Our Experience with Integra Dermal Regeneration Template (IDRT) and Glabrous Grafting for Plantar Raw Areas
Rupika Rajan*, NC Sreekuamar, Joseph Thomas and Mihika Antonia Dean
Published Date: 2024-01-03Rupika Rajan*, NC Sreekuamar, Joseph Thomas and Mihika Antonia Dean
Department of Plastic Surgery, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, India
- *Corresponding Author:
- Rupika Rajan
Department of Plastic Surgery,
Kasturba Medical College, Manipal Academy of Higher Education,
Manipal,
India
Tel: 919048861100
E-mail: rupikarajan@gmail.com
Received date: June 04, 2022, Manuscript No. IPARS-22-16909; Editor assigned date: June 06, 2022, PreQC No. IPARS-22-16909 (PQ); Reviewed date: June 20, 2022, QC No. IPARS-22-16909; Revised date: December 27, 2023, Manuscript No. IPARS-22-16909 (R); Published date: January 03, 2024, DOI: 10.36648/2472-1905.10.1.165
Citation: Rajan R, Sreekuamar NC, Dean MA, Thomas J (2024) Our Experience with Integra Dermal Regeneration Template (IDRT) and Glabrous Grafting for Plantar Raw Areas. J Aesthet Reconstr Surg Vol:10 No:1
Abstract
Background: One of the principles of plastic surgery is to replace “like with like”. In situations when flap cover is not feasible for reconstructing the soft tissue defects of the sole, an alternative is to apply IDRT to cover the vital structures (bone, tendon, fascia, nerves, vessels) and cover with glabrous skin graft to the areas of the weight-bearing region. The use of glabrous skin graft holds good with the principle of plastic surgery in replacing like with like. The glabrous graft will act and look like normal plantar skin. There is not much literature available on the use of IDRT with glabrous graft for the reconstruction of plantar raw areas
Materials and methods: The study included 7 patients with raw areas in the plantar aspect of the foot admitted under the Department of Plastic and Reconstructive Surgery at Kasturba Medical College, Manipal between 2021 and 2022. These patients underwent multiple rounds of debridements, IDRT application with NPWT dressing followed by glabrous grafting was done to weight-bearing areas of the foot.
Result: In our study, we used IDRT for exposure of bone, plantar fascia, thinned-out soft tissue, and deep soft tissue defect of the plantar area of the foot. 100% graft take noted in 6 patients and 90% in one patient. Donor sites healed within 2 weeks. Patients were pleased with color match at the recipient site and donor site scar. Patients were able to weight bear by 4 weeks at the recipient site.
Conclusion: The combination of the use of IDRT along glabrous graft can be used for resurfacing the plantar defects, as it covers vital structure and provides an additional layer to the foot the by use of IDRT and use of glabrous graft maintains the ontour of the foot without adding bulk to the foot unlike a flap, which makes ambulation and weight bearing easier and more stability. It also gives better a sensation than a non-neurotised flap. Hence this can be a recommended procedure to be considered for reconstruction of plantar skin defects.
Keywords
IDRT; NPWT; Glabrous graft; Plantar raw area; Reconstruction
Abbreviations
IDRT: Integra Dermal Regeneration Template; NPWT: Negative Wound Pressure Therapy; VSS: Vancouver Scar Scale; STSG: Split Thickness Skin Grafts
Introduction
Glabrous skin is found in the palms and soles. Here the epidermis is very thick with a thick layer of stratum corneum and a more compact but less elastic dermis. It is devoid of hair. In the sole glabrous skin is for weight bearing and is durable. Plantar raw areas are most commonly due to trauma, post-infection, post-excision of the tumor, or due to ischemic reasons.
One of the plastic surgery principles is to replace “like with like” to achieve the best possible result [1]. This concept has not been put to its full use in reconstructing soft tissue defects of the sole [2]. The flap cover is used whenever feasible for the reconstruction of plantar defects. The flap will be insensate and prone to recurrent breakdowns. Then the alternative is to apply IDRT to cover vital structures (bone, tendon, fascia, nerves, vessels) and cover with Split Thickness Skin Grafts (STSGs). The basic principle of donor site selection is to take skin from areas that will heal with minimal scarring while balancing the needs of the recipient site [3]. The use of non-glabrous skin graft has significant disadvantages when used for the reconstruction of plantar defects, these include painful hyperkeratotic buildup at the periphery of the skin graft, hypertrophic scarring and hyperpigmentation at the recipient site.
Using a glabrous graft for resurfacing the plantar raw areas goes in hand with the principle of plastic surgery. These grafts appear and act like normal plantar skin and will be more durable. The glabrous graft can withstand stress, pressure, and shearing forces. There is minimal donor site morbidity as the graft is harvested from the instep of the foot.
Integra dermal regeneration template is a bilaminar membrane system. The inner layer consists of a porous coprecipitate of bovine tendon type I collagen and shark glycosaminoglycan (chondroitin-6-sulfate), the outer layer by a temporary silicone epidermal substitute. The silicone layer prevents excessive moisture loss and formation of granulation tissue on the matrix surface [4]. The silicone layer acts as a physical barrier to bacterial contamination. Integra heals in phases similar to skin graft healing, progressing through (1) imbibition, (2) fibroblast migration, (3) neovascularization and (4) remodeling and maturation. During imbibition, the interstices of the matrix fill with wound fluid containing red blood cells and the fibrin in the wound exudate fosters adherence of the matrix to the wound bed. By day 7, myo fibroblasts start migrating into the matrix and start producing collagen by the beginning of week 3. The silicone epidermal layer has usually sloughed or been removed by this point in time. New blood vessels can be seen in the deep portion of the matrix by day 12 and reach the superficial surface by day 28, at which point a skin graft may be applied.
There is not much review of literature available for the application of IDRT with glabrous skin grafts for plantar raw areas.
Materials and Methods
The study included 7 patients with raw areas in the plantar aspect of the foot admitted under the Department of Plastic and Reconstructive Surgery at Kasturba Medical College, Manipal between 2021 and 2022. The raw area in the plantar aspect of the foot was following trauma and diabetic ulcer. All these patients underwent debridement followed by IDRT application with NPWT for 21 days and then underwent glabrous skin grafting. All patients had been followed up post-operatively at 2 weeks, 6 weeks, and 12 weeks. The age and gender of each patient and their wound etiology, area and size of skin defect for which glabrous graft was applied, donor site and outcomes were recorded and are listed in Table 1. Outcomes were analyzed to identify complications, skin graft take, the donor site satisfaction for glabrous graft and their Vancouver Scar Scale (VSS) scores for glabrous recipient site and donor site.
| Case no. | Age/gender | Cause of wound | Site of wound | Indication for IDRT | Glabrous graft area | Graft take % | Cause of graft failure | Donor site satisfaction for glabrous graft* | Post-op VSS score (Glabrous recipient/donor site) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 47/M | Degloving injury | Left foot plantar area | Exposure of plantar fascia | Left foot heel | 100 | 1 | 3/1 | |
| 2 | 25/M | Crush injury | Right foot plantar area | Thinned out soft tissue | Lateral border right foot | 90 | Hematoma | 2 | 4/2 |
| 3 | 36/M | Post-trauma | Right foot | Calcaneum exposure | Right heel | 100 | 1 | 3/1 | |
| 4 | 56/M | Diabetic ulcer | Right foot | Deep soft tissue defect | Right midfoot | 100 | 1 | 3/1 | |
| 5 | 23/M | Degloving injury | Right foot | Bone exposure | Right forefoot | 100 | 1 | 3/0 | |
| 6 | 42/M | Degloving injury | Right foot | Bone exposure | Right heel and along the border of first metatarsal area | 100 | 1 | 3/1 | |
| 7 | 33/M | Crush injury | Right foot | Plantar fascia exposure | Right midfoot | 100 | 1 | 3/1 |
Table 1: Summary of patient demographics, surgical method used and the outcomes assessed by post-operative Vancouver Scar Scale (VSS) score (*Donor site satisfaction excellent-1, good-2)
Patients with raw areas on the plantar aspect of the foot underwent multiple rounds of debridement to achieve favorable bed for IDRT application. With the application of IDRT a healthy bed of granulation tissue over bone, tendons or plantar fascia is achieved. Also the application of IDRT will provide an additional layer to the plantar aspect of the foot which will help in weight-bearing. Patients were put on NPWT dressing for 21 days. By this time silicone layer over the IDRT will start to separate off.
After 21 days the silicone layer over the IDRT is removed and the wounds in the weight-bearing part of the plantar aspect of the foot were covered with glabrous graft and the rest of the raw areas were covered with split-thickness skin graft from the thigh. The glabrous graft was harvested from the instep of the opposite foot using Humby’s knife and the graft was hand meshed with number 10 blade. Bactigras dressing was done for the recipient and donor site. Splint was applied for the recipient site. The graft was examined on post-op day 6 and a staple removed on post-op day 8 and then dressing was done on an alternate day. By post-op day 10 donor site dressing was opened and the covered with light dressing and ambulation was allowed on the donor site.
Patients were allowed ambulation with partial weight bearing on the recipient site by 2 weeks post–op. The outer cuticle layer of the graft was able to be removed by 2 weeks post-op. Patients were followed up post-op 2 weeks, 6 weeks and 12 weeks. By 4 weeks post-op patients can do full weight-bearing in the area of glabrous graft with off-loading shoes.
Results
Between 2021 to 2022, 7 patients were included in this study. The causes of wounds were traumatic wounds in 6 patients and diabetic ulcer in 1 patient. Indication for IDRT bone exposure (3 patients), plantar fascia exposure (2 patients), thinned out soft tissue (1 patient), deep soft tissue defect (1 patient). Area where glabrous graft was applied–heel (3 patients), midfoot (2 patients), forefoot (1 patient), lateral border (1 patient). All the patients were followed up for 3 months. No major complications occurred in these patients.
In all these patients the donor site was the opposite foot. The graft take noted was 100% in 6 patients and 90% in 1 patient. A good color match to the surrounding or opposite foot plantar area was noted. In all patients donor site healed within 2 weeks. All the patients were pleased with their glabrous donor site scar (excellent in 6 and good in 1).
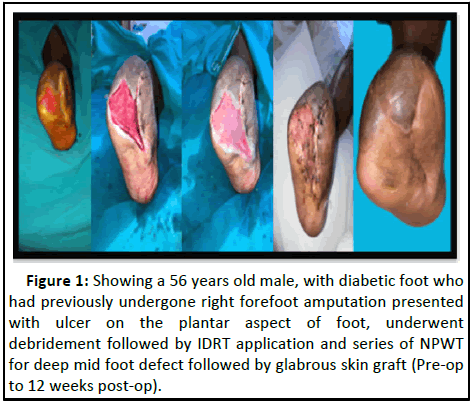
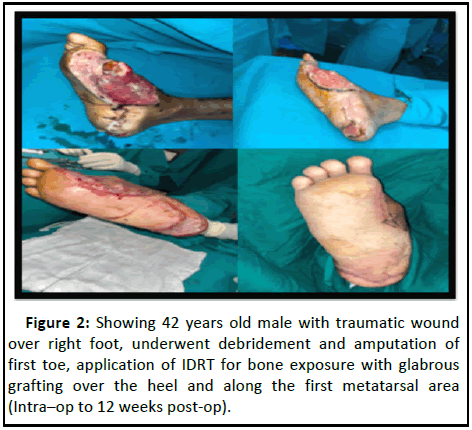
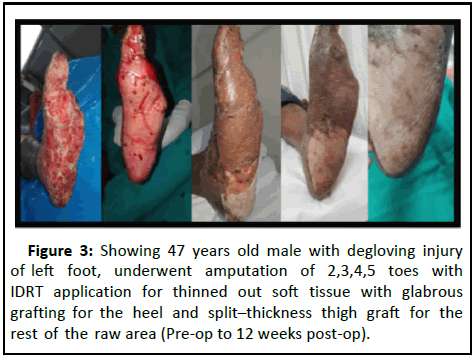
Scars at both the donor site and glabrous recipient sites were evaluated using VSS and results were noted to be excellent, the mean scores were 3.14 for recipient sites and 1 for donor sites respectively. Patients reported good weight bearing in the glabrous grafted area. The surgical course of the few patients is illustrated in Figures 1-3 and donor site of a patient is illustrated in Figure 4.
Figure 1: Showing a 56 years old male, with diabetic foot who had previously undergone right forefoot amputation presented with ulcer on the plantar aspect of foot, underwent debridement followed by IDRT application and series of NPWT for deep mid foot defect followed by glabrous skin graft (Pre-op to 12 weeks post-op).
Discussion
Le Worthy in 1963 was the first one to describe the technique of split-thickness plantar skin grafting [5]. The problems seen with nonglabrous split thickness skin grafting for plantar defects have largely been eliminated by the use of glabrous skin grafts. The glabrous skin grafts take well. A very good color match to the normal plantar skin is noted. The glabrous graft can with-stand pressure and shearing forces and hence durable. Application of IDRT over exposed bone, tendon or plantar fascia helps in covering these structures with an additional layer due to IDRT and making the wound bed viable for graft uptake [6]. The defects with significant depth in the plantar aspect when covered with IDRT along with NPWT dressing help to fill out to the level of the surrounding skin to an impressive degree. This is followed by glabrous grafting to the area of utmost weight-bearing in cases of a near total loss of plantar skin where the rest of the plantar raw area is grafted with split-thickness graft from the thigh, this helps the patient to ambulate with weight bearing in those areas of glabrous graft. The use of IDRT with glabrous graft recontours the plantar aspect of the foot to almost the normal plantar skin [7]. This in turn contributes greatly to the functionality of the foot in the form of early weight-bearing in the glabrous grafted area. There is no donor site morbidity as the donor site is instep of the foot, there is no hindrance for weight-bearing and the scar is hidden. The donor site is healed with stable, durable, pain-free and with minimal scar. These make the instep of the foot a favorable donor site both functionally and aesthetically. The disadvantage noted is limited donor site availability [8].
Conclusion
The combination of use of IDRT along with glabrous graft can be used for resurfacing the plantar defects, as it covers vital structure and provides an additional layer to the foot by use of IDRT and use of glabrous graft maintains the contour of the foot without adding bulk to the foot unlike a flap, which makes ambulation and weight bearing easier and more stability. It also gives better sensation than a non-neurotised flap. Hence this can be a recommended procedure to be considered for reconstruction of plantar skin defects.
References
- Banis JC (2001) Glabrous skin grafts for plantar defects. Foot Ankle Clin 6:827-837
[Crossref] [Google Scholar] [PubMed]
- Liu HH, Chang CK, Huang CH, Wu JR, Chen CY, et al. (2018) Use of split thickness plantar skin grafts in the management of leg and foot skin defects. Int Wound J 15:783-788
[Crossref] [Google Scholar] [PubMed]
- Le Worthy GW (1963) Sole skin as a donor site to replace palmar skin. Plast Reconstr Surg 32:30-38
[Google Scholar] [PubMed]
- Chang DK, Louis MR, Gimenez A, Reece EM (2019) The basics of integra dermal regeneration template and its expanding clinical applications. Semin Plast Surg 33:185-189
[Crossref] [Google Scholar] [PubMed]
- Heimbach DM, Warden GD, Luterman A, Jordan MH, Ozobia N, et al. (2003) Multicenter postapproval clinical trial of Integra® dermal regeneration template for burn treatment. J Burn Care Rehabil 24:42-48
[Crossref] [Google Scholar] [PubMed]
- Cheshire PA, Herson MR, Cleland H, Akbarzadeh S (2016) Artificial dermal templates: A comparative study of NovoSorb™ Biodegradable Temporising Matrix (BTM) and integra Dermal Regeneration Template (DRT). Burns 42:1088-1096
[Crossref] [Google Scholar] [PubMed]
- Schiavon M, Francescon M, Drigo D, Salloum G, Baraziol R, et al. (2016) The use of integra dermal regeneration template versus flaps for reconstruction of full-thickness scalp defects involving the calvaria: A cost benefit analysis. Aesthetic Plast Surg 40:901-907
- Wood FM, Stoner ML, Fowler BV, Fear MW (2007) The use of a non-cultured autologous cell suspension and Integra dermal regeneration template to repair full-thickness skin wounds in a porcine model: A one step process. Burns 33:693-700.
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences