Concomitant Abdominal Procedures with Abdominoplasty �?? Patient Selection and Principles to Avoid Complications
Kushal Monga * and Pradeep Goil
Department of Plastic Surgery, SMS Hospital, Jaipur, Rajasthan, India
- *Corresponding Author:
- Dr. Kushal Monga
Department of Plastic Surgery
SMS Hospital
Jaipur, Rajasthan, India
Tel: +919829111048
E-mail: mongakushal87@gmail.com
Received Date: May 19, 2021; Accepted Date: June 15, 2021; Published Date: June 22, 2021
Citation: Monga K, Goil P (2021) Concomitant Abdominal Procedures with Abdominoplasty – Patient Selection and Principles to Avoid Complications. J Aesthet Reconstr Surg Vol.7 No.4:30.
Abstract
Background: Combining abdominal surgeries with an abdominoplasty procedure can be done safely to achieve better outcomes in terms of early recovery, cost effectiveness, single hospitalisation and better cosmetic outcomes. Many patients coming to a general surgeon’s practice who have a pendulous abdomen should be given an option of having a concomitant surgery, which involves a panniculectomy.
Methods: We present 12 patients that underwent combined abdominoplasty with various intraabdominal procedures from January 2018 to January 2020 and followed up for 1 year.
Results: One patient had a wound infection that required drainage and antibiotics. Four patients had minor complications. Patients' satisfaction with the functional and cosmetic outcome of combined procedures has been impressive.
Conclusion: Our experience confirms the basic safety of the combined surgery when done on appropriately selected patients.
Keywords
Abdominoplasty; Intraabdominal; Hernia
Introduction
Abdominoplasty was initially described by Demars and Marx in 1890 [1]. Back then, indications for abdominoplasty were few and removing the umbilicus was also seen to be impossible. So it did not gain much popularity. Later advances were made and in 1905, preserving the umbilicus became possible [2]. But then also, abdominoplasty was restricted to use in injury wounds in World War 1 era. Slowly the expectation and demands of people have grown so that the operation is usually performed primarily for aesthetic reasons, popularly called tummy tuck procedure. The present day abdominoplasty consists of panniculectomy, repair of the musculofascial layer and undermining and advancement of upper abdominal flap. Combined use of liposuction with abdominoplasty has gained much popularity in present times. Hence, the indication of abdominoplasty has evolved over time [3-5]. In present day scenario, patients as well as surgeons hope to combine multiple surgeries in one sitting, thereby reducing hospital stay, recovery time and the financial costs are also reduced. In our view, all patients coming to a general surgeon or a gynaecologist for an elective intraabdominal procedure with a pendulous abdomen should be offered an option of abdominoplasty for better aesthetic outcomes. This study presents our experience of combining various intraabdominal procedures with abdominoplasty. Our study goes out to reveal that in selected patients and with experienced surgeons, this approach of combining multiple surgeries is very rewarding and advantageous with comparable complication rate.
Materials and Methods
Study was designed having 12 patients with an intraabdominal pathology diagnosed clinically and/or on ultrasound scan willing to undergo the primary procedure and seeking treatment of their sagging abdomen. Time period was from January 2018 to January 2020. Adequate ethical approval was taken from the institutional ethics committee. All patients having comorbidities like uncontrolled diabetes, hypertension, coronary artery diseases and history of thromboembolic episodes were excluded. Smokers were asked to refrain from smoking 2 weeks prior to surgery. All patients were followed up for 1 year for any complications.
Surgical technique
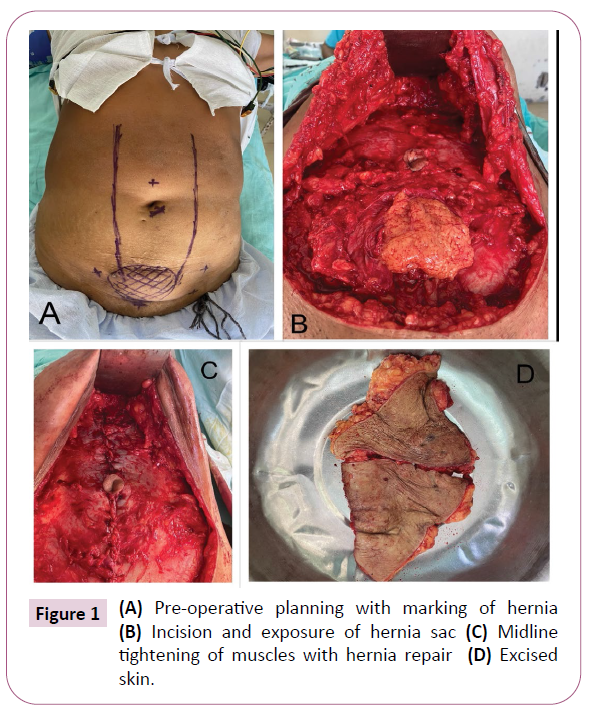
Preoperative ultrasound to look for intrabdominal pathology and to identify the margins of incisional hernia sac, when present, was done for planning purposes. Figure 1A shows preoperative planning for an incisional hernia sac dissection in the lower abdomen. The laxity of the lower abdomen was checked with the pinch test to identify how much amount of extra skin to be excised in the lower abdomen without tension. If the patient has undergone previous lower abdomen surgery, the scar was included in the tissue to be resected. Standard lower abdomen horizontal incision is given with bevelling towards the part to be resected. After the skin incision, flap with skin and subcutaneous tissue is elevated at the level of the anterior abdominal wall fascia. The umbilical stalk is freed from the flap by giving a circumferential incision around the umbilicus with bevelling outwards to safeguard the umbilical vascularity. Laterally skin flap is raised 10 cm beyond the lateral border of the rectus abdominis muscles on each side. The hernia sac, if present, is separated from the flap and the margins of the sac identified in the anterior abdominal wall. Figure 1B shows abdominal contents coming out after the hernia sac, after it has been dissected off from the skin flap. The flap dissection is carried upwards towards the xiphoid process in the midline and costal margins on the side, giving an inverted V shaped anterior abdominal wall exposure and safeguarding the perforators supplying the abdominal flap. After the flap elevation, the exposure for secondary procedure is planned. In case of lower abdominal hernia, sac is opened and intrabdominal procedure is carried out, if indicated. Later the hernia sac is closed and an onlay mesh repair is done for lower abdominal hernia repair. Figure 1C shows repair of the anterior abdominal wall and midline continuous prolene sutures to tighten the rectus muscles as a standard abdominoplasty procedure. Hernia site reconstituted with a prosthetic mesh. In cases where there is no intraabdominal pathology, sac is not opened; herniorhaphy followed by onlay mesh plasty is done. In 2 cases, a lower midline incision was given in the anterior abdominal wall fascia, after the skin flap elevation to enter the abdomen, followed by hysterectomy by gynaecology colleagues. Similarly, in cases of open cholecystectomy, upper midline incision in the fascia was given for entering the abdomen and cholecystectomy was done by general surgery colleagues. Closure was done in layers. Closure of peritoneum was done by continuous absorbable sutures, while the incision in the aponeurosis was closed by interrupted prolene 2-0 sutures. In one case, laparoscopic cholecystectomy was done with standard 4 port surgery but the ports were made in the anterior abdominal wall fascia after the skin flap has been raised. This technique had no scars on the abdomen and is a modification of the technique used by Prasad et al, who termed it as scar less cholecystectomy [6].
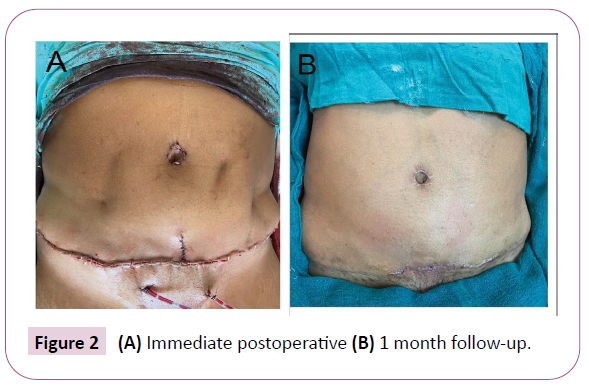
The degree of rectus diastasis is identified and tightening of the rectus abdominal wall is carried out by plication of rectus abdominal muscles by prolene 2-0 continuous interlocking sutures and buried at the end of the knot as shown in Figure 1C. The skin flap is draped over the abdomen and umbilicus is exteriorised in its new position by making a button hole in the flap. The distal extra skin of the flap is excised (Figure 1D) and closure done in layers after placing 2 negative suction drains beneath the flap (Figure 2). Drains are removed on the 6th day.
Patients are asked to ambulate 24 hours after surgery albeit with an abdominal binder which should be used for a minimum of 3 months postoperatively.
Results
Patients included in the study had a mean age of 51 years (range- 30-65 years) and all were females. All patients along with their indication are shown in Table 1. Most commonly performed surgery along with abdominoplasty was incisional hernia repair for a previous incision in the lower abdomen [6] and in the epigastric region [1]. Laparoscopic cholecystectomy was done in 1 case while open cholecystectomy was done in 2 cases. 2 patients underwent hysterectomy via the same abdominoplasty approach. All patients were followed up for a period of 1 year and there was no recurrence of hernia. However, there was infection in 1 case which required going back to the theatre, cleaning the wound of all debris and secondary suturing after the infective process had terminated. There were minor complications in 3 cases where there was a marginal skin change but they ultimately settled without any intervention. No incidence of seroma or hematoma was seen. Table 1 also shows complications seen in the study.
| S. No. | Primary approach | Second procedure | Third procedure | USG finding/indication | Complications |
|---|---|---|---|---|---|
| 1 | Abdominoplasty | Incisional hernia repair (previous pfennensteil incision) | Ventral hernia | Marginal changes | |
| 2 | Abdominoplasty | Incisional hernia repair (right paramedian incision) | Appendicectomy | Ventral hernia with subacute appendicitis | - |
| 3 | Abdominoplasty | Incisional hernia repair (paramedian) | Ventral hernia | Infection at suture line (debridement and secondary suturing done at a later time) | |
| 4 | Abdominoplasty | Epigastric hernia repair | Cholecystectomy | Ventral hernia with cholelithiasis | - |
| 5 | Abdominoplasty | Hysterectomy | Fibroid uterus | - | |
| 6 | Abdominoplasty | Incisional hernia repair | Ventral hernia | Marginal changes | |
| 7 | Abdominoplasty | Incisional hernia repair | Ventral hernia | - | |
| 8 | Abdominoplasty | Hysterectomy | - | ||
| 9 | Abdominoplasty | Incisional hernia repair | Appendicectomy | Ventral hernia with subacute appendicitis | - |
| 10 | Abdominoplasty | Lap Cholecystectomy (scarless) | cholelithiasis | - | |
| 11 | Abdominoplasty | Cholecystectomy | cholelithiasis | Marginal changes | |
| 12 | Abdominoplasty | Cholecystectomy | cholelithiasis | - |
Table 1: Combined procedures with Abdominoplasty with complications.
Discussion
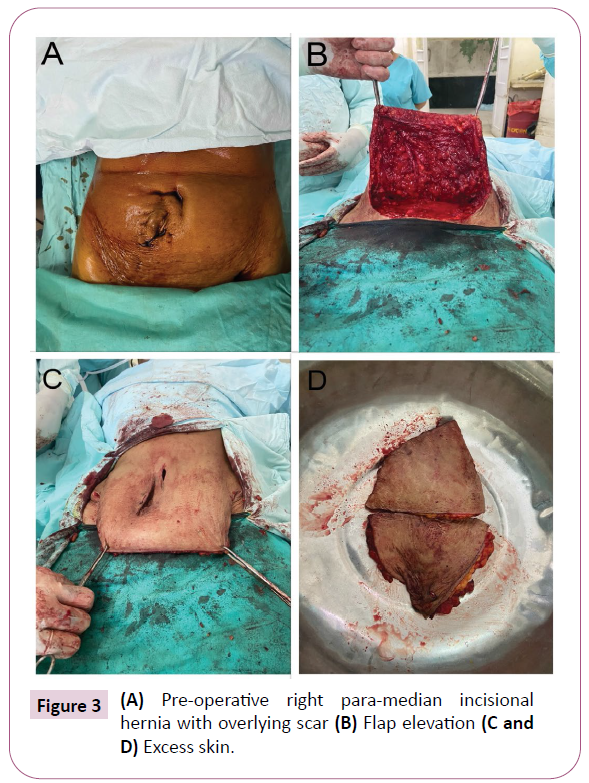
Abdominoplasty is a very commonly performed procedure these days whose indications have evolved from reconstructive to present day cosmetic purposes. Lot of patients undergoing standard elective intraabdominal surgeries are demanding better cosmetic outcomes with minimal scar and early return to work. In this scenario, patients can be offered this approach of performing an intraabdominal procedure along with removal of excess and sagging lower abdominal skin. Advantage of combining these procedures is sparing the patient of a second surgery and thus less downtime away from work, single recovery period and reduction in risk involved with anaesthetic drugs. The cost effectiveness cannot be stressed upon more both for the patient and the hospital. Most importantly, the satisfaction level of patient is very high as abdominoplasty improves quality of Life, lessens the psychological distress of having a floppy lower abdomen and better self-confidence (Figure 3).
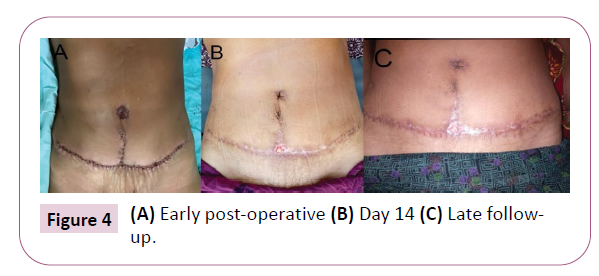
Incisional hernia repair is the most commonly performed procedure in conjunction with abdominoplasty. In all cases of incisional hernia in the lower abdomen, the previous scar was excised and replaced by new tissue recruited from above, which is essentially a full thickness flap comprising skin and subcutaneous tissue. Thus it had good healing and good long term prognosis than a repair which left the same previously operated damaged skin over a prosthetic mesh for abdominal wall repair. We attribute this as a reason for not having a recurrence along with use of a mesh for reconstituting the hernia repair done by interrupted sutures. Figure 4 shows end result after incisional hernia repair has been done and healthy full thickness flap are covering the hernia site. The technique of mesh repair whether sublay or onlay doesn’t have significant difference in results as has been depicted in the study conducted by Iljin A et al. [7]. Our method of approach is an onlay mesh repair because it avoids tedious dissection and is less time consuming.
In all cases of cholecystectomy (laparoscopic and open), we were able to achieve best cosmetic result wherein there was no scar in the upper abdomen, leading to better patient satisfaction. In a technique described in the study by Prasad et al. [6], all 4 ports were put in the lower abdomen skin which was resected later on. The disadvantage of this method is that the ports are much away from the operation site (gallbladder). Consequently, the viewing angle is slightly changed and room for the instrument maneuvering is less. Therefore, they advised extreme caution with a low threshold to put an extra port in the upper abdomen in case of any undue technical difficulty. Our technique is a modification of the technique, where we raise the abdominal flap till xyphoid process and costal margins in all the cases, which makes putting all 4 ports as per standard technique possible and still have a scarless end result.
In cases where hysterectomy was done, patient satisfaction was termed good as there was a single horizontal incision in the lower abdomen which would be hidden under clothing of females.
Although there are potential advantages in combining procedures, the surgeon’s primary concern should be the safety of patients. Voss et al. [8] reported an incidence of pulmonary embolism in 6.6% of his cases after abdominoplasty combined with gynaecological procedures. Similarly, Savage [9] reported pulmonary embolism in 1 out of 13 patients who had underwent abdominoplasty with hysterectomy. However, in our study there was no incidence of pulmonary embolism. This is attributed to patient selection. We had chosen patient who did not have any comorbidities. Smokers were asked to stop smoking for 2 weeks prior to surgery.
Some studies have demonstrated a risk to the vascularity of umbilical stalk while doing abdominoplasty [10-12]. The vascularity to the umbilical stalk is from superficial and deep sources. Superficial source is from the subdermal plexus which is disrupted while doing a circumferential incision around the umbilicus. Deep branches come from the deep inferior epigastric arteries that ascend just posterior to the rectus abdominis [13]. These branches anastomose with the branches from the opposite side. In our opinion, if the dissection is above the anterior rectus sheath, then vessels from the deeper system to the umbilical stalk will not get damaged from either side. This is to be attributed as the reason for no incidence of umbilical stalk ischemia in our study. One exception to this is umbilical hernia, where the deep supply to the umbilicus is uncertain and thus should be dealt with precaution. We recommend separate surgeries in such cases to avoid irreversible damage to the umbilicus. A laparoscopic approach to periumbilical hernia (intraperitoneal onlay mesh- IPOM) repair after the abdominal flap has been raised can be done as it spared the surgical insult to the anterior rectus sheath and thus preserving the deep blood supply to the umbilicus. However, this technique has not been tried by authors so far and is something to look forward to in future.
Simultaneous ventral hernia repair with abdominoplasty can be performed through either a vertical or a horizontal incision. Many of the hernia patients already have a midline incision which can be excised at the time of meticulous closure. According to Cheesborough et al. [14], the vertical incisions minimize skin undermining and improve the torso hourglass shape.
Various authors have described the use of a vertical abdominoplasty technique with open hernia repair. The technique involves a midline incision to raise an abdominal flap followed by an infraumbilical incision through the linea alba for hernia identification, reduction, and repair [15] However, this technique comes with its share of postoperative complications, which have been reported to occur in up to 40% in the study by Bruner TW et al, and the operation results in a large vertical scar from the xiphoid to the pubis [14,16].
Also, in hairy individuals, there are chances of hair being present in the area of neoumbilicus creation, which can hamper the healing process, which is not much of an issue with the standard horizontal lower abdomen incision. The standard low horizontal incision is easier to camouflage but comes at the cost of Greater skin flap elevation. Even though it is well established that repair of hernias with mesh is more durable than Suture repair alone, mesh is avoided by many surgeons because of concerns regarding risk of infection, extrusion, pain, and the need for removal of the mesh. But we prefer a mesh repair as it gives least chances of recurrence of hernia in late follow up period [17].
Patients who have had upper abdominal surgery previously like an open cholecystectomy or an upper midline incision should be excluded as in these cases the viability of the undermined abdominal flap is uncertain. In these cases, a vertical abdominoplasty approach would be better, although we don’t advice doing it as a vertical scar in Indian population can be unpleasant and repelling.
Large number of surgeons performing abdominoplasty has accepted that around half of the times they have had to perform an additional procedure while doing abdominoplasty [18]. But no clear guidelines as to proper patient selection and surgical planning have been reported.
Combining procedures can be time consuming and carries a higher risk of complications like deep vein thrombosis but in most cases the morbidity of concomitant surgeries is the same as an abdominoplasty alone [19]. So it is absolutely vital to have an experienced gynaecologist or general surgeon as your contemporary performing these procedures because of unconventional exposure and not so common technique.
We believe that these procedures when done by experienced hands in a tertiary centre with proper selection of patients can be combined and yield much better results than if performed separately. The ideal patient is a multiparous female in fourth decade of her life, with or without a previous lower abdominal surgery scar who demands functional as well as cosmetic outcomes in terms of minimal scar and an hour glass shaped abdomen.
Conclusion
Concomitant abdominoplasty and elective abdominal procedures is not without risk; however, with the proper patient selection and the technique described, this approach is a beneficial option. The good results in our study are attributed to appropriate patient selection and skilful execution of the procedure. Most patients if given such an option will agree to it seeing the functional and aesthetic benefits outweigh the same procedures performed independently with a delay in between. So our general surgeon and gynaecology colleagues should also be educated of this option as primarily the patient will come to their clinic. In our opinion, these procedures can be safely performed concurrently by an experienced team in a tertiary centre with appropriate patient selection yielding better results and reducing perioperative risk to the patient by undergoing only one operation rather than two to achieve the same outcome.
Conflict of Interest
Authors have no potential conflicts of interest.
Funding
Authors have no sources of funding to disclose.
Consent
The patient has given informed consent for the use of nonidentifiable images and case presentation in this manuscript.
References
- Elbag JS, Flageul G (1979) Plastic surgery of the abdomen. New York, Masson, USA. p. 42.
- Murillo WL (2018) Emulation of a Newborn’s Umbilical Scar. Omphaloplasty 105-125.
- De Cardoso CC (1987) Limited incisions in abdominoplasty. Ann Plast Surg 19: 436-447.
- Grazer FM (1973) Abdominoplasty. Plast Reconstr Surg 51: 617-623.
- Psillakis JM (1984) Plastic surgery of the abdomen with improvement in body contour. Clin Plast Surg 11: 465-478.
- Prasad MB, Surapaneni SR, Dabade SS (2012) Scarless cholecystectomy: laparoscopic cholecystectomy with abdominoplasty. Indian J Surg 74: 486-488.
- Iljin A, Antoszewski B, Zieliński T, Skulimowski A, Szymański D, et al. (2019) Sublay or onlay incisional hernia repair along with abdominoplasty: which is better? Long-term results. Hernia 23: 757-765.
- Voss SC, Sharp HC, Scott JR (1986) Abdominoplasty combined with gynecologic surgical procedures. Obstet Gynecol 67: 181-186.
- Savage RC (1982) Abdominoplasty combined with other surgical procedures. Plast Reconstr Surg 132: 165-168.
- Saxe A, Schwartz S, Gallardo L, Yassa E, Alghanem A (2008) Simultaneous panniculectomy and ventral hernia repair following weight reduction after gastric bypass surgery: is it safe? Obes Surg 18: 192-195.
- Ortega J, Navarro V, Cassinello N, Lled S (2010) Requirement and postoperative outcomes of abdominal panniculectomy alone or in combination with other procedures in a bariatric surgery unit. Am J Surg 200: 235-240.
- Le Gall H, Reibel N, De Runz A, Epstein J, Brix M (2017) Abdominoplasty and simultaneous laparoscopic ventral hernia repair. Clinical study about 45 patients. Ann Chir Plast Esthétique 62: 115-121.
- Stokes E, Whetzel T, Sommerhaug E, Saunders C (1998) Arterial vascular anatomy of the umbilicus. Plast Reconstr Surg 102: 761-764.
- Cheesborough JE, Dumanian GA (2015) Simultaneous prosthetic mesh abdominal wall reconstruction with abdominoplasty for ventral hernia and severe rectus diastasis repairs. Plast Reconstr Surg 135: 268-276.
- Bruner TW, Salazar Reyes H, Friedman JD (2009) Umbilical hernia repair in conjunction with abdominoplasty: A surgical technique to maintain umbilical blood supply. Aesthet Surg J 29: 333-334.
- Shermak M (2006) Hernia repair and abdominoplasty in gastric bypass patients. Plast Reconstr Surg 117: 1145-1150.
- Al-Qattan MM (1997) Abdominoplasty in multiparous women with severe musculoaponeurotic laxity. Br J Plast Surg 50: 450-455.
- Pitanguy I (1967) Abdominolipectomy: An approach to it through an analysis of 300 consecutive cases. Plast Reconstr Surg 40: 384.
- Grazer FM (1973) Abdominoplasty. Plast Reconstr Surg Jun 51: 617-623.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences