Comparison between Methods of Reconstruction after Nasal BCC Skin Excision
Ali Alizade*, Hosseini SN and Vakili MM
Department of Plastic and Reconstructive Surgery, Zanjan University of Medical Science, Ayatollah Mousavi Hospital, Zanjan, Iran
- *Corresponding Author:
- Dr. Ali Alizadeh
Department of Plastic and Reconstructive Surgery
Zanjan University of Medical Science
Ayatollah Mousavi Hospital, Zanjan, Iran
Tel: 0989123837701
E-mail: ali110alizadeh@yahoo.com
Received Date: May 08, 2021; Accepted Date: June 17, 2021; Published Date: June 24, 2021
Citation: Alizadeh A, Hosseini SN, Vakili MM (2021) Comparison between Methods of Reconstruction after Nasal BCC Skin Excision. J Aesthet Reconstr Surg Vol.7 No.4:31.
Abstract
Background: Basal cell carcinoma (BCC) is the most common malignant cutaneous lesion affecting the nose. With the rising incidence of skin cancers, plastic surgeons increasingly face nasal reconstruction challenges after excision of BCC, and in addition to size and depth of the tumor, aesthetic considerations such as color, contour, skin consistency, nose retraction and scarring plays a major role in selecting the type of nasal tumor reconstruction surgery in order to obtain natural function and a beautiful appearing nose. Since a patient’s skin is thicker in this area and also because of the late referral of patients for treatment and also having to make a choice concerning an appropriate reconstruction method for preventing tumor recurrence in future, and achieving appropriate function of nose and appearance, it was decided to compare flap, graft and primary closure methods.
Methods: This retrospective study reviewed 80 patients suffering from basal cell cancer (BCC) who underwent tumor excision and nasal reconstruction during September 2014 to April 2018. In this study the amount of satisfaction, beaut y and recurrence of the illness after nasal reconstruction was evaluated in 4 weeks, 6 months and 19 months after surgery.
Results: In the present study, although using graft surgery is accompanied with maximum satisfaction in the short term due to it facilitating the work at hand and due to less use of skin excision in comparison with flap surgery, but in the long term it is accompanied with undesirable results due to the resulting unattractive appearance. In our study we surprisingly found that long term flap reconstruction often leads to optimal satisfaction and cosmetic results in comparison with graft and primary closure method after 6th months that were found to be completely meaningful using chi-square test with a p-value of 0.05.
Conclusion: Since the results obtained in our study are meaningful according to the satisfaction level and by achieving aesthetic considerations of patients, the flap method is proposed as opposed to the two methods of graft and primary closure, obtaining tumor free margins and pleasing aesthetic results are major concerns in nasal reconstruction.; In small excised BCC tumors where the resulting defects are equal to or smaller than 1.4 cm, in order to prevent tumor recurrence in the future, instead of excising a margin of 2 mm or less, right from the start a margin of 4 mm or more is excised and flap surgery is performed instead of primary closure.
Keywords
BCC (Basal Cell Carcinoma); Flap; Graft; Primary closure; Patient satisfaction; Aesthetic considerations; Recurrence
Introduction
Among the skin cancers, BCC is the most common malignant cancer that affects the nose (the most common place affected by BCC on the face is the nose which makes up 30 percent of cases). Considering the increasing prevalence of skin cancers, plastic surgeons face challenges with regards to nasal reconstruction after excision BCC cancer. In addition to the size and depth of the tumor, aesthetic considerations such as color, contour, skin consistency, nose retraction and scarring plays a major role when selecting the type of nasal tumor reconstruction surgery in order to obtain natural function and a beautiful appearing tones. Since a patient’s skin is thicker in this area and also because of late referral of patients for treatment and also having to make a choice concerning the appropriate reconstruction method for preventing tumor recurrence in future, some challenges arise when selecting flap, graft or initial repair and for this reason, there is a need to study comparison reviews on flaps, grafts and initial repair, therefore decisions were made based on comparison reviews on skin flaps and grafts and initial repair in patients who had undergone surgery according to patient satisfaction, aesthetic considerations and recurrence after surgery. Consequently, it can be said that the main goal of performing the present study was to determine and compare surgical methods including flaps, grafts and initial repair in the reconstruction of nasal cancer symptoms after excision of a skin lesion of that area [1].
Literature Review
This study was carried out on 80 patients referring to the Plastic and Reconstructive Surgery Clinic of Ayatollah Mousavi Hospital, Zanjan with the ethical code A-12-152-7. Our study is a quasiexperimental study. In this study 20 patients out of 100 patients with nasal cancer were omitted from the study due to SCC and underlying diseases such as diabetes, vascular disease, other malignancies and collagen diseases and immunosuppressing receivers. 80 patients with nasal BCC underwent excision and nasal reconstruction by flap, graft and primary closure (from September 2014-April 2018). This study is verified due to observing the Helsinki Declaration and by Medical Ethics Committee.
Informed consent was obtained from all patients. Demographic information and perioperative details of the patient’s operation regarding age, gender, location of tumor, tumor type diagnosis, reconstruction methods, follow up duration and postoperative complications were separately recorded. In this study 80 patients aged between 40 and 95 who had undergone nasal reconstruction surgery, (flap, graft and primary closure) due to Basal Cell Carcinoma (BCC) between September 2014 to May 2018, were studied respectively [2].
The variables were examined in this study include amount of patient satisfactionand cancer recurrence, aesthetic consideration status, age average and gender in the 4th week and 6th month after nasal reconstruction surgery. Patients with underlying diseases such as diabetes, vascular disease and collagen diseases, consumers of corticosteroids and immunosuppressive drugs and melanoma tumors and squamous cell carcinoma were excluded from the study. These patients were followed up for 19 months after nasal reconstruction surgery with three methods of flap, graft and primary closure and two items of their satisfaction and aesthetic considerations were assessed in 4th week and 6th month post-operatively and tumor recurrence in the 19th month. Satisfaction status was assessed by a questionnaire completed by patient s and three items of aesthetic, natural function and psychological aspects were considered in this questionnaire. The amount of tumor recurrence was assessed based on an examination made by an attending physician in the 4th week and 6th month and later in the 19th month post-operatively using several items including excision amount of tumors from units and subunits, bumps and depressions, and regular margins in the initial examination, and finally aesthetic consideration status was assessed using the pre-arranged visits in the 4th week and 6th month and nasal reconstruction pre-operation and postoperation pictures analyzed by a plastic surgeon [3].
Excisional biopsy is done for tumors with diameters lower or equal to 1 cm in order to prove malignancy, an incisional biopsy was performed for tumors larger than 1 cm in diameter. After excision of tumor, all remaining defects were reconstructed by primary closure or using local flaps and grafts aiming to preserve aesthetic issues of nasal subunits. In this study defects larger than 1.4 cm, after excision were reconstructed by various types of flaps including Limburg, bilobed, nasolabial, v-y advancement, forehead and glabellar or using grafts (from behind the ear or subclavian). Although in defects larger than 1.4 cm in lose skin and skin that reached each other with undermining method, instead of flaps or graft s, primary closure is used.
In general, in defects smaller or equal to 1.4 cm, primary closure was used but in thick and firm skin, flaps were used instead. According to previous studies, nasal defects were categorized into subgroups including 1/3 proximal, 1/3 middle and 1/3 distal and a reconstruction method was used for each. As a rule, in proximal, middle and distal defects smaller than 1.4 cm reconstruction is done by primary closure and in defects larger than 1.4 cm in the central and lateral part of proximal, reconstruction it is done using a glabellar flap and in the central part of middle part, miter flap or bilobed and in the lateral part, nasolabial flap or v-y flap are used. In defects larger than 1.4 cm the middle part of distal part, the Limberg flap or bilobed and in lateral parts of the distal part, nasolabial flap or v-y are used. Furthermore, in defects larger than 1.4 in the middle part of the distal part, the Limberg flap or bilobed, and in the lateral part of distal part, nasolabial flap or v-y are used. Also in defects larger than 1.4 cm in the distal part and larger than one third (two third distal), the frontal flap is used. In general in defects larger than 1.4 cm and in reconstruction by frontal flap method, patients underwent general anesthesia and in other patients with defects smaller than 1.4 cm, nasal reconstruction was done under local anesthesia [4].
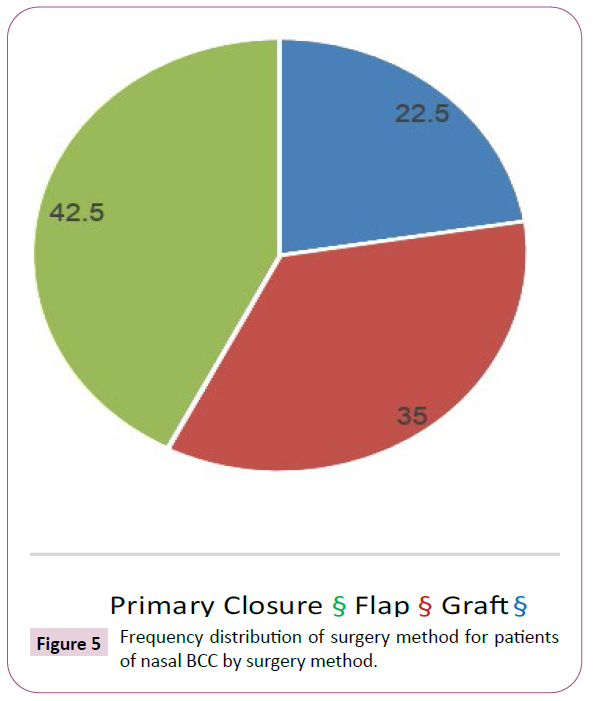
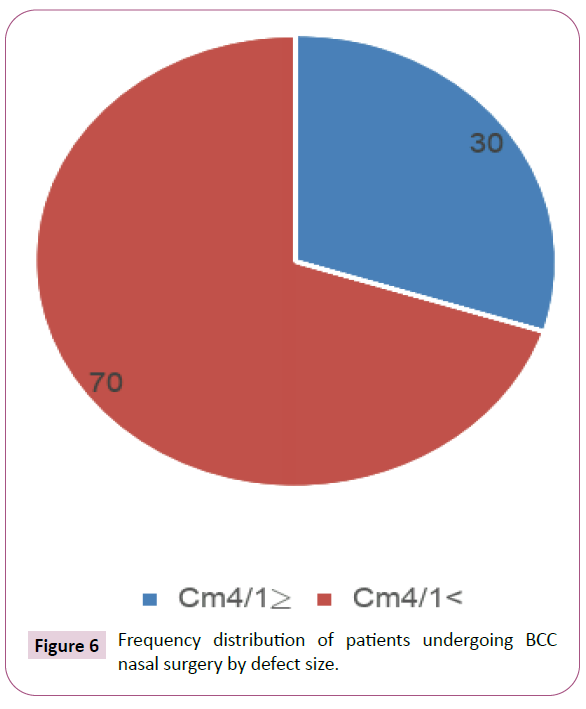
A total of 24 patients out of 80 (30%) had defects smaller than 1.4 and 56 patients (70%) had defects larger than 1.4. 18 patients (22.5%) had skin graft s, 28 patients (35%) had skin flaps and 34 patients (42.5%) had primary closure. In order to assess patient satisfaction, first a questionnaire was prepared in which three sections discussed patient’s appearance, nasal function and respiratory function in the form of three questions.
• Patient appearance was segmented into three states and the related code was allocated: Good (3) Medium (2) and Bad (1).
• Nasal function was segmented into three states and the related code was allocated: Good (3) Medium (2) and Bad (1).
• Respiratory function was segmented into three states and the related code was allocated: Good (3) Medium (2) and Bad (1).
Patients with points 3 to 5 were put in the dissatisfied group, those with points 6 to 7 in the semi-satisfied group and those with points 8 to 10 in the satisfied group.
In order to assess aesthetic considerations, plastic surgery was used. Plastic surgery is assessed according to 5 criteria including contour and board in color change, scarring, retraction and rotation of nose. Each criterion has 2 points.
On this basis patients with 5 to 7 points were placed in the ugly (unbeautiful) group and patients with 8 to 10 points in the beautiful group.
Finally, in order to assess tumor recurrence, three criteria were studied including bumps and depressions of margins, creation of new texture, and creation of new wound.
On this basis patients with 3 to 4 points had recurrence and patients with 5 to 6 points did not have recurrence. The patient questionnaire including satisfaction form and the aesthetic consideration form was completed at the 4th week and 6th months after nasal reconstruction operation.
Patients’ photos were also taken before and after operations.
Results and Findings
Studied data were analyzed using observation method and patients’ checklist using SPSS 23 software and by employing nonparametric tests related to intervention group.
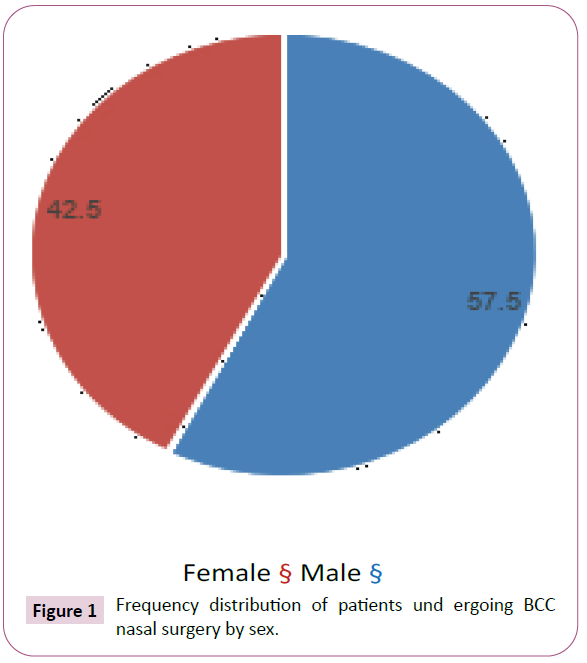
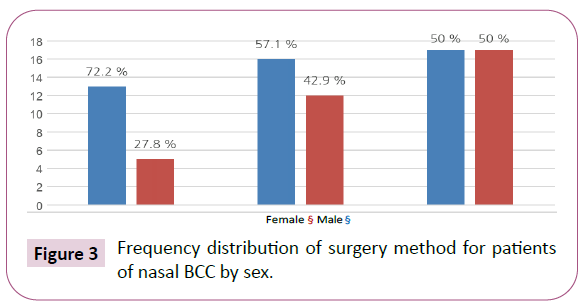
Figure 1 shows frequency distribution of patients undergoing BCC nasal surgery by sex as well as frequency distribution of surgery method of patients undergoing BCC nasal surgery by sex is explained. Overall, out of 80 patients suffering from BCC nasal cancer, 46 patients (57.5%) were male and 34 patients (42.5%) were female. The most common used method in BCC nasal reconstruction in men and women was primary closure (50%) and the least common method used in BCC nasal reconstruction in men and women was skin grafts for 72.2% and 27.8% respectively.
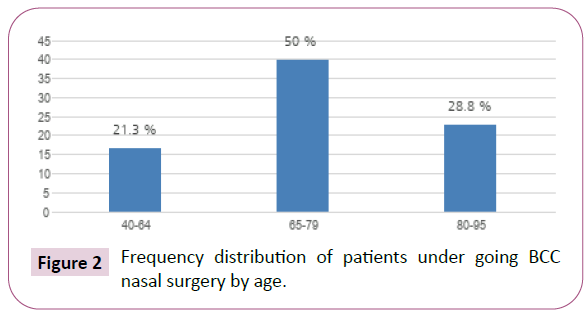
Figure 2 shows frequency distribution of patients undergoing BCC nasal surgery by age as well as frequency distribution of surgery method of patients undergoing BCC nasal surgery by age is explained. Generally out of 80 patients suffering from BCC nasal cancer, the highest frequency is in age group 65-79 with 40 persons (50%) and the lowest frequency was in age group 80-95 with 23 persons (28.8%).
• In age group 40-64 the highest frequency of surgery method is primary closure with 10 persons (29.4%) and the least commonly used method is graft with 3 persons (16.7%).
• In age group 65-79 the most common surgery method is primary closure with 18 persons (52.9%) and the least common method is graft with 7 persons (38.9%).
• In age group 80-95 the most common surgery method is graft with 8 persons (44.4%) and the least common method is primary closure with 6 persons (17.6%).
Figure 3 shows frequency distribution of patients undergoing BCC nasal surgery by sex as well as frequency distribution of surgery method of patients undergoing BCC nasal surgery by sex is explained. Overall, out 80 patients suffering from BCC nasal cancer, 46 patients (75.5%) were men and 34 patients (42.5%) were women. The most commonly used surgery method in BCC nasal reconstruction in men and women is primary closure (50%). The least common surgery method in BCC nasal reconstruction in men and women is graft with 75.5% and 27.8% respectively.
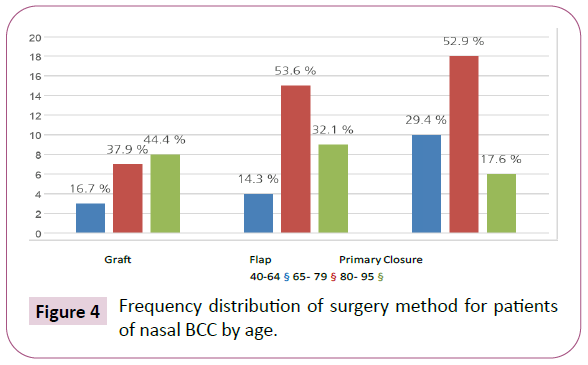
Figure 4 shows frequency distribution of patients undergoing BCC nasal surgery by age as well as frequency distribution of surgery method of patients undergoing BCC nasal surgery by age is explained. Overall, out of 80 patients’ suffering from BCC nasal cancer, the highest frequency is in age group 65-79 with 40 persons (50%) and the lowest frequency is in age group 80-95 with 23 persons (28.8%).
• In age group 40-64 the highest frequency of surgery method is primary closure with 10 persons (29.4%) and the least commonly used method is graft with 3 persons (16.7%).
• In age group 65-79 the most common surgery method is primary closure with 18 persons (52.9%) and the least common method is graft with 7 persons (38.9%).
• In age group 80-95 the most common surgery method is graft with 8 persons (44.4%) and the least common method is primary closure with 6 persons (17.6%).
Figure 5 shows frequency distribution of patients undergoing BCC nasal surgery by surgery methods. Based on this figure the most commonly used surgery method in nasal reconstruction is primary closure with 34 persons (42.5%) and the least common surgery method in nasal reconstruction is graft with 18 persons (22.5%).
Figure 6 shows frequency distribution of patients undergoing BCC nasal surgery is shown by size of defect. Based on Figure 6 the highest frequency is for excision resulting defects larger than 1.4 cm which amounts to 56 persons (70%) and defects with sizes smaller than 1.4 cm are about 24 persons (30%).
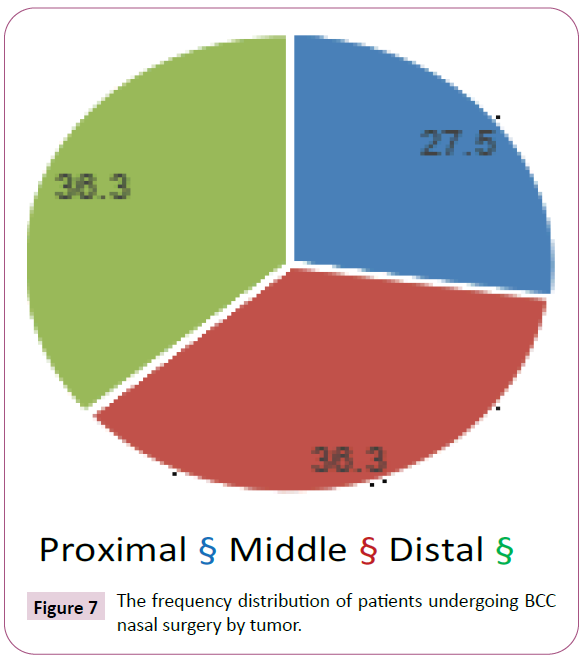
Figure 7 shows frequency distribution of patients undergoing BCC nasal surgery is shown by tumor location. Based on Figure 7 the highest frequency of nasal BCC in the middle and distal part is 29 persons (36.3%) and 29 persons (36.3%) respectively, and the least frequency of nasal BCC is in 1/3 nasal proximal with 22 persons (27.5%). In other words the most common location of nasal BCC in our study is in middle and distal part and the least is in proximal part.
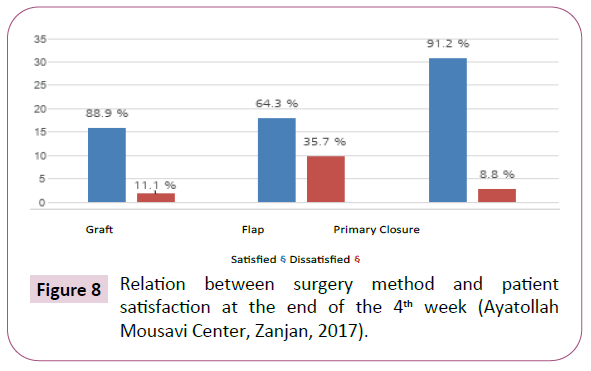
Figure 8 shows relation between the surgery methods used for nasal reconstruction with patient satisfaction at the end of 4th week is studied. According to this figure at the end of the 4th week out of 18 patients undergoing reconstruction by graft method, 16 patients (88.9%) were satisfied. From 28 patients undergoing reconstruction by flap method, 18 persons (64.3%) were satisfied and 10 persons (35.7%) were dissatisfied and out of 34 patients undergoing reconstruction by primary closure 31 persons (91.2%) were satisfied and 3 persons (8.8%) were dissatisfied. Based on this figure it can be said that the least patient satisfaction was indicated in flap method at the end of 4th week and using chisquare test with P. value of 0.017 this relation is meaningful.
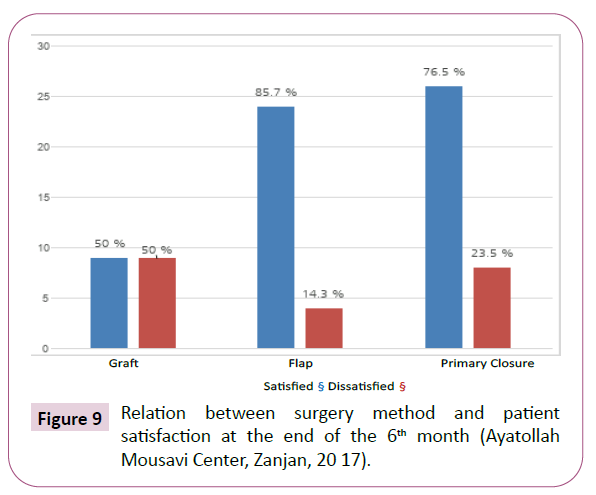
Figure 9 shows relation of surgery method with patient satisfaction at the end of the 6th month is shown. According to this figure out of 28 patients undergoing reconstruction by flap method, 24 persons (85.7%) were satisfied at the end of the 6th month period. 40 persons (14.3%) were dissatisfied but at the end of the 6th month period out of 18 patients undergoing reconstruction by graft method, 9 patients (50%) were satisfied and 9 patients (50%) were dissatisfied and this was the highest level of satisfaction among patients over 80 years. Satisfaction level for primary closure at the end of the 6th month included 26 satisfied persons (76.5%) and 8 dissatisfied persons (23.5%). This relation using chi-square test with a 0.024 P-value was meaningful.
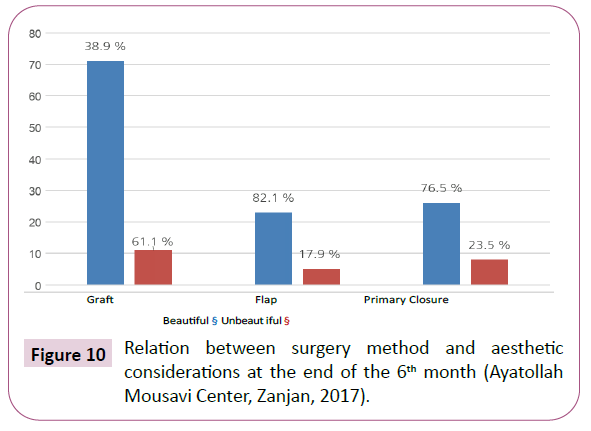
Figure 10 shows relation between surgery methods with aesthetic considerations at the end of 6th month is shown. According to the opinion of a plastic surgeon the highest beaut y was achieved in flap method with 23 persons out of 28 (882.1%) and the lowest beauty in graft method with 7 persons out of 16 (38.9%). It should be ment ioned that the graft used in these 2 persons was in the area of ala nasal. Out of the 34 patients undergoing construction by primary closure method 26 patients (76.5%) were put in the ‘ beaut iful group’ and 8 persons (23.5%) in the ‘unbeautiful group’ and using the chi-square test with a P-value less than 0.05 (P-value =0.004) this relation was meaningful.
Out of 80 patients undergoing BCC nasal surgery in our center no patient had any recurrence. It should be mentioned that 2 patients with BCC were lateral 1/3 middle and lateral 1/3 distal and in the previous center they underwent reconstruction with primary closure method and finally the tumor was excised with more majoring in our center and were reconstructed by flap method.
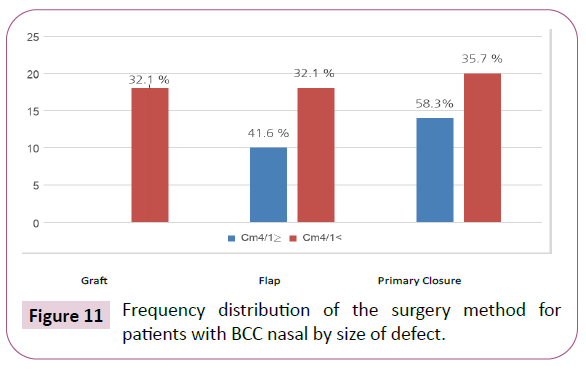
Figure 11 shows frequency distribution of the surgery method for patients with BCC nasal is shown by size of defect. Based on this figure the highest frequency of surgery method were in defects bigger than that of 1.4 cm using flap or graft method with 36 patients out of 56 patients which is equal to 64.2% and the lowest frequency of the surgery method used in defects bigger than 1.4 cm was primary closure method with 20 patients out of 56 equal to 35.7%.
In defects less than or equal to 1.4 cm, the most frequently used method of reconstruction was primary closure with 14 patients out of 24 patients (58.3%). In defects less than or equal to 1.4 cm the least frequent method of reconstruction was graft and it was not used for any patient with this size. In defects equal to and less than 1.4, flap was used for 10 patients (41.6%).
Table 1 shows frequency distribution of the surgery method for patients with BCC nasal is shown by the location of tumor. Based on this table the highest frequency of surgery method in 1/3 distal reconstruction was flap (10 persons equal to 12.5%) and among the flaps the most common one was the bilobed flap. In 1/3 distal the least common method was graft (5 persons equal to 6.25%). In 1/3 middle the most common reconstruction method was flap (16 persons equal to 20%) and the least common was graft with 7 persons (8.75%). In 1/3 proximal the most common method is primary closure (17 persons equal to 21.25%) and the least common was flap (2 persons equal to 2.5%).
| Status | 1 /3 Distal | 1/3 Middle | 1/3 Proximal |
|---|---|---|---|
| Method | (No. â?? Percent) | (No. â?? Percent) | (No. â?? Percent) |
| Primary closure | 8- 10% | 9- 11.25% | 17-21.25% |
| Flap V-Y | 2- 2.5% | 12- 15% | -- |
| Nasolabial flap | 2- 2.5% | 3- 3.75% | -- |
| Bilobed flap | 5- 6.25% | 2-2.5% | |
| Limberg, Forehead, Glabellar flap | 1- 1.25% | 1- 1.25% | -- |
| Graft | 5- 6.25% | 7- 8.75% | 6-7.5% |
Table 1: Frequency distribution of the surgery method for patients with BCC nasal by the location of tumor.
In this study 20 patients out of 100 patients with nasal cancer were omitted from the study due to SCC and vascular diseases and for using immunosuppressors and diabetes, vascular diseasesand collagen diseases. Out of 80 patients suffering from nasal BCC, 56 persons had defects resulting from tumor excision larger than 1.4 cm; our selected method for most of the patients with defects larger than 1.4 cm was flap and graft. It should be ment ioned that in defects larger than 1.4 cm in loose skin or skin that reached each other with undermining, primary closure method was used instead of flap or graft. In 56 patients (70%) the size of defect was larger than 1.4 cm of which 36 persons (64.2%) underwent flap or graft surgery and 20 persons (35.8%) underwent reconstruction with primary closure method. Out of 80 patients suffering from nasal BCC, in 24 persons defects resulting from tumor excision were less than or equal to 1.4 cm and our selected method for most of the patients with defects equal to or smaller than 1.4 cm was primary closure method. It should be ment ioned that in defects with equal to or smaller than 1.4 cm with thick and firm skin, flap was used instead of primary closure. In 24 patients (30%) the size of defect was equal to or less than 1.4 cm of which 14 patients (58.3%) underwent reconstruction with primary closure method and 10 persons (41.7%) underwent reconstruction by flap method.
In the present study the highest prevalence of nasal BCC cancer was in men (57.5%). The highest incidence of nasal BCC cancer was in the age range of 65-79. The most common surgery method was primary closure (42.5%). The least common surgery method was graft (22.5%). The most common method used for young people (under 65 according to WHO) is primary closure method (29.4%) and the least common method in young people is graft (16.7%). The most commonly used method in the elderly (over 65) is flap and primary closure (60%). In general the highest amount of grafts were used in the elderly (18.75%); this may be due to the presence of accompanying comorbidities in the elderly and necessity of short operating time and worrying less about the undesirable appearance in these people. The highest prevalence was in defects larger than 1.4 cm (70%). The most frequent distribution of tumors in 1/3 middle and 1/3 distal was 36.3% with equal frequency. The highest level of satisfaction of patients at the end of 4th week was 88.9% for graft, and 91.2% for primary closure and the lowest level of satisfaction at the 4th week was for flap (64.3%) (P. value < 0.001) Maybe this minimum satisfaction in flap results from more excisions of flap in comparison with the other two methods of graft and primary closure (Figure 12).
The highest level of patient satisfaction at the end of the 6th month period was for flap (85.7%) and primary closure (76.5%), and the lowest level was for graft (50%) (P. value < 0.05) the reasons for less satisfaction of patients at the end of 6th months in primary closure in comparison with flap, can be considered the higher expectations of patients with respect to surgery results and rotation of nose tip and creation of dogear (Figure 13).
It can be said that although the graft method satisfies patient s in the short term, but in the long term it is not a suitable method due to the unfavorable appearance. Generally, a skin graft is not an ideal alternative for coverage of nasal defects since such grafts may create a patchy appearance and scar contracture. Although using grafts, due to the ease of work and less use of skin excisions in comparison with flaps are accompanied with maximum satisfaction in the short term but in long term it is accompanied with very unpleasant results relating to the patchy appearance. It should be mentioned that in our research only 2 patients were satisfied with their grafts and the graft s were applied in all nasal area. The best achievement of beaut y taking into mind the aesthetic considerations at the end of the 6th month was in flap and primary closure that was surprisingly more than grafts (96.4% against 76.5%) and the least achievement of beaut y at the end of the 6th month was for grafts (11%). In our study performed on 80 patients suffering from nasal BCC that underwent tumor excision and nasal reconstruction by flap, graft and primary closure methods at the end of the 6th and 19th month, no recurrence was seen including creation of new soft tissue, new wounds and protrusion and depression of the margins [5]. After surgery only 2 patients suffered from hematoma and 1 patient suffered from ischemia of the tip of the flap and it was recovered by secondary intentions. Only 2 patients had recurrence of nasal BCC in the 1/3 middle and distal area s resulting from reconstruction by primary closure in another center and they were referred to our center. These 2 patients underwent repeated excision and reconstruction through flap method with more majoring (Figure 14).
In the current study we surprisingly came to the result that in the long term, reconstruction with flap method in comparison with graft and primary closure, had brilliant results in terms of satisfaction and beaut y after the sixth month, and this relation was meaningful using the chi-square test with p-value of 0.05.
In addition using grafts, due to the patchy appearance and scar contracture is not an ideal alternative for skin coverage of nasal defects although in specific cases such as cant us and alar area they accompanied by good aesthetic results.
Discussion
One of the most important limitations was that we had to include patients with pure non melanoma nasal skin cancer not involving other parts of t e face and body, so leading to decrease number of sample size. The second limitation was due to lack of closed patient observation as for some of them were living in not easily accessible rural areas. We could be able to overcome these hardships with closed relation and consult to pathologists and dermatologists to select those specific cases and also obtain Patients and their relatives telephone numbers to access them easily for long term follow-up.
In the study of Rorich et al. [6] the average age of patients suffering from nasal basal cell cancer was 51, while in our study the average age of patients was 71. In the study of Rorich, the common location of tumors was in the nasal distal but in our study it was in the middle and distal sections with equal distribution. In their study 1.9% of patients had recurrence, but in our study no recurrence was seen and this may be due to the emission of squamous cell cancer from our study.
In the study of Singh et al. [7] 219 patients underwent nasal reconstruction and the aesthetic and functional results of 85 percent of those were exceptional, 13% good, and in 2 percent medium and weak aesthetic results were not mentioned, but in our study the lowest patient satisfaction was for flap method at the end of 4th week.
In the study of Arden et al. [8] using melolabial island plaques in all skin types was lacking in the nasal alar area. Following nasal cancer surgery resulting in decreased scarring and the achievement of desired result from an aesthetic point of view. In our study, the least beaut y at the end of the 6th month was gained in graft and the highest beaut y, which correlates to Arden’s study, was achieved in flap method (87.1%).
In the study of Han et al. [9] on 18 patients that underwent nasal alar reconstruction with flap, 5 patients (29%) were very satisfied, 10 patients (59%) were satisfied, 1 patient (6%) had relative satisfaction and 1 patient was dissatisfied (6%); while in our study on 28 patients undergoing reconstruction with flap method, at the end of the 6th month, 24 patients (85.7%) were satisfied and only 4 patients (14.3%) were dissatisfied of those that underwent reconstruction with graft method and at the end of the 6th month 9 patients (50%) were satisfied and 9 patients (50%) dissatisfied and the highest satisfaction rate from graft s was in patients over 80. Satisfaction from primary closure method at the end of the 6th month, included 26 patients who were satisfied (76.5%) and 8 patients who were dissatisfied (23.5%) but at the end of the 4th week the least satisfaction was from flap with 10 dissatisfied persons (35.7%) and the satisfaction at the end of the 4th week was related to primary closure method (91.2%) and the reason of low satisfaction at the end of the 4th week may be attribut ed to numerous incisions in comparisonwith the previous two methods.
The study of Han et al. [10] correlates with the present study in that the amount of satisfaction and achievement of aesthetic considerations was at the lowest possible amount in grafts and in order to overcome these problems, Han et al. used a specific technique to excise the superficial epithelial layer in relatively thick skin grafts called dermis grafts that had satisfactory results both in function and in aesthetic matters.
Conclusion and Suggestions
Taking into consideration the fact that our study results were meaningful according to patient satisfaction level and achieving aesthetic considerations with the flap method in comparison with the two methods of graft and primary closure, since reaching borders without tumors and acquiring pleasant and desirable aesthetic results, are of fundamental concern in nasal reconstruction. It is suggested that in small excised tumors in which the resulting defect is equal to or smaller than 1.4 cm, in order to prevent recurrence of tumor, in future, instead of excising majoring 2 mm or less, from the very beginning of the treatment bigger majoring (4 mm or more) and reconstruction with flap method is carried out instead of primary closure.
Acknowledgment
The authors of the present article would like to express their utmost gratitude to the Research and Technology Deputy of Zanjan University of Medical Sciences.
References
- Rifaat MA (2013) Reconstruction of composite defects of the nose following tumor resection: a single author’s experience and evaluation of the outcom. Chin Ger J Clin Oncol 12: 427-434.
- Yeh JM, Ou CY, Lee JYY, Wong TW (2013) Secondary intention healing with satisfactory outcome after nodular basal cell carcinoma excision on the face. Dermatol Sin 31: 68-72.
- Jin HR, Jeong WJ (2009) Reconstruction of nasal cutaneous defects in Asians. Auris Nasus Larynx 36: 560-566.
- Rohrich RJ, Griffin JR, Ansari M, Beran SJ, Potter JK (2004) Nasal Reconstruction? Beyond Aesthetic Subunits: A 15-Year Review of 1334 Cases. Plast Reconstr Surg 1405-1416.
- Baj A, Russillo A, Segna E, Romano M, Bolzoni A, et al. (2017) Nasal reconstruction: our experience. J Biol Regul Homeost Agents 31: 169-174
- Rohrich RJ, Pessa JE (2007) Reconstruction of composite defects of the nose following tumor resection: a single author’s experience and evaluation of the outcome. Plast Reconstr Surg 119: 2219-2227.
- Singh DJ, Bartlett S (2010) Aesthetic Considerations in Nasal Reconstruction and the Role of Modified Nasal Subunits. Plast Reconstr Surg 111: 639-648.
- Arden RL, Miguel GS (2012) The subcutaneous melolabial island flap for nasal alar reconstruction: A clinical review with nuances in technique. Laryngoscope 122: 1685-1689.
- Han DH, Mangoba DCS, Lee DY, Jin HR (2012) Reconstruction of Nasal Alar Defects in Asian Patients. Arch Facial Plast Surg 14: 312.
- Han SK, Yoon WY, Jeong SH, Kim WK (2012) Facial dermis grafts after removal of basal cell carcinomas. J Craniofac Surg 23: 1895-1897.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences