Reduction Mammaplasty in Patients with Significant Asymmetry- An Assessment of Clinical and Patient Reported Outcomes
1Division of Plastic Surgery, Department of Surgery, University of Pennsylvania, Philadelphia, PA, USA
2Department of Surgery, Thomas Jefferson University, Philadelphia, PA, USA
- *Corresponding Author:
- Dr. John P. Fischer
Division of Plastic Surgery
Department of Surgery
University of Pennsylvania
Philadelphia, PA, USA.
Tel: 00989121909095
E-mail: John.Fischer2@pennmedicine.upenn.edu
Received Date: August 17, 2021; Accepted Date: September 13, 2021; Published Date: September 20, 2021
Citation: Rios-Diaz AJ, Cunning JR, Shakir S, Broach R, Elfanagely O, et al. (2021) Reduction Mammaplasty in Patients with Significant Asymmetry- An Assessment of Clinical and Patient Reported Outcomes. J Aesthet Reconstr Surg Vol.7 No.6:41.
Abstract
Background: The improvement in Patient-Reported Outcomes (PROs) gained by patients undergoing Reduction Mammoplasty (RM) for macromastia with marked asymmetry has not been characterized. We assessed clinical and PROs in women with marked preoperative breast asymmetry.
Methods: Patients with macromastia undergoing RM at an academic hospital were retrospectively identified (2016-2020). Those who completed pre- and postoperative BREAST-Q© questionnaires were included. Marked breast asymmetry was defined by the ratio of breast tissue excised between breasts > 75th percentile. Risk-adjusted logistic regression and generalized linear models were used to compare clinical outcomes and determine predicted mean differences in PRO BREAST-Q© scores, respectively.
Results: 105 patients were included: 75.2% symmetric, 24.8% asymmetric. Median age was 39 years and BMI 29.8 kg/m2, 50.5% were Black, 74% had brassier cupsize ≥ DDD, undergoing a wise-pattern inferior pedicle RM (60%). The asymmetric group had a 27.4% (IQR 20.5–39.5%) The median difference of between breast tissues excised was higher for the asymmetric group (27.4% vs. 6.5%; p < 0.01). The overall complications and revisions did not differ (p > 0.05). Marked asymmetry was associated with lower baseline BREAST-Q© scores in the psychosocial, sexual, and physical well-being scales. Overall, PROs improved significantly for all RM patients (p < 0.05), with no significant differences in the relative improvement between cohorts (p > 0.05).
Conclusion: The macromastia burden is higher for patients with marked breast asymmetry. However, surgeons should be encouraged to achieve symmetric results irrespective of preoperative imbalances as clinical outcomes and the magnitude of PROs improvement are comparable despite differences in tissue excised among patients with macromastia.
Keywords
Patient-reported outcomes; Breast reduction; Mammoplasty; Satisfaction; Quality of life; Surveys; Questionnaire; Patient-centered; Asymmetry
Introduction
While human bodies are theoretically symmetric bilaterally, paired structures, such as breasts, ears, and fingers, often show small degrees of asymmetry when dimensions are directly compared [1]. As sexually selected traits, breasts are especially prone to fluctuating asymmetry. While estrogen appears to be a factor influencing asymmetry in breasts, it is more well-known for its role in breast growth. Cases of excessive breast growth can result in symptomatic macromastia, a common condition known to incapacitate women [2]. Symptomatic macromastia results in adverse Patient-Reported Outcomes (PROs) such as functional disability and physical and psychologic distress that leads to decreased in satisfaction and health-related Quality Of Life (QOL) [3-5]. Consequentially, many women with symptomatic macromastia seek Reduction Mammoplasty (RM) to provide symptomatic relief and improve their QOL [6].
Prior studies have demonstrated that women presenting for RM have lower than average PROs and that surgery results in a significant, quantifiable improvement [7,8]. Moreover, existing literature suggests that Increased Body Mass Index (BMI), breast cup size, and/or amount of tissue resected do not correlate with the degree of improvement in postoperative PROs [9,10]. However, available literature on the association breast asymmetry with PROs is limited to data derived from international cohorts and unadjusted comparisons of postoperative PROs, which fail to account for baseline preoperative differences between groups [11]. The cutoffs for the degree of asymmetry used were based on a classification derived from a an international study by Persichetti P, et al. [12], and therefore, is it unknown whether these are generalizable to a racially-diverse population in the United States (U.S.). Moreover, the burden of disease among patients with symptomatic macromastia and significant asymmetry and their clinical outcomes following RM have yet to be elucidated.
We have utilized the previously validated BREAST-Q© QOL instrument to collect matched preoperative and postoperative patient-specific data related to the impact of breast asymmetry on symptomatic clinical improvement and PROs over time [13,14]. In this study, we aimed to
(1) Determine whether there are differences in PROs as defined by the BREAST-Q© survey among patients with substantial breast asymmetry who plan to undergo RM relative to the general population.
(2) Assess the magnitude of PROs improvement by the degree of asymmetry.
(3) Compare clinical outcomes. We hypothesized that women with marked breast asymmetry undergoing RM for the treatment of symptomatic macromastia have lower preoperative PROs yet experience similar clinical outcomes and degree of improvement based on the BREAST-Q instrument as women without marked breast asymmetry.
Methods
Design and study population
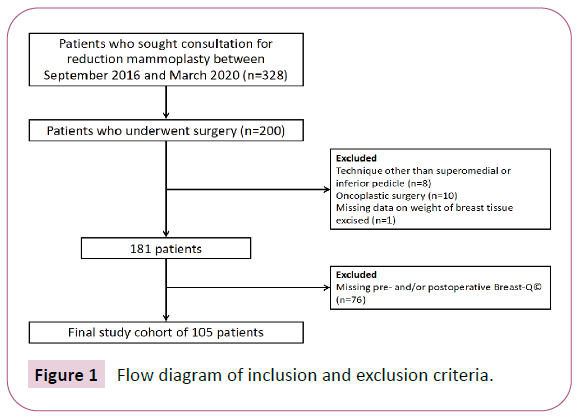
We performed a retrospective cohort study approved by the University of Pennsylvania Institutional Review Board. Inclusion criteria was comprised of adult women ( ≥ 18 years old) seeking consultation for RM by two plastic surgeons who administer PROs as standard of care (JPF and PB) in a large academic center between September 2016 and March 2020. Exclusion criteria included RM techniques that did not utilize a wise pattern inferior or superomedial pedicle, oncoplastic cases, and missing data on weight of breast tissue excised. We additionally excluded those with incomplete QOL data. Patients were subsequently stratified into two cohorts (symmetric vs. asymmetric) according to the ratio of right-to-left breast tissue excised (grams) greater than the 75th percentile. This definition was chosen given that the goal of RM should be the achievement of QOL improvement with good breast symmetry, shape and volume [11] and that surgeons correct preoperative imbalances through excision of different amount tissue mass per breast.
Data source and covariates
Demographic, clinical, and operative variables were extracted through review of the Electronic Medical Record (EMR). Variables extracted included age, race (African-American, Caucasian, Other), ethnicity (Non-Latino or Non-Hispanic, Latino or Hispanic, Unknown), private insurance, self-pay status, income quartile by zip code, BMI, smoking status (non-smoker, active, former), diabetes mellitus, Hypertension (HTN), Chronic Obstructive Pulmonary Disease (COPD), Peripheral Vascular Disease (PVD), immunosuppression, history of weight loss surgery, regnault ptosis grade [15], breast asymmetry (per surgeon’s discretion), brassier notching, presence of intertriginous breast rash, brassier cup size, average nipple to Inframammary Fold (IMF) distance, long nipple to IMF distance ( > 75th percentile for either breast), average nipple to sternal notch distance, long nipple to sternal notch distance ( > 75th percentile for either breast), pedicle technique (inferior, superomedial), skin excision pattern (wise, vertical), use of skin glue, and use of surgical drains.
BREAST-Q© questionnaire and QOL data collection
The BREAST-Q© Breast Reduction module is a validated PRO survey that quantifies QOL and satisfaction for patients undergoing breast surgery in various scales: Satisfaction with breasts, psychosocial well-being, sexual well-being and physical well-being for both preoperative and postoperative versions, satisfaction with outcome and satisfaction with information for the postoperative version. The first four scales are shared between the preoperative and postoperative versions. In addition, the BREAST-Q© Breast Reduction Module includes a seventh scale that quantifies satisfaction with nipple-areola [6]. BREAST-Q© surveys are routinely administered in our outpatient practice as the standard of care while patients wait to see the surgeon in clinic during preoperative and postoperative followup encounters (typically between at 1-3 months). These data are entered by our medical assistant using a built-in Epic (Epic Systems Corporation, Verona, WI) SmartPhrase and are readily available in the EMR before the patient encounter is started. Surgeons use this information to assess baseline and progress of QOL before and after surgery. BREAST-Q© scores are retrospectively abstracted from the EMR using a prospectively maintained REDCap database (REDCap, Vanderbilt University, Tennessee). Scores are calculated a posteriori for research and quality improvement purposes using the BREAST-Q© proprietary software.
Outcomes
The primary outcomes were QOL and satisfaction as measured by each of the BREAST-Q© domains. These outcomes data were collected during preoperative (baseline) and postoperative encounters. Secondary outcomes included postoperative complications such as cellulitis, Surgical Site Infection (SSI), seroma, hematoma, delayed healing, wound dehiscence, nipple areolar complex (NAC) necrosis, fat necrosis, readmissions and Emergency Department (ED) visits related to the index procedure, reoperations (due to a complication or adverse non-aesthetic outcome) and a composite of the aforementioned. Revisions, which were defined as reoperations for aesthetic reasons, were also collected.
Statistical Analysis
Descriptive statistics were used to report counts and frequencies for categorical data, and medians and Interquartile Range (IQR) for non-normally distributed continuous data. Pearson’s Chi-square and Kruskal-Wallis tests were used to compare categorical and continuous data, respectively. Paired Wilcoxon signed-rank test were used to compare improvement of BREAST-Q© for each group. The improvement in QOL difference between postoperative and preoperative BREAST-Q© scores were compared between groups. Unadjusted and adjusted generalized linear models with log link followed by postestimation calculations of average marginal effects were used to obtain predicted mean differences in BREAST-Q© scores with 95% CI between groups. These models were adjusted for age and pedicle technique which differed significantly between groups in univariate analysis, in addition to BMI and brassier cup size which have been identified as a potential confounder by prior literature. Modified Park tests [13] were used to account for the non-normal distributions of BREAST-Q© scores and determined the appropriate family distribution for each model. BREAST-Q©’s scales are independent from each other [6], so complete data were analyzed for each domain. A risk-adjusted logistic regression model with robust standard errors was used to determine the association of marked preoperative asymmetry with postoperative complications. In order to assess whether our patients had lower QOL than the population, we compared the BREAST-Q© scores to normative values for preoperative scales provided by Mundy LR, et al. [8] using Z tests. Univariate comparisons of all the characteristics and clinical outcomes assessed between respondent and non-respondents were performed to assess non-respondent bias. Lastly, a sub analysis comparing the degree of correlation between surgeon defined asymmetry and our definition by weight of tissue excised was ascertained by the Pearson's correlation coefficient. The sample size was defined by the available data since the surgeons routinely incorporated capture of PROs in their practices and we were at least powered to detect 20-30% difference in BREAST-Q© scale (power 0.8; alpha=0.05) using as reference data provided by Mundy LR, et al. [8]. Statistical significance was set at p < 0.05 and all analyses were performed using STATA/IC 16.0 (StataCorp LLC; College Station, TX).
Results
A total of 191 women were considered for eligibility. Of these, 105 patients met the inclusion criteria (55% response rate): 79 (75.2%) in the symmetric cohort and 26 (24.8%) in the asymmetric cohort (Figure 1). Median weight removed per breast was 781 grams (IQR 581-1048) across cohorts and the median difference of breast tissue removed from one side relative to the other was 6.5% (IQR 3.5%-10.9%) and 27.4% (IQR 20.5%-39.5%) in the symmetric and asymmetric cohorts, respectively (p < 0.01). Overall, the median age was 39 years (IQR 27-51) and the majority of patients were African-American (50.5%), non-Hispanic (94.3%), insurance payers (88.6%), with median BMI 29.8 kg/m2 (IQR 26.8- 33), a brassier cup size DDD or greater (73.8%), and underwent RM based on an inferior pedicle (60%).
Table 1 includes a comparison of demographic, clinical and operative characteristics. Patients in the asymmetric cohort were older (median 47.2 years [IQR: 38.4 - 55.6] vs. 36.2 years [IQR: 26.7 - 45.6]; p < 0.01) and diabetic (15.4% vs. 1.3%; p < 0.01), but did not differ by BMI (median 30.6 kg/m2 [IQR: 27.9 - 34.4] vs. 29.6 kg/m2 [26.2 – 33]; p=0.2). Patients with marked asymmetry were also more likely to undergo RM based on a wise pattern inferior pedicle with drain placement, and less likely to have skin glue utilized during cuticular closure.
| Characteristic | Patients with Breast Symmetry (n=79) | Patients with Marked Breast Asymmetry (n=26) | p | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Race | -- | -- | -- | -- | 0.67 |
| Black | 40 | 50.60% | 13 | 50.00% | -- |
| White | 34 | 43.00% | 10 | 38.50% | -- |
| Other | 5 | 6.30% | 3 | 11.50% | -- |
| Ethnicity | -- | -- | -- | -- | 0.15 |
| Non-Latino or Non-Hispanic | 76 | 96.20% | 23 | 88.50% | -- |
| Latino or Hispanic | 2 | 2.50% | 3 | 0.115 | -- |
| Not Disclosed | 1 | 0.013 | 0 | 0% | -- |
| Private Insurance | 75 | 94.90% | 24 | 92.30% | 0.62 |
| Self-Pay | 7 | 8.90% | 0 | 0% | 0.12 |
| Income Quartile | -- | -- | -- | - | 0.6 |
| 0-25th | 22 | 27.80% | 4 | 15.40% | -- |
| 26-50th | 15 | 19.00% | 7 | 26.90% | -- |
| 51-75th | 20 | 25.30% | 7 | 26.90% | -- |
| 76-100 | 22 | 27.80% | 8 | 30.80% | -- |
| Smoking Status | -- | -- | -- | -- | 0.47 |
| Never | 67 | 84.80% | 20 | 76.90% | -- |
| Current | 4 | 5.10% | 1 | 3.80% | -- |
| Former (Quit for > 30 days) | 8 | 10.10% | 5 | 19.20% | -- |
| Diabetes | 1 | 1.30% | 4 | 15.40% | < 0.01 |
| Immunosuppression | 1 | 1.30% | 1 | 3.80% | 0.4 |
| Peripheral Vascular Disease | 2 | 2.50% | 1 | 3.80% | 0.73 |
| Significant Weight Loss | 6 | 7.60% | 0 | 0% | 0.15 |
| Ptosis Grade | -- | -- | -- | -- | 0.17 |
| Grade 0 | -- | -- | 1 | 0.038 | -- |
| Grade 2 | 25 | 31.60% | 6 | 23.10% | -- |
| Grade 3 | 54 | 68.40% | 19 | 73.10% | -- |
| Bra Notching | 75 | 94.90% | 21 | 80.80% | 0.03 |
| Rash | 54 | 68.40% | 19 | 73.10% | 0.65 |
| Cup Size | -- | -- | -- | -- | 0.68 |
| C, D, DD | 22 | 28.60% | 5 | 19.20% | -- |
| DDD | 26 | 33.80% | 8 | 30.80% | -- |
| DDDD | 10 | 13.00% | 5 | 19.20% | -- |
| > DDDD | 19 | 24.70% | 8 | 30.80% | -- |
| Preoperative Nipple to Notch Distance > 75th percentile* | 8 | 10.50% | 6 | 25.00% | 0.08 |
| Preoperative Nipple to IMF Distance > 75th percentile* | 8 | 10.50% | 3 | 12.50% | 0.79 |
| Pedicle Technique | -- | -- | -- | -- | 0.01 |
| Inferior Pedicle | 42 | 53.20% | 21 | 80.80% | -- |
| Super medial Pedicle | 37 | 46.80% | 5 | 19.20% | -- |
| Skin Excision Pattern | -- | -- | -- | -- | 0.09 |
| Wise pattern/Inverted-T | 71 | 89.90% | 26 | 100.00% | -- |
| Vertical | 8 | 10.10% | 0 | 0.00% | -- |
| Use of Skin Glue | 57 | 72.20% | 12 | 48.00% | 0.03 |
| Use of Surgical Drains | 49 | 62.00% | 23 | 88.50% | 0.01 |
| Median | IQR | Median | IQR | p | |
| Age (years) | 36.2 | (26.7 - 45.6) | 47.2 | (38.4 - 55.6) | 0.01 |
| BMI (kg/m2) | 29.6 | (26.2 - 33) | 30.6 | (27.9 - 34.4) | 0.2 |
| Preoperative Nipple to Notch Distance (cm)* | 32.2 | (30 - 35) | 33.4 | (30.1 - 37) | 0.63 |
| Preoperative Nipple to IMF Distance (cm)* | 13.8 | (12.2 - 15.2) | 14 | (13 - 14.5) | 0.67 |
| Average Weight of Tissue Removed (g) | 755.5 | (543.5 - 1013.5) | 947.2 | (660 - 1200) | 0.07 |
Table 1 Demographic, clinical and operative characteristics in a population of women who underwent reduction mammoplasty grouped by degree of asymmetry.
Table 2 reports postoperative outcomes. The overall complication rate was 24.8% and comparable between cohorts (p=0.78). Individual complications did not significantly differ between cohorts (p > 0.05). The total revision rate was 6.7% and did not differ between cohorts (p=0.81). Within a risk-adjusted logistic regression model, there was no association between marked preoperative asymmetry and postoperative complications (Odds Ratio 0.82 [95% Confidence Interval: 0.25 - 2.7]; p < 0.74).
| Outcomes | Patients with Breast Symmetry (n=79) | Patients with Marked Breast Asymmetry (n=26) | p | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Complication Composite* | 19 | 24.10% | 7 | 26.90% | 0.77 |
| Surgical Site Infection | 3 | 3.80% | 0 | 0.00% | 0.31 |
| Cellulitis | 1 | 1.30% | 0 | 0.00% | 0.56 |
| Hematoma | 1 | 1.30% | 1 | 3.80% | 0.4 |
| Delayed Healing at T-Point | 7 | 8.90% | 1 | 3.80% | 0.4 |
| Wound Dehiscence | 2 | 2.50% | 1 | 3.80% | 0.73 |
| NAC Necrosis | 4 | 5.10% | 0 | 0.00% | 0.24 |
| Fat Necrosis | 4 | 5.10% | 2 | 7.70% | 0.62 |
| ED Visit | 4 | 5.10% | 0 | 0.00% | 0.24 |
| Readmission | 1 | 1.30% | 0 | 0.00% | 0.56 |
| Reoperation | 5 | 6.30% | 3 | 11.50% | 0.39 |
| Revision | 5 | 6.30% | 2 | 7.70% | 0.81 |
Table 2 Postoperative outcomes grouped by degree of asymmetry.
QOL and satisfaction
Table 3 reports BREAST-Q© scores for preoperative and postoperative domains as well as the net improvement in the four scales shared between cohorts. The median time to postoperative BREAST-Q© was 80 days (IQR 45-94), which was not significantly different between cohorts (p < 0.17). In univariate analyses, baseline BREAST-Q© scores were lower in the psychosocial well-being for patients in the asymmetric cohort preoperatively (median 28 [21-41] vs. 38 [28–49]; p=0.03) but were comparable for the other preoperative scales assessed (p > 0.05). Both postoperative scores and relative improvement (postoperative score – preoperative score) for the four scales were comparable between cohorts (p > 0.05). However, paired comparisons of preoperative versus postoperative scores for the four scales assessed demonstrated significant improvement in both cohorts (p < 0.01). Controlling for age, BMI, and surgical technique, patients with marked preoperative asymmetry had lower preoperative scores in the psychosocial well-being, sexual well-being and physical well-being BREAST-Q© scales (Table 4). There were no differences in postoperative scores or the relative improvement. Non-respondent analysis showed no significant differences.
| Breast-Q© domain | Patients with Breast Symmetry (n=79) | Patients with Marked Breast Asymmetry (n=26) | P | |||
|---|---|---|---|---|---|---|
| p50 | IQR | p50 | IQR | |||
| Preoperative Scores n | Satisfaction with breast | 23 | (18 - 31) | 18 | (0-26) | 0.19 |
| Psychosocial well-being | 38 | (28 - 49) | 28 | (21-41) | 0.03 | |
| Sexual well-being | 38 | (29 - 46) | 36.5 | (7.5-40) | 0.4 | |
| Physical well being | 45 | (33 - 53) | 36 | (23-50) | 0.09 | |
| Postoperative Scores | Satisfaction with breast | 90 | (72 - 100) | 90 | (79-100) | 0.69 |
| Psychosocial well-being | 100 | (68 - 100) | 87 | (71-100) | 0.87 | |
| Sexual well-being | 100 | (67 - 100) | 84 | (61-100) | 0.35 | |
| Physical well being | 83 | (71 - 92) | 71 | (63 - 92) | 0.26 | |
| Satisfaction with outcome | 100 | (100 - 100) | 100 | (100-100) | 0.26 | |
| Satisfaction with information | 100 | (83 - 100) | 100 | (83-100) | 0.95 | |
| Satisfaction with nipples | 100 | (87 - 100) | 100 | (100 - 100) | 0.36 | |
| Satisfaction with plastic surgeon | 100 | (100 - 100) | 100 | (100 - 100) | 0.34 | |
| Satisfaction with medical team | 100 | (100 - 100) | 100 | (100 - 100) | 0.26 | |
| Satisfaction with office staff | 100 | (100 - 100) | 100 | (100 - 100) | 0.68 | |
| Score Improvement (Postoperative - Preoperative) | Satisfaction with breast | 64 | (49 - 77) | 63 | (48-82) | 0.66 |
| Psychosocial well-being | 49 | (29 - 63) | 46 | (32-74) | 0.55 | |
| Sexual well-being | 42.5 | (22.5 - 67.5) | 48.5 | (25 -61.5) | 0.88 | |
| Physical well being | 36 | (27 - 50) | 46 | (29 - 58) | 0.46 | |
Table 3 BREAST-Q© scores per scale comparing patients undergoing RM by presence of marked asymmetry.
| Unadjusted | Adjusted | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Breast-Q™ Domain | Predicted Mean Difference | 95% CI | p | Predicted Mean Difference | 95% CI | p | |||||
| Preoperative | Satisfaction with breast | -1.1 | -8.2 | -- | 6 | 0.77 | -5.4 | -13.1 | -- | 2.3 | 0.17 |
| Psychosocial well-being | -11.4 | -14.4 | -- | -8.4 | < 0.01 | -13.3 | -16.6 | -- | -10 | < 0.01 | |
| Sexual well-being | -4.1 | -7 | -- | -1.2 | 0.01 | -6 | -9.2 | -- | -2.7 | < 0.01 | |
| Physical well-being | -6.7 | -15.7 | -- | 2.3 | 0.14 | -9.8 | -19.4 | -- | -0.1 | 0.047 | |
| Postoperative | Satisfaction with breast | 1.9 | -6.7 | -- | 10.5 | 0.67 | 1.9 | -6.7 | -- | 10.5 | 0.67 |
| Psychosocial well-being | -4.3 | -12.8 | -- | 4.2 | 0.32 | -4.1 | -13.8 | -- | 5.6 | 0.41 | |
| Sexual well-being | -4.9 | -15.6 | -- | 5.8 | 0.37 | -7.7 | -20.5 | -- | 5 | 0.24 | |
| Physical well-being | -3.7 | -11 | -- | 3.6 | 0.33 | -3.5 | -11.7 | -- | 4.8 | 0.41 | |
| Satisfaction with outcome | 1 | -4.7 | -- | 6.7 | 0.73 | 3 | -3.4 | -- | 9.3 | 0.36 | |
| Satisfaction with information | 0.7 | -6.9 | -- | 8.2 | 0.86 | 1.3 | -6.7 | -- | 9.4 | 0.75 | |
| Satisfaction with nipples | 3.5 | -4.7 | -- | 11.6 | 0.4 | 1.5 | -7.8 | -- | 10.9 | 0.75 | |
| Satisfaction with plastic surgeon | 0.3 | -5.2 | -- | 5.7 | 0.92 | -0.5 | -4.1 | -- | 3.1 | 0.78 | |
| Satisfaction with medical team | 1.8 | -2.8 | -- | 6.4 | 0.44 | 0.6 | -0.7 | -- | 2 | 0.36 | |
| Satisfaction with office staff | 1.7 | -4.1 | -- | 7.5 | 0.56 | 0.5 | -3.7 | -- | 4.7 | 0.82 | |
| Postoperative improvement | Satisfaction with breast | 2.9 | -8.2 | -- | 14 | 0.61 | 7.4 | -4.7 | -- | 19.4 | 0.23 |
| Psychosocial well-being | 6 | -6.2 | -- | 18.2 | 0.34 | 9.5 | -3.9 | -- | 22.8 | 0.17 | |
| Sexual well-being | 1.6 | -13 | -- | 16.3 | 0.83 | 3.8 | -12.5 | -- | 20 | 0.65 | |
| Physical well-being | 2.8 | -6.7 | -- | 12.3 | 0.56 | 6.7 | -3.5 | -- | 16.9 | 0.2 | |
Table 4 Generalized linear models determining the predicted mean difference in health-related quality of life and satisfaction BREAST-Q© scores for patients with marked breast asymmetry relative to those without it in a population of women who underwent reduction mammoplasty.
Assessment of surgeons’ assessment of symmetry
We found no correlation between surgeons’ asymmetry assessment and the definition based on difference of tissue excised we (R2=0.13; p=0.24).
Discussion
Asymmetry is common in the human body, especially in breasts. For patients with symptomatic macromastia and marked preoperative asymmetry, a RM can not only provide symptomatic relief, but can also be used as a balancing procedure to symmetrize the breasts. While the magnitude of improvement in PROs for patients undergoing RM may not relate to BMI, breast cup size, or amount of tissue resected the existing literature remains limited regarding the impact of breast asymmetry. We assessed clinical outcomes and PROs among patients with marked preoperative asymmetry using a cohort of 105 racially and ethnically diverse patients with symptomatic macromastia undergoing RM by two surgeons that have standardized practices for breast reduction. We found that these patients did start with lower QOL at baseline relative to those without asymmetry and that they achieved a significant improvement postoperatively that was comparable to the improvement experienced by patients without asymmetry. Moreover, there were no differences in clinical outcomes based on degree of asymmetry. Ultimately, this study quantifies the burden of macromastia as we showed psychosocial, sexual and physical well-being are significantly lower in patients with marked asymmetry independent of age and BMI.
Patients who suffer from symptomatic macromastia often seek surgical intervention, as they typically experience a high physical health burden inclusive of back and neck pain, headaches, shoulder grooving, and rashes. However, these patients also suffer from psychological implications of this condition, such as self-consciousness about breasts, social embarrassment, and low self-esteem [16]. PRO measures allow surgeons to capture such constructs from a patient perspective, to evaluate the impact of surgical interventions on patient symptoms and QOL, and to explore patient characteristics most correlated with QOL. Prior studies using PRO instruments have shown that RM significantly improves QOL and satisfaction in patients suffering from symptomatic macromastia a finding similar to our own. Specifically, in regards to breast asymmetry, prior data from an international study suggested that QOL by the BREAST-Q© following RM is greater for patient with significant asymmetry [11]. However, their study did not statistically compare these results and did not examine and account for preoperative differences in BREAST-Q© scores and important patient-level confounders. In our adjusted analyses controlling for age, BMI, brassier cup size and surgical technique, we demonstrated that marked preoperative asymmetry in patients with symptomatic macromastia is independently associated with higher burden of disease particularly in the physical, psychosocial, and sexual wellbeing domains (Table 4). These findings imply that breast asymmetry in patients with macromastia may cause additional psychological distress at baseline, perhaps as a result of patients being less confident and accepting of their bodies. In addition, this study highlights the importance of offering surgery to patients with substantial asymmetry given the major decrease in baseline PROs related to QOL, and it calls for consideration and even inclusion of asymmetry as an independent factor for insurance coverage. Moreover, these findings support prior studies encouraging insurers to consider PROs among the criteria for approval determination.
When comparing the preoperative and postoperative BREAST-Q© scores as an objective measure of the magnitude of PROs improvement, we found that both patients with symmetric and asymmetric breasts improved significantly relative to their baseline and that the magnitude of improvement between groups was comparable. While no studies had explored the association of breast asymmetry with regards to magnitude of PRO improvement, our results are in line with a study by Gonzalez MA, et al. [17] that showed that the improvement of QOL after RM does not depend on the amount of tissue resected.
Another important finding was that the preoperative BREAST-Q© scores were lower in our cohort compared to the general population regardless of the degree of asymmetry. However, existing population norms were derived from a mostly nondiverse population ( > 90% White) [18]. Therefore, future studies should account for these differences and efforts are needed to estimate the true burden of disease among minority patients with symptomatic macromastia to further discover underlying causes of such differences.
While this study shows differences in baseline PROs based on presence of breast asymmetry, there were no differences in clinical outcomes between the symmetric and asymmetric cohort (Table 2). Patients without breast asymmetry experienced an overall complication rate of 24.1%, while those with breast asymmetry had a rate of 26.9% (p=0.77), both of which are within the range previously described (7-51%) [19,20]. For patients with marked asymmetry, this is an especially important finding because it demonstrates that the risk of complications does not increase with the amount of tissue resected, as they served as an internal control with breasts of varying sizes. Nonetheless, it is important to note that around one in four patients may experience a complication when discussing the operative plan and counseling patients preoperatively.
The limitations of this study are its retrospective design, relatively small sample size (n=105), and short follow up at the time of QOL assessment, which make it is unclear whether these results are generalizable. For instance, the baseline QOL for the entire cohort was lower than population norms previously published. However, the strength of the study lies on describing the burden of disease associated with macromastia among racially diverse women by the degree of asymmetry. There are available classifications for the degree of asymmetry such as the one provided by Persichetti P, et al. [12]. However, this classification depends on the presumed volume to be resected, and as demonstrated in our sub analysis, surgeons’ asymmetry assessment prior to surgery does not correlate with marked asymmetry. Therefore, we chose to use the mass of breast tissue excised as this provides an objective measure to define patients that started off with a significant degree of asymmetry, as plastic and reconstructive surgeons will attempt to balance any asymmetry at the time of RM. Despite these limitations, our findings from this study have important implications as they can be used clinically by surgeons to guide treatment approaches and to counsel patients, as well as by policymakers to support the use of asymmetry as a factor for insurance approval.
Conclusion
Patients with symptomatic macromastia and marked breast asymmetry have a higher burden of disease that is significantly alleviated by RM. Surgeons should strive to achieve symmetric results irrespective of differences in tissue excised as clinical outcomes and the magnitude of QOL improvement are comparable between patients with and without asymmetry. These results highlight the need for policy changes to include asymmetry and PROs among the criteria for insurance coverage approval in order to facilitate access to care for these patients, especially since the burden of disease appears to be higher in racially diverse populations. Further efforts exploring factors contributing to such disparities are warranted to establish norms that account for race and ethnicity.
References
- Scutt D, Manning JT, Whitehouse GH, Leinster SJ, Massey CP (1997) The relationship between breast asymmetry, breast size and the occurrence of breast cancer. Br J Radiol 70: 1017-1021.
- Bauermeister AJ, Gill K, Zuriarrain A, Earle SA, Newman MI (2019) Reduction mammoplasty with superomedial pedicle technique: A literature review and retrospective analysis of 938 consecutive breast reductions. J Plast Reconstr Aesthetic Surg 72: 410-418.
- Blomqvist L, Eriksson A, Brandberg Y (2000) Reduction mammoplasty provides long-term improvement in health status and quality of life. Plast Reconstr Surg 106Z: 991-997.
- Chao JD, Memmel HC, Redding JF, Egan L, Odom LC, et al. (2002) Reduction mammoplasty is a functional operation, improving quality of life in symptomatic women: A prospective, single-center breast reduction outcome study. Plast Reconstr Surg 110: 1644-1652.
- Singh KA, Losken A (2012) Additional benefits of reduction mammaplasty: A systematic review of the literature. Plast Reconstr Surg 129: 562-570.
- Surgery AS of AP. Cosmetic (Aesthetic) Surgery National Data Bank. www.surgery.org. Accessed May 22, 2020.
- Thoma A, Sprague S, Veltri K, Duku E, Furlong W (2007) A prospective study of patients undergoing breast reduction surgery: Health-related quality of life and clinical outcomes. Plast Reconstr Surg 120: 13-26.
- Mundy LR, Homa K, Klassen AF, Pusic AL, Kerrigan CL (2017) Understanding the health burden of macromastia: Normative data for the BREAST-Q reduction module. Plast Reconstr Surg 139: 846e-853e.
- Collins ED, Kerrigan CL, Kim M, Lowery CJ, Striplin TD, et al. (2002) The effectiveness of surgical and nonsurgical interventions in relieving the symptoms of macromastia. Plast Reconstr Surg 109: 1556-1566.
- Wagner DS, Alfonso DR (2005) The influence of obesity and volume of resection on success in reduction mammoplasty: An outcomes study. Plast Reconstr Surg 115: 1034-1038.
- Cogliandro A, Barone M, Cassotta G, Tenna S, Cagli B, et al (2017). Patient satisfaction and clinical outcomes following 414 breast reductions: Application of BREAST-Q. Aesthetic Plast Surg 41: 245-249.
- Persichetti P, Cagli B, Tenna S, Simone P, Marangi GF, et al. (2005) Decision making in the treatment of tuberous and tubular breasts: Volume adjustment as a crucial stage in the surgical strategy. Aesthetic Plast Surg 29: 482-488.
- Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, et al. (2009) Development of a new patient-reported outcome measure for breast surgery: The BREAST-Q. Plast Reconstr Surg 124: 345-353.
- Coriddi M, Nadeau M, Taghizadeh M, Taylor A (2013) Analysis of satisfaction and well-being following breast reduction using a validated survey instrument: The BREAST-Q. Plast Reconstr Surg 132: 285-290.
- Regnault P (1976) Breast ptosis: Definition and treatment. Clin Plast Surg 3: 193-203.
- Rogliani M, Gentile P, Labardi L, Donfrancesco A, Cervelli V (2009) Improvement of physical and psychological symptoms after breast reduction. J Plast Reconstr Aesthetic Surg 62: 1647-1649.
- Gonzalez MA, Glickman LT, Aladegbami B, Simpson RL (2012) Quality of life after breast reduction surgery: A 10-year retrospective analysis using the breast Q questionnaire: Does breast size matter? Ann Plast Surg 69: 361-363.
- Cabral IV, Da Silva Garcia E, Sobrinho RN, Pinto NLL, Juliano Y, et al. (2018) Use of the BREAST-QTM survey in the prospective evaluation of reduction mammoplasty outcomes. Aesthetic Plast Surg 42: 388-395.
- Kerrigan CL, Slezak SS (2013) Evidence-based medicine: Reduction mammoplasty. Plast Reconstr Surg 132: 1670-1683.
- Ogunleye AA, Leroux O, Morrison N, Preminger AB (2017) Complications after reduction mammoplasty: A comparison of wise pattern/inferior pedicle and vertical scar/superomedial pedicle. Ann Plast Surg 79: 13-16.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences