A Novel Skin Marking Technique for Excess Skin Resection by Fleur-de-lis Abdominoplasty
Valderi Vieira da Silva Júnior
DOI10.4172/2472-1905.100029
Valderi Vieira da Silva Júnior*
Stetic Class Clinic, Institute Dr. José Frota, General Hospital Dr. César Cals, Fortaleza, Ceará, Brazil
- *Corresponding Author:
- Dr. Valderi Vieira da Silva Júnior
Stetic Class Clinic
Institute Dr. José Frota
General Hospital Dr. César Cals
Rua Barão de Aracati, 1304-Aldeota
Fortaleza, Ceará, CEP: 60.115-081, Brazil
E-mail: valderijr@hotmail.com
Received Date: August 10, 2016; Accepted Date: August 17, 2017; Published Date: August 28, 2017
Citation: da Silva Júnior VV (2017) A Novel Skin Marking Technique for Excess Skin Resection by Fleur-de-lis Abdominoplasty. J Aesthet Reconstr Surg. 3:6. doi: 10.4172/2472-1905.100029
Abstract
Introduction: Fleur-de-lis abdominoplasty is used in vertical and horizontal correction of excess skin. However, determining how much skin to resect can be challenging. In this paper we describe a high-precision skin marking technique for this purpose.
Patients and methods: Between April 2012 and June 2016, 24 patients of both sexes were submitted to fleur-de-lis abdominoplasty under peridural anesthesia and sedation, without liposuction, by the same surgeon.
Results: The average age was 44 years (range: 23-61). The mean duration of surgery was 144 min (range: 120-160). All scars were adequately aligned.
Conclusion: The technique was found to be safe and easy to perform and reproduce. Moreover, high precision helps avoid sinuous and tense scars.
Level IV: Evidence obtained from multiple time series with or without the intervention, such as case studies. Dramatic results in uncontrolled trials might also be regarded as this type of evidence.
Keywords
Fleur-de-lis; Abdominoplasty; Skin; Anesthesia; En bloc
Introduction
Anchor abdominoplasty was first performed by Weinhold in the early twentieth century. The procedure was later perfected by Somalo (1940), Dufourmentel (1959), Castañares (1967) and Regnald (1975) who introduced the fleur-de-lis design [1,2].
The procedure corrects excess skin in the vertical and horizontal dimension, but determining the amount of skin to resect can be challenging. The final tension, symmetry and quality of the scar and the risk of dehiscence, necrosis and complications potentially compromising the outcome all depend on the care taken at this first step [3,4].
The purpose of this study was to provide a stepwise description of a novel technique of skin marking for resection by fleur-delis abdominoplasty in formerly obese patients and identify the advantages associated with it.
Patients and Methods
The study included 24 formerly obese patients of both sexes submitted to fleur-de-lis abdominoplasty by the same surgeon at a public referral hospital in Northeastern Brazil between April 2012 and June 2016. All patients had experienced considerable weight loss following bariatric surgery two or more years previously. All had excess skin in the vertical and horizontal dimension and indication for fleur-de-lis abdominoplasty. Patients with excess skin in only one dimension (vertical or horizontal) were ineligible. The procedure was performed under peridural anesthesia and sedation, without liposuction.
Techniques
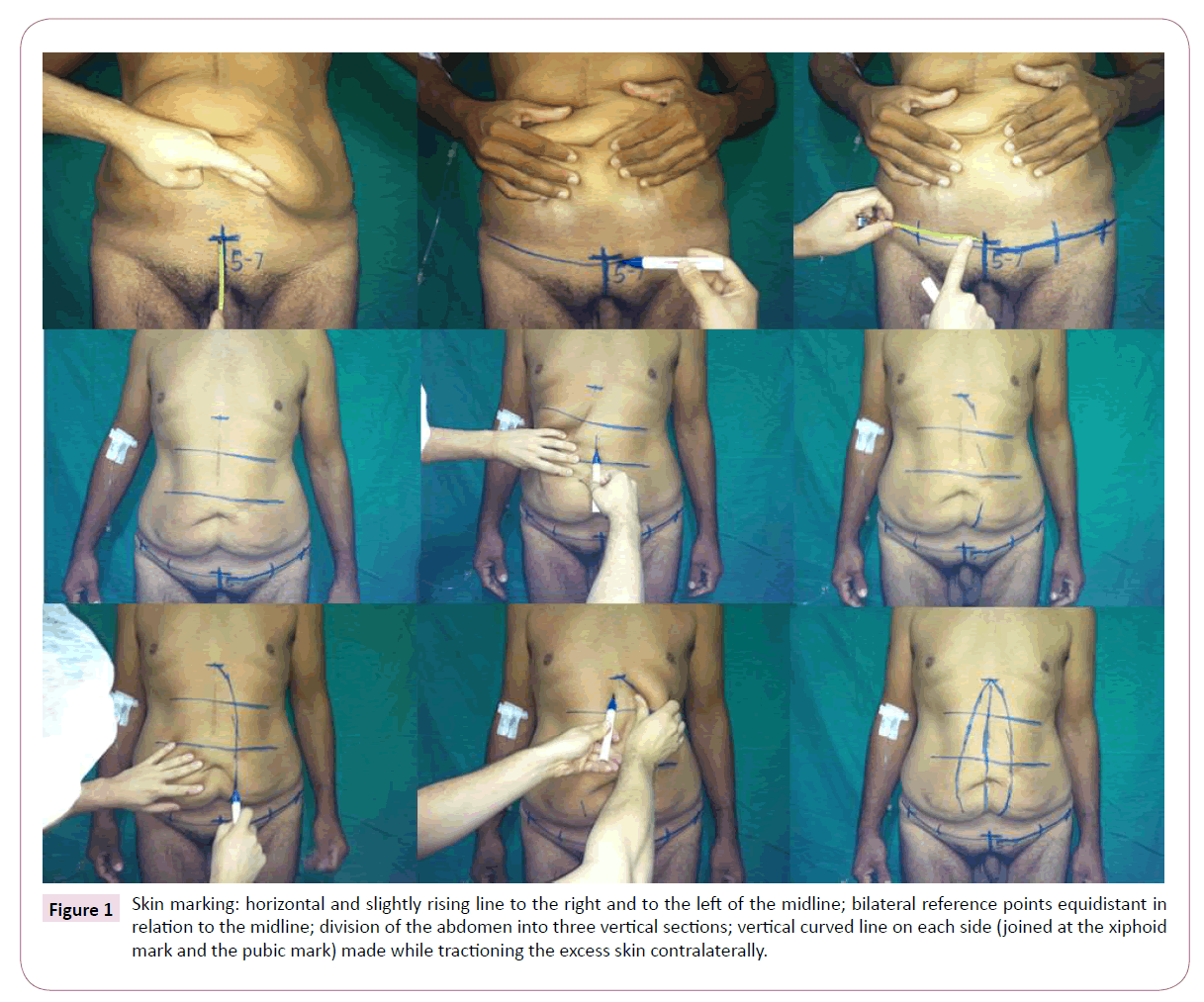
With the patient in the orthostatic position, the surgeon places a mark on the xiphoid process and another on the pubic midline at 5-7 cm above the vaginal commissure (women) or base of the penis (men) (Figure 1). From this point, a horizontal and slightly rising line is drawn to the right (X) and to the left, and two reference points equidistant in relation to the midline are marked on each side. Then the abdomen is divided vertically into three sections.
Figure 1: Skin marking: horizontal and slightly rising line to the right and to the left of the midline; bilateral reference points equidistant in relation to the midline; division of the abdomen into three vertical sections; vertical curved line on each side (joined at the xiphoid mark and the pubic mark) made while tractioning the excess skin contralaterally.
Using one hand, the surgeon tractions the excess skin of the upper third portion contralaterally and, starting at the xiphoid process, marks a line at right angles with the floor. The same is done for the middle third portion and the lower third portion. The procedure is repeated contralaterally. The result is a curved line on each side, joined at the xiphoid mark and the pubic mark (Figure 1).
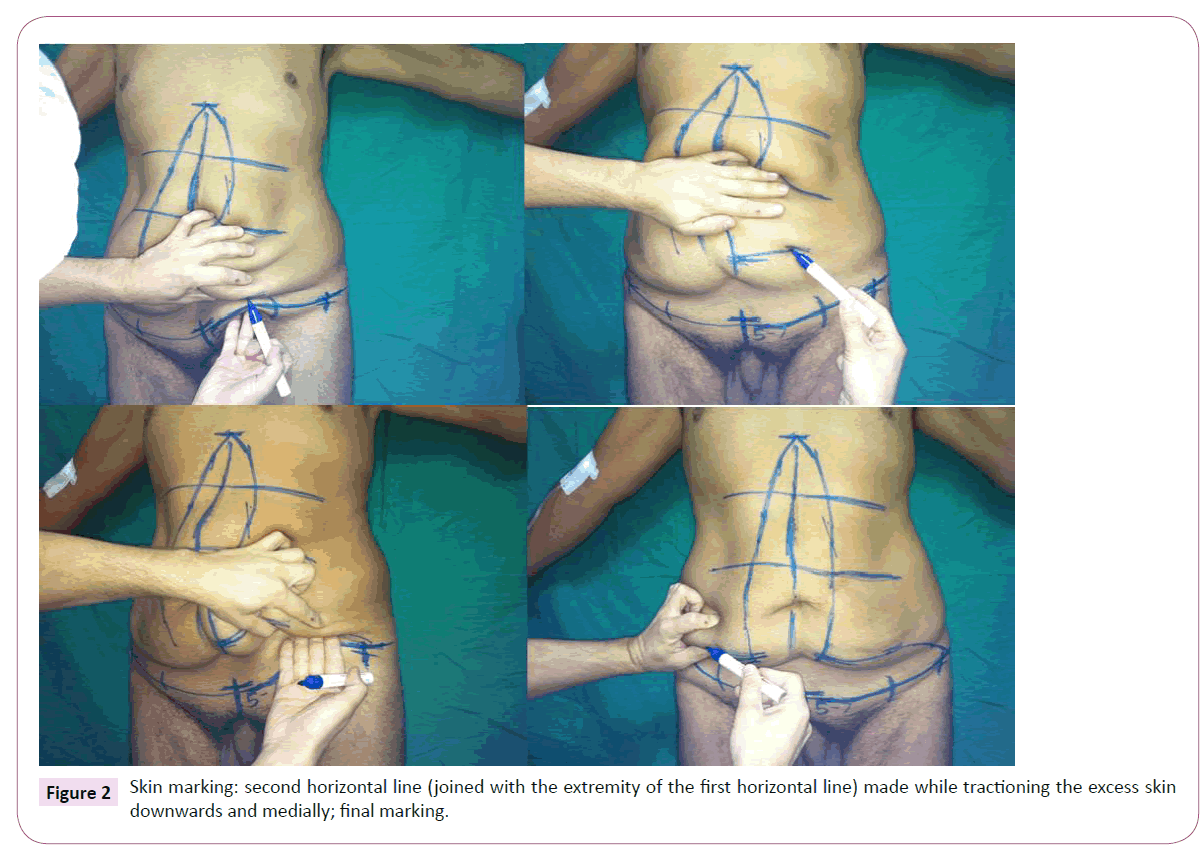
Then the skin on the right side is tractioned downwards and medially in order to draw a second horizontal line joined with the previously drawn lower horizontal line on the right side. The procedure is repeated contralaterally (Figure 2). After placing the patient in dorsal decubitus, all markings are reviewed and, if necessary, corrected. A little slack should be allowed to avoid the problem of insufficient skin at the close of the surgery.
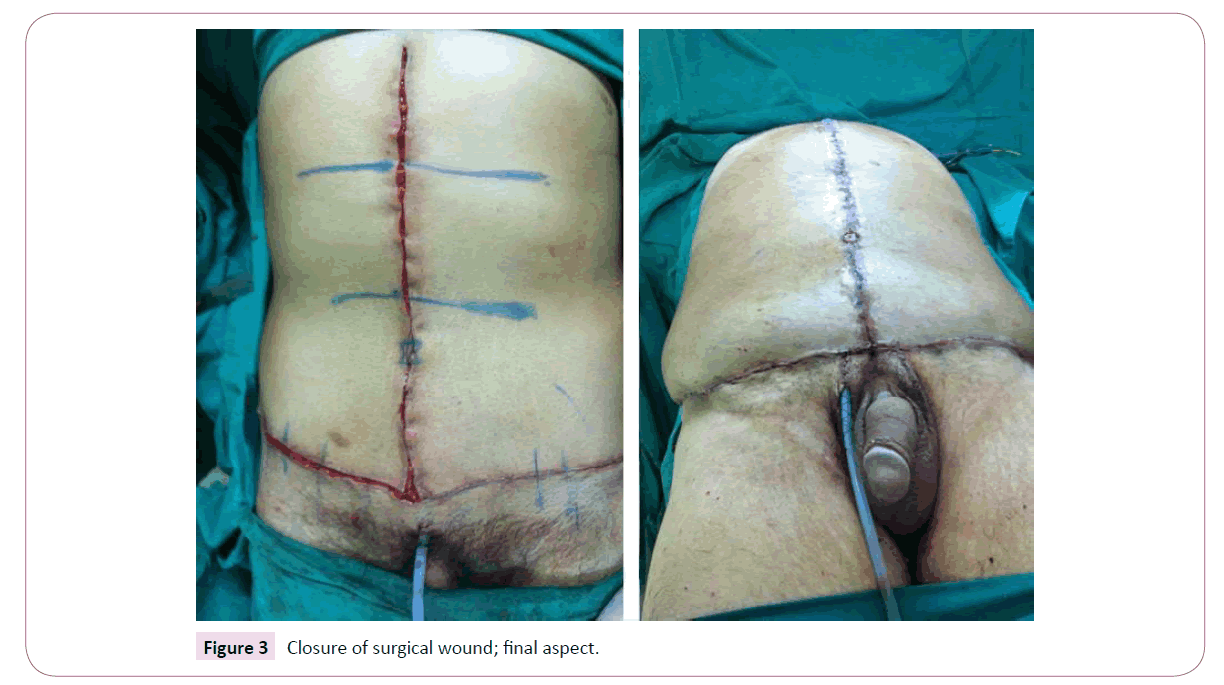
After organizing the surgical field, the excess skin is resected en bloc, followed by hemostasis, vertical plicature of the rectus abdominis muscles and insertion of a continuous vacuum suction drain (removed during recovery). The umbilical stump is preserved and sutured onto the abdominal flap using mononylon thread size 4.0. The deeper layer is sutured with polyglactin thread size 3.0 and the surface layer is sutured with polyglactin thread size 4.0 (Figure 3).
Results
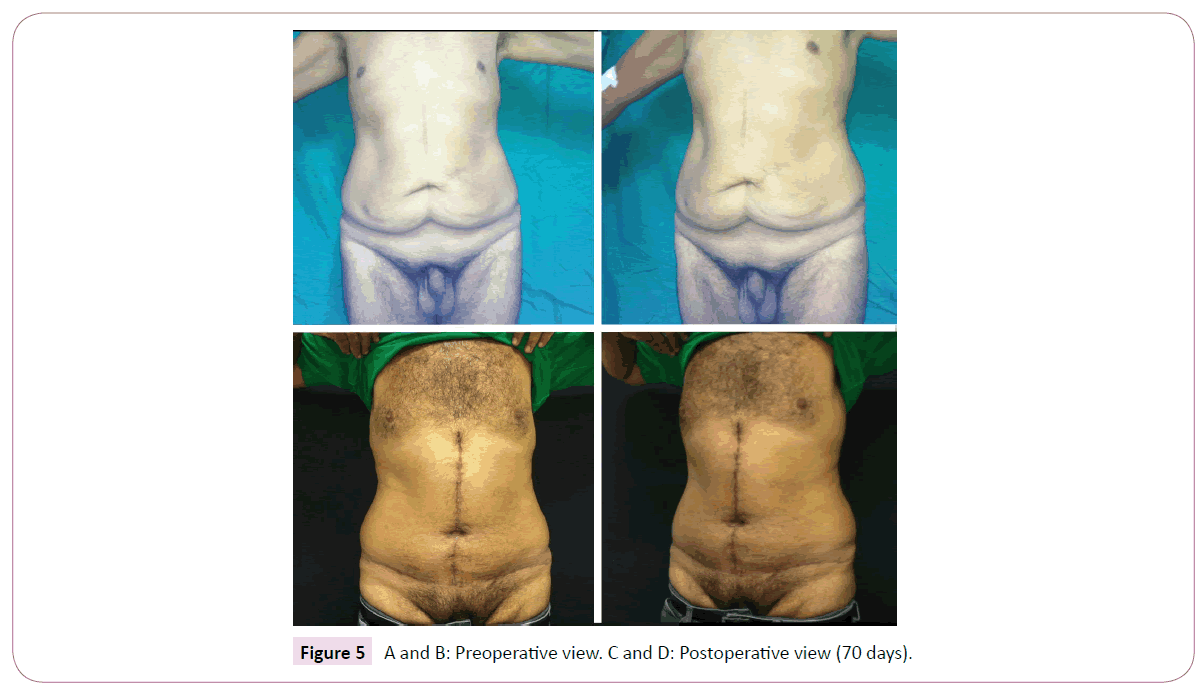
Twenty-four formerly obese patients of both sexes (M=4/F=20) aged 44 years on the average (range: 23-61) were submitted to fleur-de-lis abdominoplasty by the same surgeon between April 2012 and June 2016. The mean duration of surgery was 144 min (range: 120-160). Follow-up in the outpatient setting lasted 7.5 months on the average (range: 3-12). No hematoma, skin necrosis, tension upon surgical closure or need for additional skin detachment occurred. All scars were adequately aligned (Figures 4-6).
Discussion
Fleur-de-lis abdominoplasty is the most appropriate technique for horizontal and vertical resection of excess skin [3-6]. Surgical marking has traditionally been based on the pinch test, but with this technique the amount of resected skin will depend on how carefully the test is performed, and the result is not uncommonly a sinuous or tense scar. In addition, scars vary considerably from one surgeon to another. In contrast, our technique uses reference points and lines which reduce these variables and are easily reproduced. Precise skin marking makes resection en bloc possible, reducing time of surgery. Moreover, the wound can be closed without additional skin detachment, which might otherwise increase the risk of complications, such as skin necrosis and seroma formation.
Conclusion
The technique described in this paper is safe and easy to perform and reproduce. In addition, high precision helps avoid sinuous and tense scars.
Acknowledgment
The authors declare that they have no conflicts of interest to disclose.
References
- Lage RR, Amado BN, Sizenando RP, Heitor BS, Ferreira BM (2011) Post-gastroplasty abdominal dermolipectomy: evaluation of 100 cases operated by the. Rev Bras Cir Plást 26: 675-679.
- Roxo C, Pinheiro O, Almeida D (2001) Abdominoplastia multifuncional. Rev Bras Cir Plást 19: 64-74.
- Cavalcante H (2001) Abdominoplastia após perda de peso maciça: abordagens, técnicas e complicações. Rev Bras Cir Plást 25: 92-99.
- Gerk P (2001) Cirurgia do contorno corporal após grandes perdas ponderais. Rev Bras Cir Plást 3: 143-152.
- Le Louarn C, Pascal JF (2010) The high-superior-tension technique: evolution of lipoabdominoplasty. Aesthetic Plastic Surgery 34: 773-781.
- Bozola AR (2010) Abdominoplasty: same classification and a new treatment concept 20 years later. Aesthetic Plastic Surgery 34: 181-192.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences