Efficacy of Scratch Test in Free Flap Monitoring
Sumedha Wadhwa*
Published Date: 2022-09-14Sumedha Wadhwa*
Department of Surgery, Bharati Vidyapeeth Hospital and Research Centre, Pune, India
- *Corresponding Author:
- Sumedha Wadhwa
Department of Surgery,
Bharati Vidyapeeth Hospital and Research Centre, Pune,
India,
Tel: 9711005489;
E-mail: drsumedhawadhwa@gmail.com
Received date: July 06, 2022, Manuscript No. IPARS-22-13970; Editor assigned date: July 11, 2022, PreQC No. IPARS-22-13970 (PQ); Reviewed date: July 25, 2022, QC No. IPARS-22-13970; Revised date: September 06, 2022, Manuscript No. IPARS-22-13970 (R); Published date: September 14, 2022, DOI: 10.36648/2472-1905.8.6.153
Citation: Wadhwa S (2022) Efficacy of Scratch Test in Free Flap Monitoring. J Aesthet Reconstr Surg Vol:8 No:6
Abstract
Introduction: Re-exploration of the failing free lap at the earliest provides the best chance for successful salvage. We describe our experience with scratch test as an adjunct to clinical monitoring that provides quick and reliable results at near negligible cost to monitor the viability of the free lap in the early post operative period.
Materials and methods: A prospective, observational study was conducted from January 2018 to December 2020 on patients undergoing free laps where skin paddle was available for monitoring. Scratch test was performed by making a 2-3 mm horizontal scratch up to the dermis using a 28 gauge needle on the distal aspect of the lap. Bright red coloured blood (appearing between 3-12 seconds) was considered normal, while dark coloured blood (appearing within 3 seconds) or no blood appearing till 12 seconds were considered suggestive of vascular compromise. The scratch test commenced on the operating table immediately a ter completion of lap inset, and continued till 72 hours post-operatively.
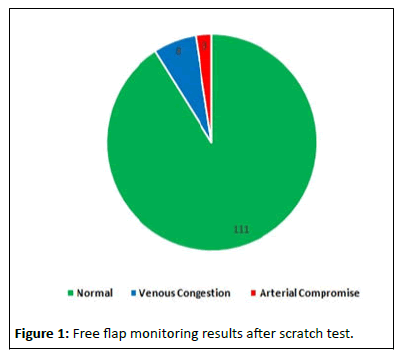
Results: 122 patients were enrolled in the study over the period of 02 years. Scratch test was normal in 111 cases (91%) for initial 72 hours following the surgery. Eleven patients overall (11/122) exhibited features of vascular compromise on scratch test when the clinical examination was either normal or equivocal at that instant. Eight out of these eleven patients (8/11) exhibited features of venous congestion, whereas three patients (3/11) exhibited arterial blockage. All these patients underwent prompt reexploration where the vascular compromise was corrected. Early identi ication helped in complete salvage of six out of eleven compromised laps.
Conclusion: Scratch test has the potential to alert at the earliest for development of vascular compromise preceding the other clinical signs. This may enable re-exploration at the earliest for the higher rates of successful salvage of the failing laps.
Keywords
Free laps; Microvascular tissue transfer; Flap monitoring; Scratch test
Introduction
Free autologous tissue transfer is a versatile treatment modality for managing complex defects and difficult wounds. Initially used widely for post-traumatic reconstruction, free lap transfer has revolutionized the reconstruction of complex defects following cancer resection [1]. Success rate of free laps has been reported to be in the range of 94-99% in most of the high volume institutions across the world [2]. The failure rate of up to 5% that has been reported, though acceptable, is felt to impose great effort, morbidity and cost due to requirement of another surgery to achieve the successful outcome [3]. Monitoring of a free lap during the initial post operative period is vital for keeping a close watch on lap viability and any need for early re exploration [4]. Earlier re-exploration of the free lap (ideally within couple of hours of detecting vascular compromise) translates consistently into higher rates of successful salvage of the lap [5,6]. Commonly, the free lap monitoring is performed by clinical examination supplemented with other adjuncts, both non-invasive and invasive [7]. In our experience, scratch test, as an adjunct to clinical monitoring, provides quick and reliable results at near negligible cost to monitor the viability of the free lap in the early post operative period. We present here our study to assess the role of scratch test as a primary lap monitoring adjunct in free micro vascular transfers.
Materials and Methods
This prospective, observational study was conducted from January 2018 to December 2020 in a tertiary level teaching hospital. All the consecutive patients undergoing free micro vascular tissue transfer for their respective diagnoses where skin paddle was available for the monitoring were included in the study. The patients who needed buried muscle or bone free laps with no skin paddle available for monitoring were excluded from the study. Informed consent for post-operative lap monitoring using scratch test as an adjunct to clinical examination was taken prior to the surgery. The monitoring with clinical examination was performed with the well described parameters namely, lap colour, temperature, lap skin turgor and capillary re ill time [7,8]. Scratch test was performed by making a 2-3 mm horizontal scratch up to the dermis, using a 28 gauge needle on the distal aspect of the lap. The time required for blood to appear was then noted along with the colour of the blood. Bright red coloured blood that appeared between 3-12 seconds was considered normal, signifying satisfactory perfusion of the flap. Dark coloured blood that appeared in less than 3 seconds was considered to be suggestive of problem in the venous outflow, even if there was no discoloration of the flap skin at the time of examination. If blood did not appear till 12 seconds after the scratch, it was considered to be suggestive of compromise of arterial inflow to the flap. The scratch test commenced on the operating table immediately after completion of flap inset, and continued 2 hourly for the first 08 hours, 4 hourly for next 16 hours, and 6 hourly till 72 hours post operatively (total 16 scratches). After 72 hours flap monitoring was completely based on clinical assessment. Based on the results noted after the scratch test, a decision of flap viability was made and appropriate surgical decision taken.
Results
The study accrued 122 patients over the period of 02 years. Male to female ratio was 3.2:1. The youngest patient in the series was 3 years of age and the oldest one was of 88 years. Co morbidities were present in 34 patients, of which 11 patients had two or more co-morbidities, with diabetes and hypertension being the most common (Table 1).
| Number of Patients | 122 | % of patients |
|---|---|---|
| Male | 93 | 76.22 |
| Female | 29 | 23.77 |
| Male to female ratio | 3.2:1 | - |
| Mean age | 48.04 | - |
| Smokers | 69 | 56.55 |
| Co-morbidities Hypertension Diabetes mellitus Coronary artery disease Hypothyroidism Collagen vascular disorders |
34 (11 with two or more co-morbidities) | 27.86 |
| 22 19 11 5 3 |
Table 1: Demographic data of the patients.
Free flaps were performed for various indications, the most common being reconstruction after cancer resection (74%). It was followed by trauma (14%), gunshot wounds, secondary reconstruction of burns, non healing chronic wounds, electric burns and radionecrosis of mandible (Table 2). Free osteo cutaneous fibula flap was used in 58 cases (48%) followed by free anterolateral thigh flap (21%) and free radial artery forearm flap (11%) respectively (Table 3).
| Indication | Number of patients | % of patients |
|---|---|---|
| Post oncologic reconstruction | 89 | 74.16 |
| Trauma | 17 | 13.93 |
| Gunshot wound | 5 | 4.09 |
| Post burn Contracture | 4 | 3.27 |
| Chronic wounds | 3 | 2.45 |
| Electrical Burns | 2 | 1.63 |
| Radio necrosis of mandible | 2 | 1.63 |
| Total | 122 | 100 |
Table 2: Indication of free flap reconstruction.
| Type of free flap | Number of patients | % of patients |
|---|---|---|
| Fibula osteocutaneous | 58 | 47.54 |
| Anterolateral thigh | 26 | 21.31 |
| Radial artery forearm | 14 | 11.47 |
| Gracilis muscle | 8 | 6.55 |
| Latissimus dorsi | 5 | 4.09 |
| Medial sural artery perforator | 3 | 2.45 |
| Thoracodorsal artery perforator | 3 | 2.45 |
| Parascapular | 3 | 2.45 |
| Toe pulp transfer | 2 | 1.63 |
| Total | 122 | 100 |
Table 3: Type of free flaps performed.
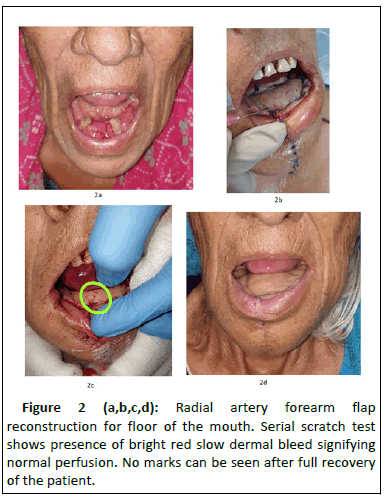
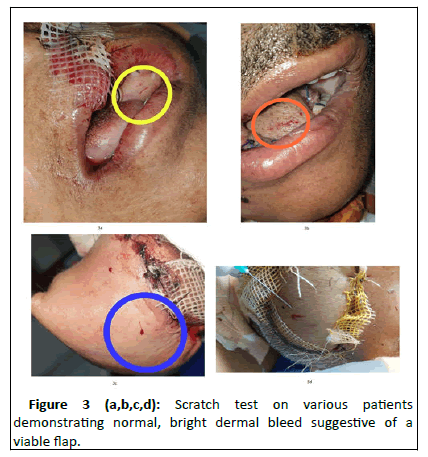
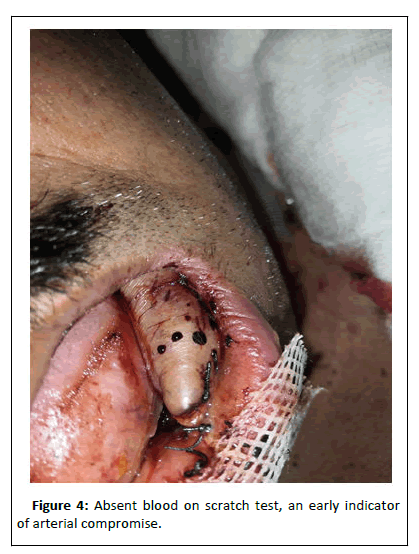
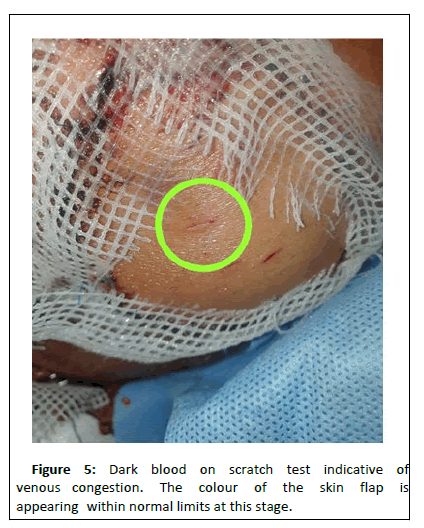
The early post operative monitoring of the free flap was done with clinical examination using the scratch test used as an adjunct. Scratch test was normal in 111 cases (91%) for initial 72 hours following the surgery (Figures 1-3). Eleven patients (9%) exhibited features of vascular compromise, detected and interpreted as per the defining criteria for the scratch test, while the clinical examination was either normal or equivocal at that instant. Eight patients out of these 11 (8/11) exhibited features of venous congestion with scratch test showing brisk flow (less than 3 seconds) of dark coloured blood (Figure 4). In this cohort, seven (7/8) had normal appearing clinical parameters (colour, temperature, turgor, capillary refill time). In one patient of this cohort (1/8), while the scratch test was suggestive of venous obstruction, the concurrent clinical examination was equivocal. Re-exploration was performed in all these 8 patients and venous compromise were found in all of them. Six patients (6/8) had a soft clot at the anastomosis line that necessitated evacuation of clot and redo anastomosis. One patient (1/8) had a well formed clot and it needed evacuation and re-anastomosis using a vein graft. In one patient (1/8), a hematoma was found compressing the anastomosis and hematoma evacuation promptly improved the venous return. Three patients out eleven in whom scratch test was deemed abnormal (3/11), had features of arterial blockage (Figure 5). In all of these three patients, scratch test showed no blood while the other clinical parameters were equivocal at that instant. Arterial blockage was confirmed on prompt re-exploration and revision of arterial anastomosis was performed. The abnormal scratch tests in these 11 patients were elicited within the initial 72 hours following the free flap surgery. Early identification helped in complete salvage of six (out of eleven compromised) flaps, while five flaps (4.09%) could not be salvaged (Table 4).
| Total flaps | 122 |
|---|---|
| Uneventful | 111 (91%) |
| Re exploration required | 11 (9%) (8-Venous compromise, 3-Arterial compromise) |
| Venous compromise (n=8) Flaps salvaged Flaps could not be salvaged |
4 4 |
| Arterial compromise (n=3) Flaps salvaged Flaps could not be salvaged |
2 1 |
| Overall flap survival | 117 (95.9%) |
| Overall flap loss | 5 (4.1%) |
Table 4: Final outcome of flaps.
We noted that invariably all the scratch marks over the flaps in the patients with successful outcome healed well without any infection or prominent scarring in the long run even if they appeared somewhat unsightly during the initial few days following the surgery.
Discussion
Free flap reconstruction has changed the face of post oncologic and post trauma reconstruction. It is a very versatile modality owing to its ability to provide ample amount of tissue for reconstruction. Post operative monitoring of free flaps is of utmost importance for timely and early identification of vascular compromise so that re-exploration can be done with an aim to salvage the compromised flap. The salvage rates in the literature are reported from 30% to more than 70% [9].
The traditional modality of flap monitoring is periodic, frequent clinical flap examination which takes into consideration flap colour, temperature, turgor and capillary refill time. This is still considered to be the gold standard for monitoring of free flaps [8]. Clinical monitoring is efficient and found to be predictive in 85-95% of cases [8,9]. While assessing the flap color, the color of the flap should be similar to the donor site. Pale colour is suggestive of arterial compromise while dark purplish colour is indicative of venous compromise. It is well recognized that flap color monitoring is very difficult in dark skinned people, thus hindering accurate judgment of flap viability [10]. Normal capillary refill time is 2-3 seconds. Brisk or delayed capillary refill times indicate venous and arterial compromise respectively. Temperature and turgor should be compared with that of adjoining non-flap tissue, but these can be difficult to assess in case of post operative edema of the adjoining areas. The surface temperature could be fallacious in cases patient is running fever. Thus, clinical examination of the flap has to be performed in a holistic fashion keeping in mind the various pitfalls that may vitiate the judgment.
Of the other available flap monitoring options, hand held acoustic doppler is a useful tool especially for the flaps where skin paddle is not available for monitoring [7]. This method was not assessed in this study. Similarly, duplex ultrasound is informative to find the arterial inflow and venous outflow. However, duplex ultrasound is operator dependent and additional cost of the equipment is associated with it [2,7].
Amongst the other used numerous methods, implantable doppler probes near the anastomoses and Indocyanine Green (ICG) near infrared angiography have shown fairly reliable and high rates of detecting early vascular compromise [11]. The implanatable dopplers (Cook-Schwartz device) are expensive and are not widely available especially in low and middle income countries. ICG near infrared angiography with pinprick test need the availability of the dye as well as ICG camera that may not be widely available especially in LMIC [12].
In many centers, pin prick test solely as an adjunct is also used for early flap monitoring [7]. However, there is always a risk of injuring an underlying perforator or an axial vessel especially if done by someone who was not a part of the operative team.
Scratch test is a simple, informative and useful adjunct to clinical examination. This test retains accuracy irrespective of skin color and allows early identification of flap failure in dark and fair skin colours alike, thus allowing early intervention. As evident by the results (ten out of eleven patients, it precedes other clinical signs in early identification of the vascular compromise. It enabled us to intervene early and six flaps out of eleven could be salvaged completely. Overall, the scratch test, as described, is simple to learn and perform, and, easy to interpret.
Conclusion
Physical examination still remains the gold standard for monitoring of free flaps. Scratch test is a simple and effective adjunct to clinical monitoring. It has the potential to alert the surgical team with first sign of vascular compromise and may precede the other clinical signs of flap monitoring.
References
- Cervenka B, Bewley AF (2015) Free flap monitoring: a review of the recent Literature. Curr Opin Otolaryngol Head Neck Surg 23:393-398
[Crossref] [Googlescholar] [Indexed]
- Chae MP, Rozen WM, Whitaker IS, Chubb D, Grinsell D, et al. (2015) Current evidence for postoperative monitoring of micro vascular free flaps: a systematic review. Ann Plast Surg 74:621-632
[Crossref] [Googlescholar] [Indexed]
- Spiegel JH, Polat JK (2007) Microvascular flap reconstruction by otolaryngologists: prevalence, postoperative care, and monitoring techniques. Laryngoscope 117:485-490
[Crossref] [Googlescholar] [Indexed]
- Perng CK (2013) Recent advances in postoperative free micro vascular flap monitoring. Formosan J Sur 46:145-148
- Siemionow M, Arslan E (2004) Ischemia/reperfusion injury: a review in relation to free tissue transfers. Microsurg 24:468-475
[Crossref] [Googlescholar] [Indexed]
- Yang JC, Kuo YR, Hsieh CH, Jeng SF (2007) The use of radial vessel stump in free radial forearm flap as flap monitor in head and neck reconstruction. Ann Plast Surg 59:378-381
[Crossref] [Googlescholar] [Indexed]
- Kohlert S, Quimby AE, Saman M, Ducic Y (2019) Postoperative Free-Flap Monitoring Techniques. Semin Plast Surg 33:13-16
[Crossref] [Googlescholar] [Indexed]
- Disa JJ, Cordeiro PG, Hidalgo DA (1999) Efficacy of conventional monitoring techniques in free tissue transfer: an 11 years experience in 750 consecutive cases. Plast Reconstr Surg 104:97-101
[Googlescholar] [Indexed]
- Hyodo I, Nakayama B, Kato H, Hasegawa Y, Ogawa T, et al. (2007) Analysis of salvage operation in head and neck microsurgical reconstruction. Laryngoscope 117:357–360
[Crossref] [Googlescholar] [Indexed]
- Chao AH, Lamp S (2014) Current approaches to free flap monitoring. Plast Surg Nurs 34:52-56
[Crossref] [Googlescholar] [Indexed]
- Han ZF, Guo LL, Liu LB, Li Q, Zhou J, et al. (2016) A comparison of the Cook-Swartz Doppler with conventional clinical methods for free flap monitoring: a systematic review and a meta-analysis. Int J Surg 32:109-115
[Crossref] [Googlescholar] [Indexed]
- Nagata T, Masumoto K, Uchiyama Y, Watanabe Y, Azuma R, et al. (2014) Improved technique for evaluating oral free flaps by pinprick testing assisted by indocyanine green near-infrared fluorescence angiography. J Craniomaxillofac Surg 42:1112-1116
[Crossref] [Googlescholar] [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences