Collaborative Research in Plastic Surgery - The Only Way Forward
Umar Choudry
DOI10.4172/2472-1905.100002
Associate Professor, Chief, Division of Plastic Surgery, Department of Surgery, University of Minnesota Medical School, Minneapolis, MN, USA
- *Corresponding Author:
- Umar Choudry MD
Associate Professor, Chief, Division of Plastic Surgery
Department of Surgery, University of Minnesota Medical School
Minneapolis, MN, USA
E-mail: choud008@umn.edu
Received date: September 22, 2015; Accepted date: September 25, 2015; Published date: October 05, 2015
Citation: Umar Choudry MD. Collaborative Research in Plastic Surgery - The Only Way Forward. J Aesthet Reconstr Surg. 2016, 1:2. doi: 10.4172/2472-1905.10002
Editorial
The field of plastic surgery is ever-changing and advancing faster than almost any other field in surgery. We are an innovative discipline, and adopt new technologies and techniques more readily than our sister specialties. This dynamism is rooted in our curiosity as plastic surgeons, and is perpetuated by the understanding that there are a myriad of principled ways of accomplishing a surgical solution to a reconstructive patient’s problem. This leads to the need for a collaborative approach in many things we do, especially in research. This collaboration spans fellow plastic surgeons, institutions, and industry. Keeping abreast of the advances globally is equally important and vital to our success as a specialty. This is accomplished through combining international professional societies, having international meetings, and having global associations through journals and publications. It is my goal to make our new publication, the Journal of Aesthetic and Reconstructive Surgery, be a source of truly global, collaborative, and innovative research and clinical concepts.
I have presented a small example of such a global and collaborative initiative. I published a paper in Plastic and Reconstructive Surgery in 2012 [1] discussing the preoperative assessment preferences and reported reoperation rates for size change in primary breast augmentation by surveying ASPS (American Society of Plastic Surgeons) members. It highlighted the diversity of approaches and planning principles followed by plastic surgeons in the United States. It also described the momentum shift towards an anatomic basis for implant selection. Breast base diameter (BBD) was the cardinal anthropometric parameter utilized by those surgeons who prioritized the patient’s anatomy over the patient’s desire for a particular implant volume (IV) as a guiding principle for selection. On the other hand, there were still a considerable number of surgeons who felt that the final implant volume had paramount importance over other potential factors. The paper concluded that those surgeons who ranked IV lower than BBD in implant selection, also reported fewer reoperation rates for size change (p=0.004).
We (Dr. Raman Meharzad, Dr. Nicholas Kim, and Dr. Umar Choudry) wanted to follow up on this under-published topic by getting a more global perspective on breast implant selection, and therefore, decided to survey a cohort of European plastic surgeons. A survey of the members of the Swedish Association of Plastic Surgeons (SAPS) was conducted using the original questionnaire used in our published paper [1]. Our aim was to report on the planning principles and perceptions of plastic surgeons from a country other than the United States and analyze any relevant differences. We hoped that this would broaden the perspectives of our member surgeons. We had a response rate of 25 percent (n=34), similar to the ASPS survey rate of 20.1 percent (n=604). We collected and analyzed the data similar to the described methods in our original article [1]. Each of the 8-survey questions used in the seminal article [1], the reported responses by SAPS members, and the comparison to the ASPS member responses from the original article [1] are detailed below:
Question 1: What preoperative measurement or assessment system do you currently use to choose a patient’s potential breast implant?
Both groups of plastic surgeons preferred to utilize their own system for choosing implants (ASPS surgeons: 54.3%; SAPS surgeons: 61.8%). ASPS plastic surgeons tended to use the Tebbetts system (TEPID) [2] significantly more (23.8%) often than their SAPS counterparts (8.8%).
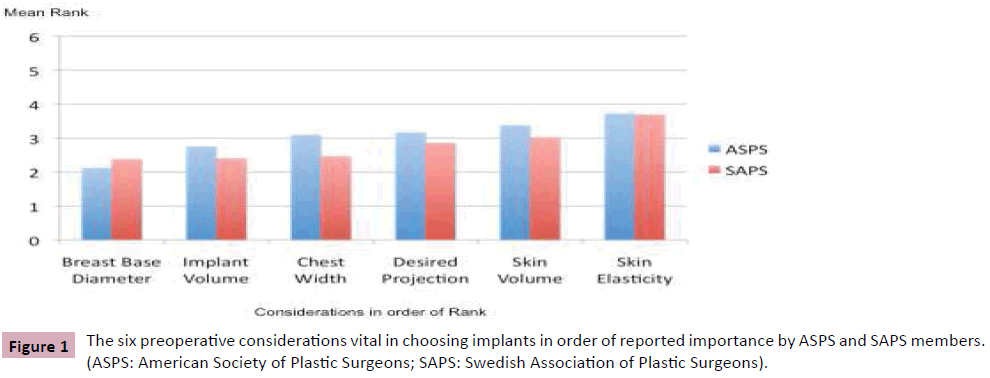
Question 2: Please RANK, in order of importance (with 1 being the most important and 6 being the least important), the following considerations that you feel are vital in choosing implants.
BBD was clearly the highest ranked variable by ASPS surgeons (Figure 1). However, SAPS surgeons ranked BBD and IV equally. Despite this, SAPS surgeons who ranked IV higher, also reported a higher reoperation rate for size change (p=0.03). This correlation was also seen in the ASPS member data analysis.
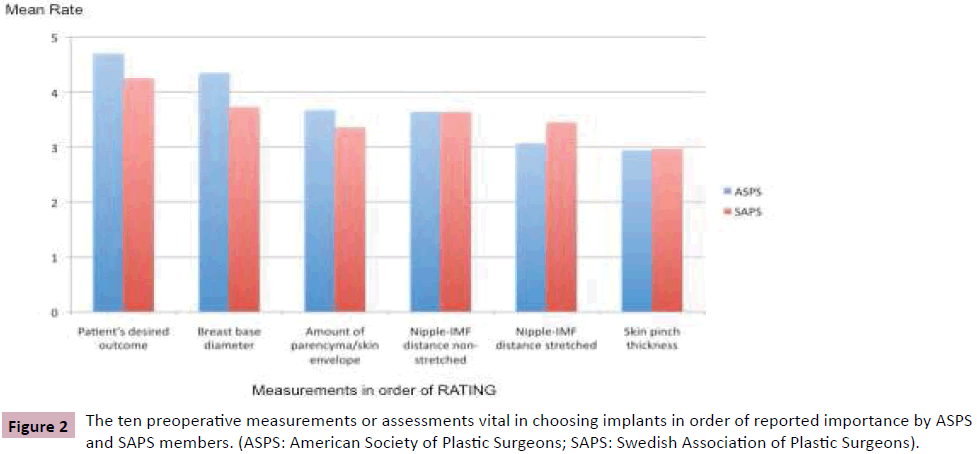
Question 3: Please RATE the importance (with 5 being the highest and 1 being the lowest) of the following measurements or assessments in your pre-operative decision-making process.
This was answered very similarly by both sets of surgeons, with the patient’s desired outcome and BBD given the highest rate of importance. However, for the SAPS members, those who rated BBD maximally at “5” reported significantly lower reoperation rates for size change compared to those surgeons who did not (i.e., rate of <5) (p=0.005). Interestingly, this correlation was not found among the ASPS members (p=0.121) (Figure 2).
Question 4: How often do you resolve the issue in the event of conflict with your patient around implant size?
One could see interesting differences between the U.S. and Swedish perspective on resolving such a situation. ASPS surgeons would reeducate their patients much more (63.7%) compared to their SAPS counterparts (44.1%). Additionally, SAPS surgeons were more likely to decline surgery (20.6%) than ASPS surgeons (7.5%).
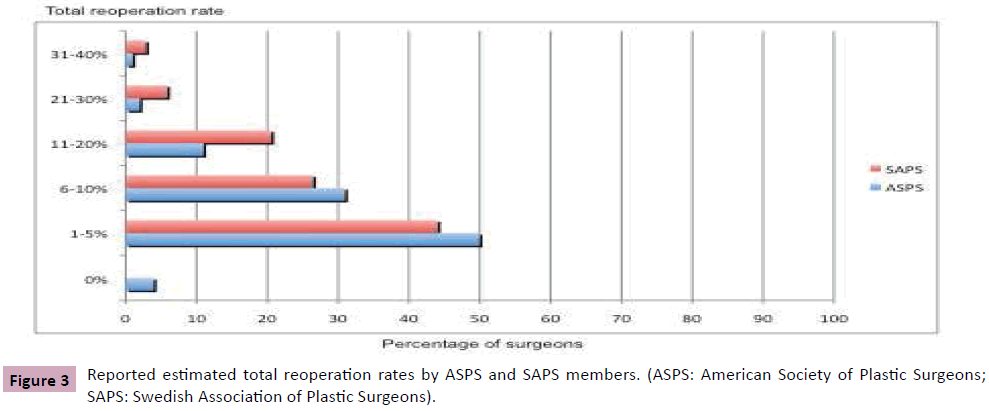
Question 5: Please estimate your total reoperation rate after primary breast augmentation.
The reported distribution of total reoperation rates was similar for both groups.
Question 6: Please RANK in order of frequency (with 1 being the most frequent and 6 being the least frequent) the different reasons for your reoperations after primary breast augmentation.
Capsular contracture was reported by both sets of surgeons as the most common reason for reoperations in primary breast augmentation, while size change ranked 2nd by ASPS surgeons, and 3rd by SAPS surgeons (Figure 3).
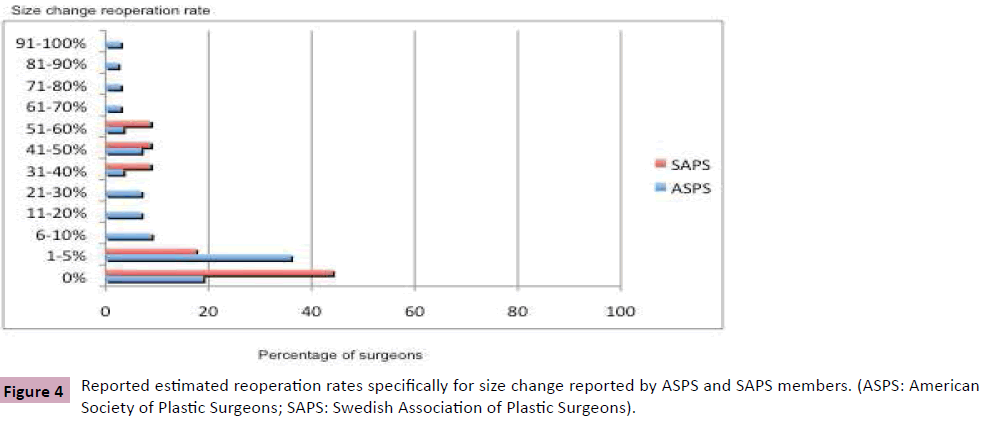
Question 7: Please estimate your percentage of reoperations that are specifically related to size change after primary breast augmentation.
Reported reoperation rates for size change were quite different between the two groups of surgeons. A significantly larger percentage of SAPS surgeons reported no size change reoperations compared to ASPS surgeons. Additionally, 62 percent (n=21) of SAPS surgeons, compared to 55 percent (n=332) of ASPS surgeons, reported a less than 5 percent rate for size change; and, 38 percent (n=9) of SAPS surgeons, compared to 45 percent (n=272) of ASPS surgeons, reported a more than 5 percent rate of size change (Figure 4).
This survey highlighted that, in general, plastic surgeons in the United States and Sweden have similar thoughts on planning principles and assessment preferences for implant selection in primary breast augmentation. The trend of using anthropometric parameter based implant selection seems to be gaining momentum even in Sweden as it has in the United States. More importantly, this survey mirrored the findings seen in the U.S. survey on rates of reoperations for size change. Surgeons in both groups reported lower size change rates when implant selection was based on anatomical parameters, and higher rates when implant volume was the basis for implant selection. This finding confirms, again, the perception and reported better outcomes seen by plastic surgeons in terms of reduction in size change rates with tissue-based implant selection [2-5].
There were an also a few important differences between the two groups of surgeons noted that are worthy of highlighting:
1. The Tebbetts system was more widely used by ASPS surgeons.
2. SAPS surgeons were less likely to reeducate their patients and more likely to refuse surgery to patients where there was a conflict about implant size.
3. SAPS surgeons reported a significantly higher 0% reoperation rate for size change.
This survey gives U.S. plastic surgeons a more global perspective on breast implant selection. It allows them to compare the polled ASPS member views to a European cohort of plastic surgeons, which may impact their decision making process in primary breast augmentation.
Acknowledgement
I want to give a special thanks to Raman Meharzad, MD and Nicholas Kim, MD who were instrumental in the conduction of the study".
References
- Choudry U, Kim N (2012) Preoperative assessment preferences and reported reoperation rates for size change in primary breast augmentation: a survey of ASPS members. Plast Reconstr Surg 130: 1352-1359.
- Tebbetts JB (2002) A system for breast implant selection based on patient tissue characteristics and implant-soft tissue dynamics. Plast Reconstr Surg 109: 1396-1409.
- Tebbetts JB (2006) Achieving a zero percent reoperation rate at 3 years in a 50-consecutive-case augmentation mammaplasty premarket approval study. Plast Reconstr Surg 118: 1453-1457.
- Tebbetts JB, Adams WP (2005) Five critical decisions in breast augmentation using five measurements in 5 minutes: The high five decision support process. Plast Reconstr Surg 116: 2005-2016.
- Adams WP, Bengston BP, Glicksman CA, Gryskiewicz JM, Jewell ML, et al. (2004) Decision and management algorithms to address patient and food and drug administration concerns regarding breast augmentation and implants. Plast Reconstr Surg 114: 1252-1257.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences