An Unusual Case of a Sunken Umbilicus Post Abdominoplasty Complicated by a Keloid
Stephanie A Luster*, Oluwatobiloba Adenuga, J’nae Smith, Swathi Mohankumar, Guny Gabriel
1Department of Surgery, Flushing Hospital Medical Center, Flushing, New York, USA
2Department of Surgery, Kingsbrook Jewish Medical Center, Brooklyn, New York, USA
3St. George’s University, School of Medicine, St. George, Grenada, New York, USA
- *Corresponding Author:
- Dr. Stephanie Luster
Department of Surgery
PGY4, Flushing Hospital Medical Center
45th Avenue at Parsons Blvd. Flushing NY 11355-2199
Suite 206A, New York, USA
Tel: +718-670-5000
E-mail: jsteph.luster@gmail.com
Received Date: June 03, 2020; Accepted Date: June 11, 2020; Published Date: June 18, 2020
Citation: Luster SA, Adenuga O, Smith J, Kumar SM, Gabriel G (2020) An Unusual Case of a Sunken Umbilicus Post Abdominoplasty Complicated by a Keloid. J Aesthet Reconstr Surg. Vol.6 No.2:5 DOI: 10.36648/2472-1905.6.2.54
Abstract
Background: A 34-year-old female patient presented to the Emergency Room with a suspected umbilical abscess status post abdominoplasty 2 years prior. Intraoperatively, it was discovered that her umbilicus was sunken and buried under a keloid scar.
Case report: Our patient, a 34-year-old female, presented with complaints of periumbilical pain and swelling. After initial imaging on CT showed periumbilical soft tissue inflammation, the patient was taken to the operating room for an incision and drainage. Intraoperatively, it was discovered that her umbilicus was sunken and buried under a keloid scar. While keloids themselves are not a rare phenomenon, a sunken umbilicus covered by a keloid has not been described.
Conclusion: Keloid scars pose a challenge for physicians because they are difficult to treat, have a negative impact on patient expectations due to suboptimal results, and may require additional procedures for correction. Further research into such local postoperative complications is needed to elucidate optimal treatments and preventative measures, thereby reducing complication rates and improving aesthetic outcomes. Here we investigate the different techniques to help combat the complications of keloid scarring.
Keywords
Keloid; Sunken umbilicus; Umbilical keloid scar; Abdominoplasty; Umbilicoplasty
Introduction
A keloid is an overgrowth of dense, fibrous tissue, which results from aberrant wound healing [1]. They present as raised dermal lesions that extend beyond the boundaries of the original wound and invade the surrounding healthy skin [2]. The scar tissue does not regress spontaneously and tends to recur after excision [2]. Keloids can appear years following skin injury or they can also form spontaneously without any predisposing cutaneous trauma [3]. Presenting signs and symptoms include cosmetic disfigurement, pain, pruritus, skin discoloration, and restriction of movement. Most frequently involved sites are the chest, shoulders, arms, upper back, and head and neck areas, especially earlobes [1] (Figure 1).
Abdominoplasty is one of the most commonly performed cosmetic surgical procedures worldwide. Although it is considered relatively safe, patients are susceptible to perioperative complications. The incidence of keloid and hypertrophic scars ranges between 1% and 3.7% following abdominoplasty procedures. Male patients tend to present with less cosmetically pleasing scars than women [4]. Necrosis of the umbilicus due to insufficient irrigation through its pedicle occurs in about 0.2% of cases. Special care should be taken while performing the plication to avoid strangulation of the umbilicus [4]. Other common complications of abdominoplasty include seromas, infection, skin necrosis, hematoma, and less commonly, systemic complications such as thromboembolism [4].
Case Presentation
A 34-year-old female presented to the emergency department with complaints of swelling and periumbilical pain. She denied having any past medical history. Past surgical history included abdominoplasty two years prior in conjunction with a mammoplasty.
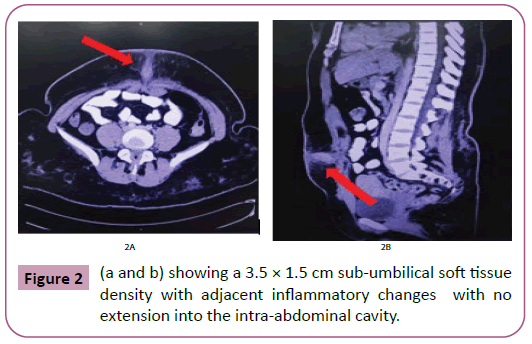
On examination, the abdomen was soft and non-distended. A keloid overlying the umbilicus was identified and elicited minor tenderness to palpation. No fluctuance or drainage was noted. A computed tomography (CT) scan of the abdomen and pelvis with contrast was done and showed a 3.5 × 1.5 cm sub-umbilical soft tissue density with adjacent inflammatory changes suggestive of sub-umbilical phlegmon. There was no extension into the intraabdominal cavity (Figures 2a and 2b).
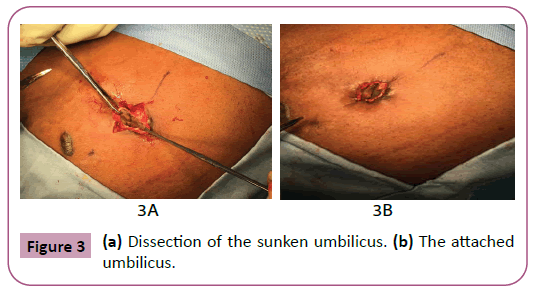
The patient was taken for incision and drainage of the umbilicus. Intraoperatively, a small curvilinear incision was made and the keloid was excised completely. A minimal amount of serous fluid was expressed. The cavity was then probed with no fluid collections identified, however, there was questionable necrosis noted in the deep posterior aspect of the cavity. After further exploration, we were able to lift the “necrotic” area discovering that it was intact skin and the patient’s sunken umbilicus. The borders of the umbilicus were dissected free from the surrounding tissue and elevated. An umbilicoplasty was performed using 3-0 vicryl sutures in the deep layer and 4-0 monocryl interrupted subcuticular sutures at the skin level. Special precautions were taken to limit the number of sutures used. At the conclusion of the procedure, 5 ml of triamcinolone were injected into the umbilical area. The patient tolerated the procedure well and was discharged from the post-anesthesia recovery unit. Unfortunately, the patient was lost to follow up, and the effects of the triamcinolone were unable to be assessed, as well as future keloid scarring (Figures 3a and 3b).
Discussion
The predisposition to keloids is an inheritable trait expressed in an autosomal dominant mode with incomplete penetrance and variable expression [1]. Keloids affect men and women equally with the highest incidence in the second and third decades of life. The diagnosis is usually made clinically based on the presenting history, as well as scar size, shape, and growth pattern [2,3]. Different advances have been studied in treating keloids and preventing their recurrence, although a definitive cure has not been identified [3]. Possible treatments include radiation therapy, flavonoids, and use of silicone gel, corticosteroids, cryotherapy, laser therapies, and platelet-rich plasma.
Radiation therapy
Radiation therapy can be used both for the prevention and treatment of keloids. It is important to keep in mind the possible risk of developing cancers in these patients weighing the risks and benefits [5]. The risk of developing secondary skin cancer from the use of radiotherapy has been seemingly rare [6,7]. According to Nestor et al. the optimal treatment of keloids using radiation is 3,000 Gy in three fractions of 600 Gy over the first three days after surgery [6]. Mankowski et al. conducted a meta-analysis to study the outcomes of various radiation-based treatments -brachytherapy, x-ray, and electron beam - in order to compare efficacy. Their research showed brachytherapy was the most effective form of radiation therapy for the treatment of keloids, showing the lowest recurrence rate of 15% compared to X-ray and electron beams that were comparable at 23%. They also highlighted the most common consequence of radiation therapy is a change in pigmentation of the skin [8].
Flavonoids
Flavonoids occurring naturally, as in onions, have shown to be used in the prevention of the formation of scars. Exact mechanisms are poorly understood, but it has shown a decrease in the activity of fibroblasts in the extracellular matrix [3,5,9]. Pikula et al. described the use of onion extracts in high doses causing apoptosis is dermal fibroblasts. Research is limited however and more investigations should be performed [10].
Corticosteroids
Injections of corticosteroids, steroid ointment tapes, or plasters are at the forefront of treatment and prevention of keloids [9,11,12]. In this patient we injected triamcinolone into the affected area after closure of the incision and removal of keloid to prevent recurrence. Triamcinolone is a synthetic steroid; it works by decreasing the activity of elements in the body that cause inflammation and also by decreasing fibroblast proliferation. According to Khalid et al., although triamcinolone is the gold standard as of now for the treatment of keloids, a combination of triamcinolone and 5-fluorouracil yielded a more effective outcome. Good to excellent results were seen in 68% of patients [13].
Surgery
Surgery in general is a risk factor for the development of keloids. Incisions with mechanical tension have shown to produce more scarring, described as mechano-transduction [5]. Hence, using a tension-free closure to reduce more inflammation is promising in preventing keloid scars. Examples of such surgical techniques are zig-zag sutures, flap surgeries, and fascial/subcutaneous tensile reduction sutures [5,6,8]. Zig-zag sutures are linear sutures that have a faster healing time limiting the progression of keloids in patients. Flap surgeries, more specifically local flaps, help release contraction in scars.
A combination of surgery, radiation, and steroids would provide a better outcome for the treatment of keloids [8,12,14]. According to Yamawaki et al. a combination treatment of surgical excision and radiation resulted in an 89% cure rate, during the course of the two years postoperatively patients were followed for any signs of recurrence and were given injections of steroids at the site of the lesions as soon as it was identified [15].
Laser therapy
Laser therapy is a relatively new treatment modality that has emerged for managing keloids and hypertrophic scars. The mechanism behind laser therapy is based on the principle of “selective photothermolysis” which was coined in 1983 [16]. According to this principle, light can be used to target specific chromophores (hemoglobin and oxyhemoglobin, melanin, and water) which respond to a specific wavelength and are then selectively destroyed [17]. Tissue effects depend upon the properties of light and the interaction of light with these chromophores [18].
Laser therapy has proven particularly useful in treating keloids and hypertrophic scars because it causes vascular destruction, which leads to tissue hypoxia, cell catabolism, and reorganization of collagen deposition [19]. The heat generated by lasers also initiates inflammation and increases vascular permeability, matrix metalloproteinase production, and collagen fiber decomposition [18]. Early application of lasers is thought to shorten the duration of acute inflammatory response and accelerate the time to scar maturation [18].
Lasers can be classified as ablative or non-ablative. Ablative lasers act on the water present in tissues causing them to vaporize, whereas non-ablative lasers act on melanin or hemoglobin leading to tissue necrosis [20]. There are four main types of lasers that are commonly used for keloids and hypertrophic scars with proven efficacy: pulsed dye laser (PDL), fractional carbon dioxide laser (fCO2), intense pulse light (IPL), and alexandrite and diode lasers. Usually, two or more modalities are combined to improve the outcome [18]. According to medical guidelines, ablative fractional laser or PDL therapy is indicated for minor keloids that failed to improve within 8 to 12 weeks with silicone gel sheeting, or major keloids that failed to improve with corticosteroids and 5-FU [18]. Laser treatment needs to be tailored to the patient, but it is typically delivered in 4-6 week intervals until a plateau in improvement is observed [19]. Laser therapy provides a novel approach to treating keloids and hypertrophic scars, which may result in improved aesthetic outcomes and decreased keloid recurrence.
Platelet-rich plasma
Platelet-rich Plasma (PRP) is also thought to have potential value in treating keloids. PRP is an autologous blood-derived product enriched in platelets, growth factors, and chemokines/ cytokines delivered in a concentrated volume of plasma [21]. PRP is reported to have 3-5 times the concentration of platelets normally found in wounds, and the resulting growth factor release following activation can further stimulate cell proliferation and tissue regeneration [21].
PRP is shown to stimulate tissue repair, accelerate wound healing, and decrease pain and disability in treated areas. In a study by Jones et al. there was evidence of improved wound healing with lower keloid recurrence with surgical excision and PRP alone, prior to the use of radiation therapy. As a result, it was recommended that all patients receive PRP to the surgical site [22]. Another study by Hersant et al. found that nearly 53% of keloid scars completely resolved with PRP two years posttreatment. This study also concluded that PRP is an effective and safe method for treating postoperative keloid scars refractory to conventional therapy [23].
In this case, we also considered the likelihood of the cause of the sunken umbilicus to be from a post-operative seroma. A seroma is defined as a collection of fluid under the skin. Seroma formation is the most common postoperative complication of an abdominoplasty, with a range of occurrence between 5% to 43% according to Seretis et al., preventative measures shows a reduction in the occurrence of seromas on average to 7.5% [24]. One of the most common preventative measures are surgical tension suture techniques. At the forefront of this technique, progressive tension sutures (PTS), in addition to drains, during the closure of the procedure are utilized. According to Jabbour et al. the technique involves using adhesion sutures while progressively moving abdominal flap from proximal to distal during closure allowing for the closing of dead space where the seroma would normally form [25]. Seroma treatment is dependent on the size; small seromas often do not require any treatment as they mostly resolve on their own, whereas larger seromas require aspiration to drain the fluid. Without intervention, seromas usually follow a natural course, resolving themselves anywhere between one month to a year [26]. In choosing treatment options and surgical techniques it is important to note that it varies from patient to patient. Various medical history factors and location of the keloid play roles in the choice of treatment.
Conclusion
We have presented a case of an incidentally discovered sunken umbilicus buried under a keloid scar. Although the sunken umbilicus could have been caused by a post-operative seroma, the intraoperative findings and history, led us to believe the more likely cause was a large keloid. This patient was lost to follow up, so a post-operative treatment plan could not be developed. However, with multiple modalities at a cosmetic surgeon’s finger tips, the keloid scar could have been treated or avoided altogether. Especially in the field of aesthetic surgery, identifying patients more prone to keloid scarring and providing the best post-operative treatment plan is crucial.
References
- Berman B, Bieley HC (1995) Keloids. J Am Acad Dermatol 33 (1): 117-123.
- Goldstein BG, Goldstein AO, Hong AM (2020) Keloids and hypertrophic scars.
- Ghazawi FM, Zargham R, Gilardino MS, Sasseville D, Jafarian F (2018) Insights into the pathophysiology of hypertrophic scars and keloids. Adv Wound Care 31 (1): 582-595.
- Vidal P, Berner JE, Will PA (2017) Managing complications in abdominoplasty: A literature review. Arch Plast Surg 44 (5): 457-468.
- Lee H, Jang Y (2018) Recent understandings of biology, prophylaxis and treatment strategies for hypertrophic scars and keloids. Int J Mol Sci 19 (3): 711.
- Nestor MS, Berman BB, Goldberg DJ, Cognetta AB, Gold M, et al. (2019) Consensus guidelines on the use of superficial radiation therapy for treating non-melanoma skin cancers and keloids. J Clin Aesthet Dermatol 12 (2): 12-18.
- Xu J, Yang E, Yu NZ, Long X (2017) Radiation therapy in keloids treatment. Chin Med J 130 (14): 1715-1721.
- Mankowski P, Kanevsky J, Tomlinson J, Dyachenko A, Luc M (2017) Optimizing radiotherapy for keloids. Ann Plast Surg 78 (4): 403-411.
- Mari W, Alsabri SG, Tabal N, Younes S, Sherif A, et al. (2015) Novel insights on understanding of keloid scar: article review. J Am Coll Clin Wound Spec 7 (1-3): 1-7.
- Pikuła M, Żebrowska ME, Olech LP, Baranowska MK, Sznitowska M, et al. (2013) Effect of enoxaparin and onion extract on human skin fibroblast cell line: therapeutic implications for the treatment of keloids. Pharm Biol 52 (2): 262-267.
- Ogawa R (2017) Keloid and hypertrophic scars are the result of chronic inflammation in the reticular dermis. Int J Mol Sci 18 (3): 606.
- Ogawa R, Akaishi S, Kuribayashi S, Miyashita T (2016) Keloids and hypertrophic scars can now be cured completely: recent progress in our understanding of the pathogenesis of keloids and hypertrophic scars and the most promising current therapeutic strategy. J Nippon Med Sch 83 (2): 46-53.
- Khalid FA, Mehrose MY, Saleem M, Yousaf MA, Mujahid AM, et al. (2019) Comparison of efficacy and safety of intralesional triamcinolone and combination of triamcinolone with 5-fluorouracil in the treatment of keloids and hypertrophic scars: A randomized control trial. Burns 45 (1): 69-75.
- Siotos C, Uzosike AC, Hong H, Seal SM, Rosson GD, et al. (2019) Keloid excision and adjuvant treatments. Ann Plast Surg 83 (2): 154-162.
- Yamawaki S, Naitoh M, Ishiko T, Muneuchi G, Suzuki S (2011) Keloids can be forced Into remission with surgical excision and radiation, followed by adjuvant therapy. Ann Plast Surg 67 (4): 402-406.
- Anderson R, Parrish J (1983) Selective photothermolysis: A precise microsurgery by selective absorption of pulsed radiation. Science 220 (4596): 524-527.
- Kronemyer B (2017) Laser and injectable options for treatment of keloids. Dermatology Times. Telehealth Webinar.
- Hultman CS, Yoshida S (2019) Laser therapy for hypertrophic scars and keloids.
- Leszczynski R, Da Silva CA, Kuczynski U, Da Silva EM (2015) Laser therapy for treating hypertrophic and keloid scars. Cochrane Database of Systematic Reviews.
- Mamalis AD, Lev-Tov H, Nguyen DH, Jagdeo JR (2013) Laser and light-based treatment of keloids: A review. J Eur Acad Dermatol Venereol 28 (6): 689-699.
- Alser OH, Goutos I (2018) The evidence behind the use of platelet-rich plasma (PRP) in scar management: A literature review. Scars, Burns and Healing p. 4.
- Jones ME, Hardy C, Ridgway J (2016) Keloid management. Adv Wound Care 29 (7): 303-307.
- Hersant B, Sid Ahmed-Mezi M, Picard F, Hermeziu O, Rodriguez AM, et al. (2018) Efficacy of autologous platelet concentrates as adjuvant therapy to surgical excision in the treatment of keloid scars refractory to conventional treatments. Ann Plast Surg p. 1.
- Seretis K, Goulis D, Demiri EC, Lykoudis EG (2017) Prevention of seroma formation following abdominoplasty: a systematic review and meta-analysis. Aesthet Surg J 37 (3): 316-323.
- Jabbour S, Awaida C, Mhawej R, Habre SB, Nasr M (2016) Does the addition of progressive tension sutures to drains reduce seroma incidence after abdominoplasty? A systematic review and meta-analysis. Aesthet Surg J.
- Stanczyk M, Grala B, Zwierowicz T, Maruszynski M (2007) Surgical resection for persistent seroma, following modified radical mastectomy. World J Surg Oncol 5 (1): 2-8.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences