Reconstruction of the Anterior Abdominal Wall by Parietoplasty in Three Cases
Mamadou Lassana Foba*, El Hadj Daour Teuw, Anne Aurore Sankale and Ndiaye Aï
Department of Plastic and Reconstructive Surgery, Aristide Le Dantec Hospital, Dakar, Senegal
Published Date: 2023-11-03DOI10.36648/2472-1905.9.4.162
Mamadou Lassana Foba*, El Hadj Daour Teuw, Anne Aurore Sankale and Ndiaye Aînina
Department of Plastic and Reconstructive Surgery, Aristide Le Dantec Hospital, Dakar, Senegal
- *Corresponding Author:
- Mamadou Lassana Foba
Department of Plastic and Reconstructive Surgery,
Aristide Le Dantec Hospital, Dakar,
Senegal,
E-mail: mamadlass1986@gmail.com
Received date: October 02, 2023, Manuscript No. IPARS-23-17967; Editor assigned date: October 05, 2023, PreQC No. IPARS-23-17967 (PQ); Reviewed date: October 19, 2023, QC No. IPARS-23-17967; Revised date: October 26, 2023, Manuscript No. IPARS-23-17967 (R); Published date: November 03, 2023, DOI: 10.36648/2472-1905.9.4.162
Citation: Foba ML, Teuw EHD, Sankale AA, Ndiaye Aï ( 2023) Reconstruction of the Anterior Abdominal Wall by Parietoplasty in Three Cases. J Aesthet Reconstr Surg Vol.9 No.4: 162.
Abstract
Repair of abdominal wall loss is relatively easy whenever the residual tissue loss is superficial and/or small. Conversely, large and transfixing resections involve more complex reconstructions. We conducted a 10 year retrospective study of anterior abdominal wall reconstruction in 3 patients. We conducted a 5 year retrospective study (2017-2022) of 3 patients with abdominal wall tumours that had undergone wide resection and parietoplasty reconstruction. The parameters studied were epidemiological, in particular age and sex, clinical aspects, in particular the circumstances of discovery, location, physical examination, morphological and anatomopathological assessment, type of excision and reconstruction and finally the postoperative follow-up three patients, predominantly female, with an average age of 52 years, were found to have sarcoma in two patients and carcinoma in one. They benefited from a large excision then reconstruction by flaps biomaterials in 2 patients plus flap alone in one patient. The postoperative course was marked by death in one patient due to his initial tumour and simple in the other two patients. The repair of the loss of substance is easy when the tumours are superficial but when the resections are transfixing, the association of a biomaterial for the reconstruction of the deep plane with a surface flap is necessary.
Keywords
Abdominal wall; Reconstruction; Parietoplasty
Introduction
Abdominal wall defects are defined as the loss of soft tissue in a wound in the abdomen. The abdominal wall is the soft tissue that is attached to the spine, the rib cage and the pelvic skeleton. The causes of these losses of substance are multiple and are represented by tumoral disease, infectious causes [1].
Tumour diseases includes parietal metastases, benign and primary malignant tumours (sarcomas, desmoid tumours, etc).These malignant tumours often require radical surgery with wide, full-thickness resection, known as transfixing. In these cases, they inevitably alter the function and aesthetics of the abdominal wall [2].
Repair of abdominal loss is relatively easy whenever the residual tissue loss is superficial and/or small. Conversely, large and transfixing resections involve more complex reconstructions depending on the location, size of the defect and site.
The strategy of this parietal reconstruction is conditioned by the level of its deep involvement.
The three keys to decision making are the existence of peritoneal involvement, the biological or synthetic nature of the deep parietal reconstruction and the choice for superficial coverage of the defect.
Our study, carried out retrospectively over five years from January 2017 to January 2022, is part of this framework and aims to provide an update on:
• The difficulty of reconstruction of large abdominal wall loss with the limitation of functional and aesthetic carcinological results.
• The multidisciplinary nature of the management of abdominal parietomy.
Case Series
Case 1
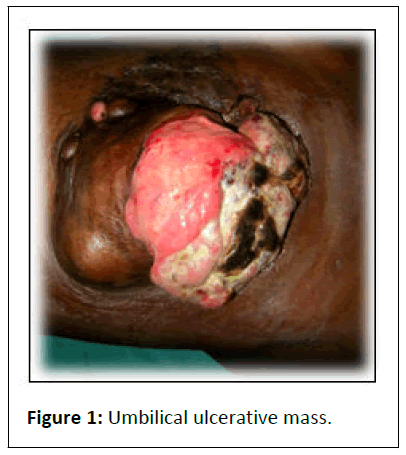
Mrs. S.S, aged 45 years, with no particular medical or surgical history, was admitted on 21/07/2017 for the management of an ulcerating tumor that had been evolving for 5 years in the umbilical region, measuring 20 cm by 12 cm (Figure 1), with no adenopathies found.
The biopsy performed was consistent with a sarcoma. The CT scan did not reveal any secondary location.
The therapeutic management on 21/09/2017 consisted of a large surgical removal followed by reconstruction of the anterior abdominal wall.
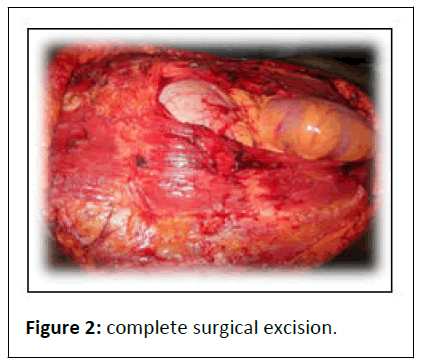
The patient was installed under general anaesthesia and in dorsal recumbency. The mono-bloc excision removed part of the rectus fascia and the peritoneum (Figure 2).
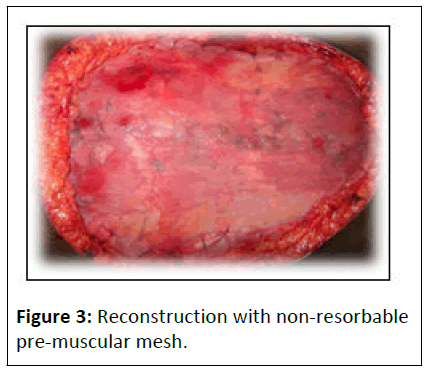
Reconstruction consisted of a peritoneal suture with polyglactin 910 (vicryl®) 2/0 by an over-jet and then the placement of a 15 cm by 20 cm non-resorbable pre-muscular mesh (Figure 3) fixed with non-resorbable 2/0 suture by separate stitches.
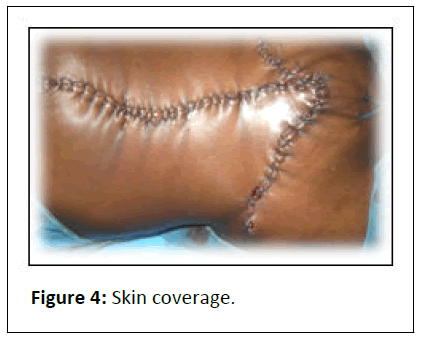
Finally, skin coverage was achieved with an inverted Trotation flap (Figure 4) using 3 advancement and transposition flaps fixed with 2/0 skin sutures in separate stitches.
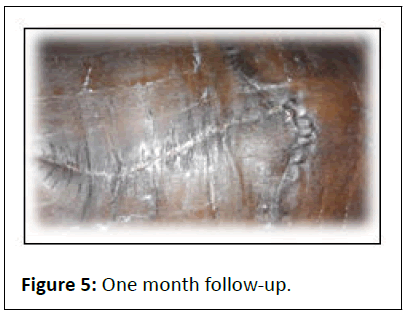
The postoperative course was simple with good healing at one month follow-up (Figure 5).
Case 2
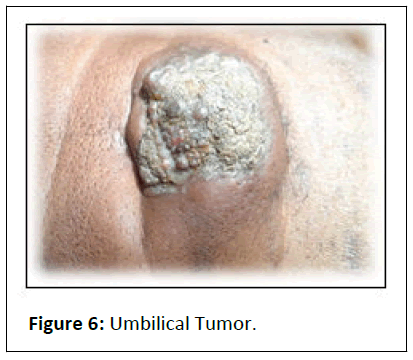
Mr. S.N, 61 years old with no particular medical or surgical history was admitted for the management of a pruritic and fistulised umbilical nodule measuring 5 cm by 8 cm that had been evolving for 2 years (Figure 6).
The abdominal CT-scan revealed a tissue mass in continuity with the rectus muscles. Biopsy was in favour of a carcinoma invading the abdominal wall.
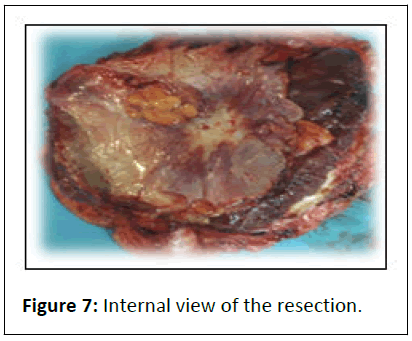
The patient has had surgery: Resection of the umbilical tumour, removing the rectus abdominis muscles and the parietal peritoneum (Figure 7).
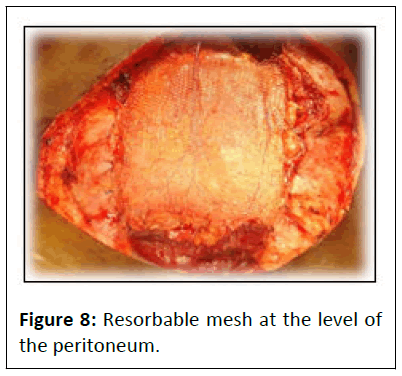
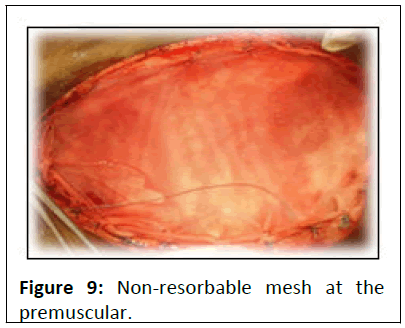
Reconstruction of the peritoneum was carried out using a 20 cm × 15 cm resorbable mesh (Figure 8) at the level of the peritoneum, followed by the placement of a non resorbable mesh in the premuscular (Figure 9).
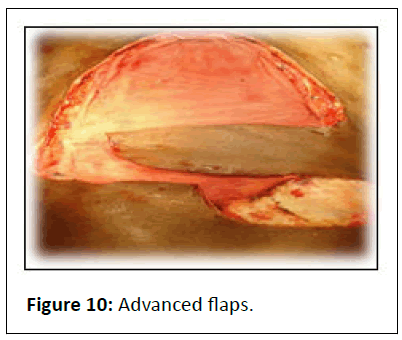
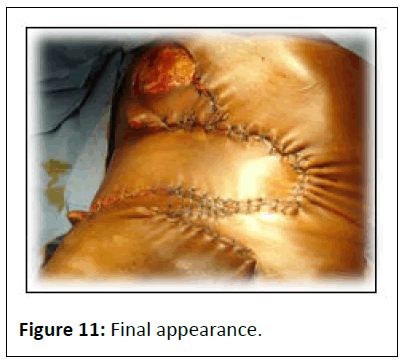
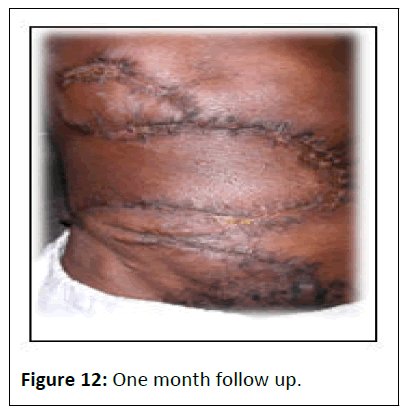
The skin was covered by five advancement and transposition laps (Figure 10) taken from the right and left flanks, the right and left inguinal regions with an upper zone left in directed healing (Figures 11 and 12).
Eight months later, a tumour of the head of the pancreas was discovered. The patient died three weeks later after attempted biliary drainage by Endoscopic Retrograde Cholangiopancreatography (ERCP).
Case 3
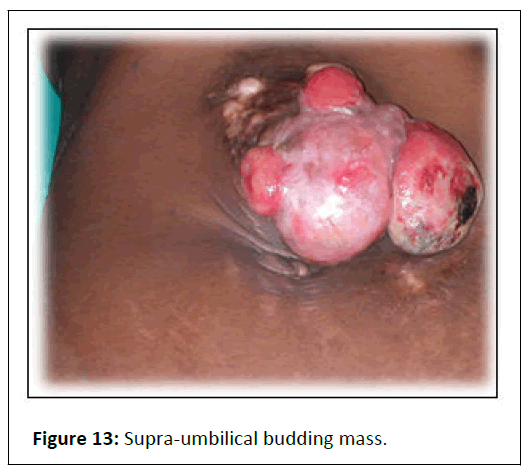
Mrs. AK, with no particular medical or surgical history, was admitted for the management of a skin tumour above the umbilical region.
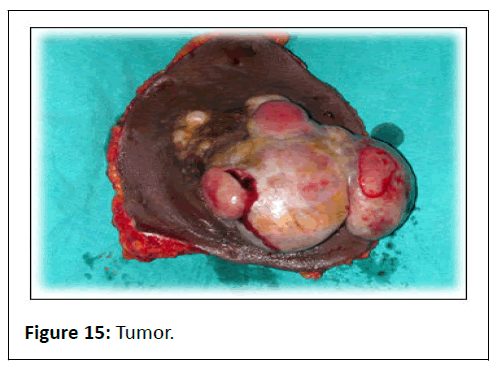
Examination revealed a bulging umbilical mass measuring 12 cm by 10 cm (Figure 13). The biopsy revealed a sarcoma.
The patient was placed in the supine position under general anaesthesia. An incision circumscribed the tumour with resection margins of 5 cm allowing conservation of the umbilicus.
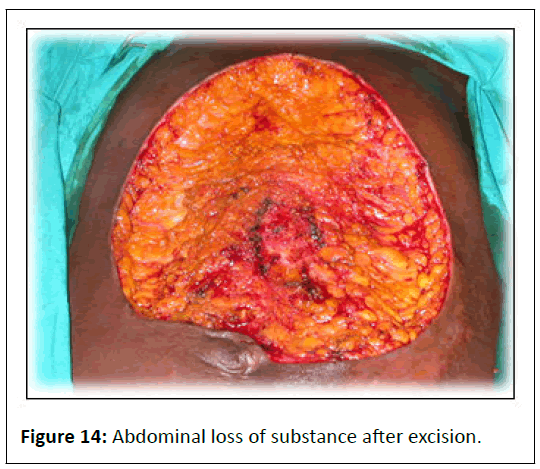
The exeresis was performed in one piece down to the premusculo fascia (Figures 14 and 15).
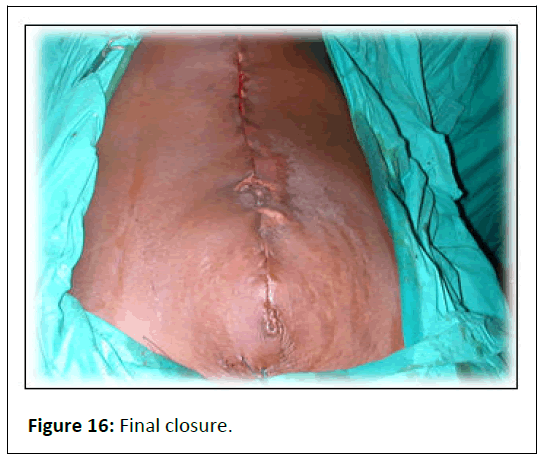
Reconstruction was performed with advancing skin flaps, then closure by suture with separate 2/0 skin sutures, thanks to the extension of the sub-umbilical incision (Figure 16).
The postoperative course was simple. Anatomical pathological examination was in favour of a sarcoma. The follow-up was 6 months.
Results and Discussion
The average age of our patients was 36.7 years. Couturaud in France found an average age of 41.3 years [2].
In our series, the distribution of patients according to sex shows a female predominance. This female predominance is found in the literature for desmoid tumours [3].
In the MIR-study in France, sarcomas have a prevalence of about 1% of adult cancers and cover a very large group of tumours occurring at all ages (median age=50 years) and affecting a population with a balanced sex ratio [4]. The aetiology of abdominal wall discharges is tumour or infectious pathology.
The aetiology of the losses of substance found in our study was 2 cases of sarcoma and 1 case of Sister Marie Joseph nodule.
Primary malignant tumours of the abdominal wall are rare and represent an inhomogeneous group [5,6]. The most common histological type is sarcoma.
Sarcomas are rare malignant tumours of mesenchymal origin, arising from connective and supporting tissues [4].
The diagnosis is usually that of an asymptomatic, often large tumour and is based on surgical biopsy. Two of our patients underwent surgical biopsy to make the preoperative diagnosis. Their histological diagnosis is difficult, requiring immunohistochemistry among other things [7]. This was not the case in our patients.
One case of Sister Mary Joseph nodule was diagnosed as a metastasis of a primary digestive tumour. The mechanism of occurrence of this secondary dissemination is discussed [2] and two hypotheses are possible:
• The first is that of metastatic spread by the haematogenous route.
• The second is that of exfoliation of cancerous cells.
Desmoid tumours [2] are fibromatoses that most often affect women. A distinction is made between extra-abdominal desmoid tumours and intra-abdominal desmoid tumours. They are locally malignant and do not metastasise, but they tend to recur. We did not find any desmoid tumours in our study.
Radiological imaging plays an important role in the preoperative and extension work-up. Our patients underwent excisional surgery. Surgery for abdominal wall tumours most often consists of monobloc excision followed by repair of the loss of substance and reconstruction of the anterior abdominal wall.
The removal of these tumours is based on certain principles, in particular the resection margins. In the case of epithelial tumours, the resection margins are of the order of a centimeter and the loss of substance caused by such tumours is only problematic when they are very large [8,9]. It is in the case of malignant connective tissue tumours or sarcomas that the margins must be extended. This was found in two of our patients where the wide resection involved part of the rectus muscle and the peritoneum.
The reconstruction of the anterior abdominal wall is done from the depth to the surface. In the case of isolated peritoneal involvement, the loss of substance poses little problem of repair [10]. If the size is small, the detachment of the peritoneal margins allows direct suturing in most cases. If the deperitonisation is extensive, a pedicled omentum may be performed if there is sufficient omentum. Two of our patients had a simple suture and placement of an absorbable prosthesis.
For prosthesis coverage, several implantation sites can be used: The intra-peritoneal site, the retro-muscular site and the pre-musculoaponeurotic site.
Implantation of prosthesis at the intra-peritoneal site is indicated in the case of major parietal decay or laparostomy and has the disadvantage of a risk of adhesion due to contact of the material with the viscera. The prosthesis will therefore normally be made of PTFE. PTFE is not available in our surgical practice, so we did not use this prosthesis.
The advantage of placing the prosthesis retro-muscularly is that the prosthesis will directly reinforce the wall at the level of the deficient musculoaponeurotic plane, while protecting the viscera from direct contact with the material. The disadvantage is that it is only possible in practice if the defect is moderate.
The advantage of the pre-musculoaponeurotic site is that it is very easy and the disadvantage is that the prosthesis is directly under the skin of the abdomen.
The use of non-absorbable synthetic prostheses limits the risk of hernia due to a solid material without tension on the sutures, but at the cost of an increased risk of infection.
Conclusion
Repair of abdominal wall loss is relatively easy whenever the residual tissue loss is superficial and/or small. Conversely, large and transfixing resections involve more complex reconstructions.
References
- Pailler Jl, Annelakhel B (1999) Incisional hernia of the abdominal wall. Pathophysiology, etiology and prosthetic repair techniques. Ann Chir Plast Esthét. 44: 313-324.
[Google Scholar], [Indexed]
- Couturaud B, Arnaud E, Revol, Servant JM (1999) Malignant tumors of the abdominal wall. 10 years of experience at the Saint-Louis hospital. Ann Chir Plast Est 44: 373-383.
[Google Scholar], [Indexed]
- Mignot L (2002) Les tumeurs desmoïdes. Orphanet encyclopédie.
- Champeau F, Verola O, Vignon P (1998) Cutaneous and subcutaneous sarcomas. Ann Chir Plast Est 43: 421-438.
- Clément A, Hoeffet C, legmenn P, Bonnin A (1995) Computed tomography imaging of abdominal wall metastases after laparoscopy. J Radiol 84: 56-54.
[Google Scholar], [Indexed]
- Gautier MS (2011) Tumeurs cutanées avec les lésions précancéreuses le manuel du généraliste (2 Edition), Dermatologie. Strasbourg 610.
- Gore Rm, Levin MS, Laufer I (1994) Text book of gastrointestinal radiology. Anterior abdominal wall in Marn CS.
- Addolf M, Arnaud JP (1976) Experimental study of resistance to and biologic tolerance of prosthetic materials used in the repair of losses of substance of the abdominal wall. Chirurgie 102: 390-396.
[Google Scholar], [Indexed]
- Boutier R, Papillard M, Rouvier O (2013) Location of perforating arteries before surgery for ALT, TAP, DIEP perforating flaps. Elsevier Masson 7-26.
- Zrig A, Zaara B, Salem R, Saad J, El-Mhabrech H, et al. (1987) Anterior abdominal wall normal and pathological aspects. Eur J Ped 146: 387-389.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences