifaceted approach comprising lower lid tightening, direct compression, and direct excision of the affected malar region offers a safe, effective, and reproducible aesthetic rejuvenation that should be considered in the armamentarium of the surgical management of malar festoons.
Conclusion
Malar festoons remain a complex clinical challenge for surgeons to address given their diverse pathophysiology, variability in severity, and rate of recurrence. The authors report a case series successfully utilizing a multifaceted approach to the surgical treatment of malar festoons. The author’s technique comprising lower lid tightening, direct compression, and direct excision of the affected malar region generates a lasting and successful aesthetic rejuvenation of the malar region for affected patients. This novel multifactorial technique addresses the varying pathology in both the periorbital and malar regions and offers an effective, predictable, and safe therapy for malar festoons. This technique may help generate better outcomes for patients with festoons requesting periorbital rejuvenation.
Disclosure of Interest
The authors report no conflict of interest.
References
- Kpdozo DS, Nahai F, McCord CD (2014) Malar mounds and festoons: Review of current management. Aesthet Surg J 34: 235-248.
- Newberry CI, McCrary H, Thomas JR, Cerrati EW (2020) Updated management of malar edema, mounds, and festoons: A systematic review. Aesthet Surg J 40: 246-258.
- Endara M, Oh C, Davison SP, Baker SB (2015) The management of festoons. Clin Plastic Surg 42: 87-94.
- Einan-Lifshitz A, Hartstein ME (2012) Treatment of festoons by direct excision. Orbit 31: 303-306.
- Krakauer MK, Aakalu VK, Putterman AM (2012) Treatment of malar festoon using modified subperiosteal midface lift. Ophthal Plast Reconstr Surg 28: 459-462.
- Branham, GH (2016) Lower eyelid blepharoplasty. Facial Plast Surg Clin N Am 24: 129-138.
- Furnas DW (1978) Festoons of orbicularis muscle as a cause of baggy eyelids. Plast Reconstr Surg 61: 540-546.
- Hoenig JF, Knutti D, De la Fuente A (2011) Vertical subperiosteal mid-face-lift for treatment of malar festoons. Aesthet Plast Surg 35: 522-529.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences