The Preoperative Value for Surgical Cases in Obesity, Aiming at the Result : Zero Death
José Humberto Cardoso Resende
DOI10.4172/2472-1905.100035
José Humberto Cardoso Resende*
Alfredo Nasser UNIFAN, Goiânia-GO, Brazil
- *Corresponding Author:
- José Humberto Cardoso Resende
Faculty, Alfredo Nasser UNIFAN
Goiânia-GO, Brazil
Tel: (62) 3094-9494
Fax: (62) 3094-9714
E-mail: jresen99@hotmail.com
Received Date: January 16, 2018; Accepted Date: January 29, 2018; Published Date: February 05, 2018
Citation: Resende JHC (2018) The Preoperative Value for Surgical Cases in Obesity, Aiming at the Result: “Zero Death”. J Aesthet Reconstr Surg 4:1. doi: 10.4172/2472-1905.100035
Abstract
This is a manuscript that draws the attention of professionals involved with obesity and the dangers of guilt that have fallen on those involved with this pathology. The elaboration of scientific projects with greater participation of doctors, patients and decision making where the main word would be: “to want”. There is no weight loss with excess food, but with several attitudes to achieve the result: to observe the quantity and quality of food eaten. To achieve the final success of surgical procedures, a careful preoperative period is needed, such as hematocrit above 38%; glycemia below 105 mg/dL; blood pressure below 150 × 100 mmHg; vitamin D above 20 ng/ml; normal radiological examinations; compatible electrocardiogram and other tests necessary for each specific case. Because it is a public health problem, the obesity must have special attention by the public agents to have the professional success as a result. Let's imagine how much savings we would make for every kilogram of obese patients, especially those with medication for hypertension and diabetes. Today, we can rely on bariatric surgery and body-relief surgeries. We observe how much improvement we obtain for the work, effective life, clothing, leisure and joy of living of the patients graced with these indicated procedures. With all these preventive actions, the results that most caught our attention were “zero death” and “public health economics”.
Keywords
Obesity; Gigantomastia; Body relief surgery; Mammary gigantoplasty
Introduction
Besides observing the cure of the patient, one of the successes of medicine is to have the quality of life of the same ones with "zero death" in the race and satisfaction as a person as a professional result. The achievement of success will depend on a set of measures involving professions and conduct with the focus set in life. In nutrition, we analyzed measures and exams, BMI (Body Mass Index), nutritional methods, aiming at a body fat of biochemical parameters from childhood to adulthood. Speech therapy is concerned with the characterization of eating habits of obese patients and their results, ranging from the number of feeding times per day to the number of chewing times [1-3]. The value of this manuscript is in the study of each partner specialty. It is a public health problem due to the increase of obese people in the world and the deformities presented by the anatomical changes of the bodies, having relation even with the alteration of the human voice. The value of psychology covers the problems caused in the obese and, later, in the post-bariatric body changes [4]. All obese subjects answered questions with few differences and variations in responses, such as: “I almost do not eat, whenever I want I lose weight”; “My bones are great”; “I became obese after the wedding”.
Over the years, we have observed that success was in a careful preoperative period and with the participation of patients in the Workshops (multidisciplinary and explanatory meetings) and direct involvement of the obese people among themselves and with physicians, where they learned to speak: “I want”! With weight loss, we observed increased hematocrit, low blood glucose, normalization of blood pressure, low cholesterol, decreased BMI and increased self-esteem. [5-7]. The “zero death” is a consequence of correct attitudes of all the professionals involved with the client or patient. It is also linked to the correct release decision for plastic surgery or bariatric surgery, with normal laboratory tests, including being fit for all partner specialties [8]. Often, we first do the surgery of corporal relief, like the reduction of the breasts or the giant abdomens and later, we authorize the bariatric surgery. After the release of all these multidisciplinary specialties, including endocrinology with hormonal controls and surgical risk evaluated by clinicians, cardiologists, and anesthesiologists, we indicate surgeries and body areas that may lead to a lower surgical risk [9]. Plastic or bariatric surgery is indicated in cases where the classification of risk of death reaches ASA1 II, given by anesthetists.
In this manuscript, we present a summary of reports of 30 professional years dedicated to obesity with hundreds of successful operative acts, not counting the value of faith each health professional can influence in this result: “zero death” [10].
Case Presentation
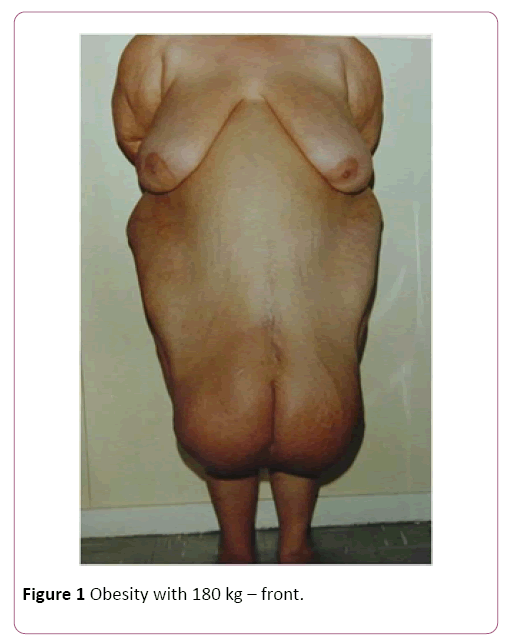
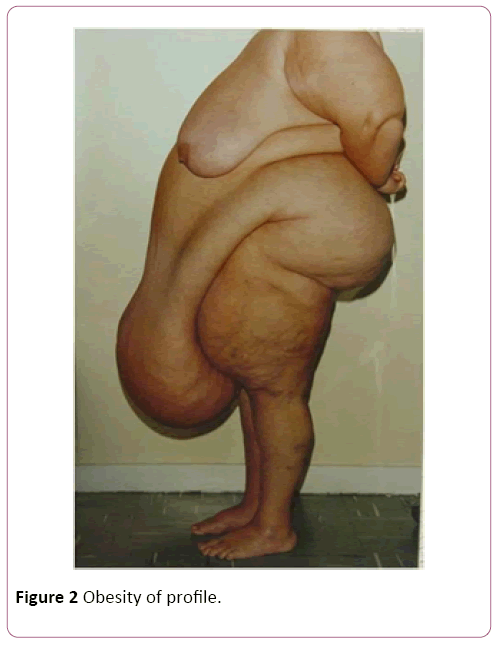
Among the hundreds of cases of the Plastic Surgery Service of the Federal Hospital of the Servants of the State of Rio de Janeiro, we selected 30 cases that we consider to be extremely high risk of death, considering the weight of the patients (Figures 1-4), format and location of body fat, abdomen or breast, and the impossibility or difficulty of anesthetic intubation due to the possibility of respiratory tamponade by the surgical table position or by excess fat [11].
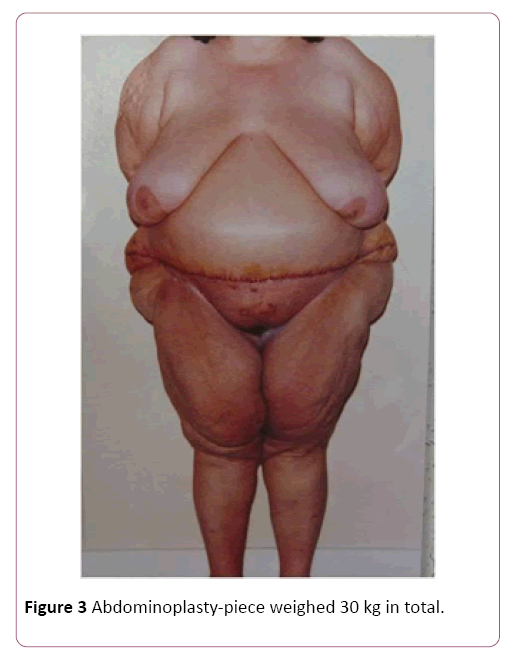
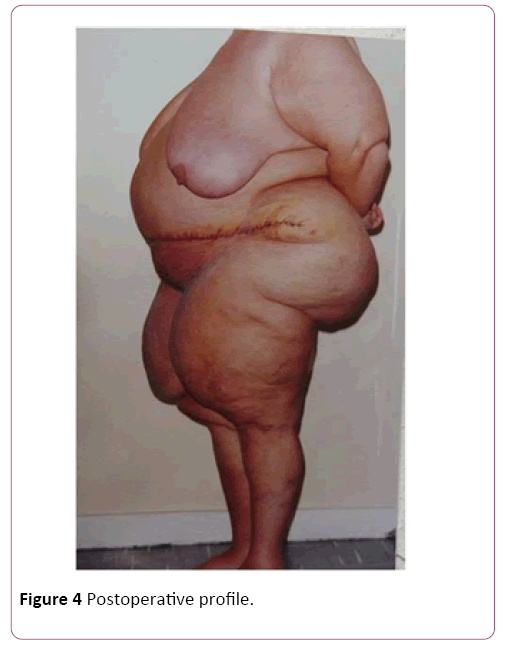
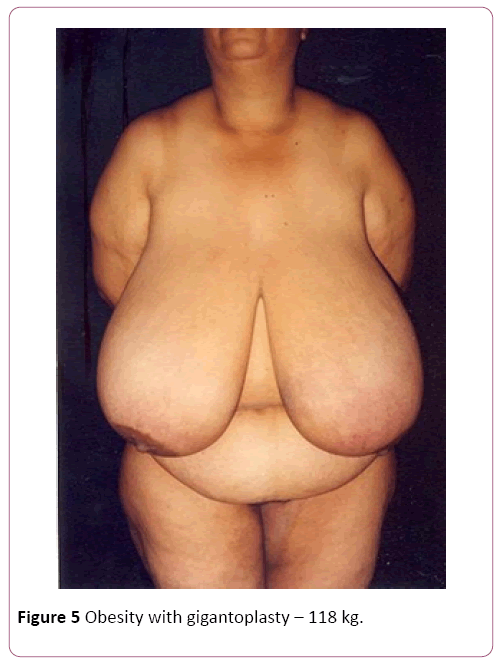
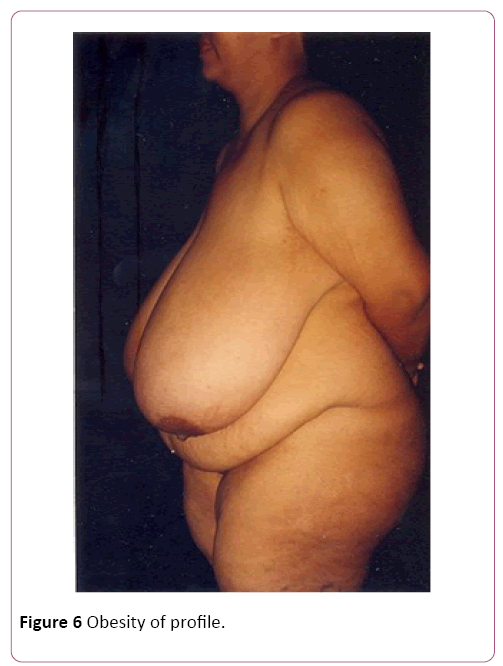
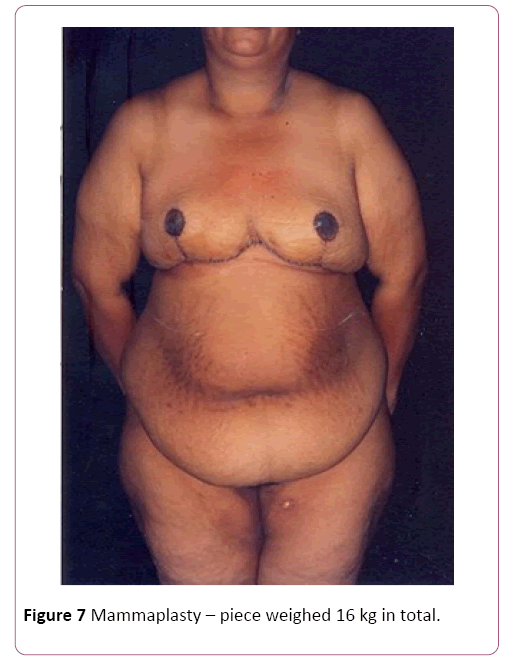
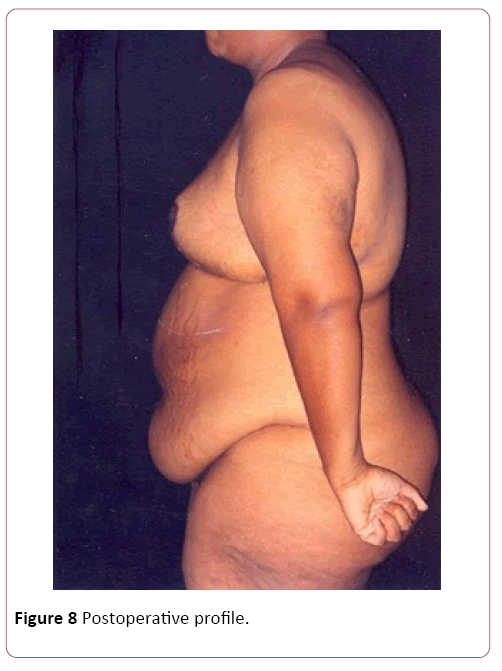
Of the 30 cases, 22 were of mammary gigantism, with the lowest weight of extirpation being 5 kg in each breast and 8 cases of abdominal gigantism with the lowest operative part of 8 kg, regardless of gender, color, occupation and purchasing power. In all cases of breasts, we used the Resende technique for gigantoplasty for body relief before bariatric surgery, and in the abdominoplasties, we performed amputations of the abdominal excess, without superior or lateral detachment to reduce the risk [12,13]. In the largest amputated breast, we removed 32 kg, 18 of the right breast and 14 of the left breast. In the abdomens, the largest operative piece weighed 30 kg in total (Figure 3). The raffias were performed all in three surgical planes: fascia, subcutaneous cellular, and skin, made of nylon. The dressings were semi-occlusive. Length of stay had an average of four days [14]. The withdrawal of stitches was from the 14th to the 21st day and the final high with 6 months. We only released the first restorative plastic surgery after one year of the body-relief surgery and for bariatric surgery at the same time [15,16]. The death rate was zero!
We showed some cases of body-relief surgery before we proceeded to bariatric surgery (Figures 5-8). Our final remark: We offered a little of our knowledge to a person who had zero hope of living well and with complete lack of quality of life. For the professionals, seeing the patients well and with joy would be a form of remuneration. Even though we know that besides to the body relief surgeries, we can have more than five reconstructive surgeries in the future. Professional satisfaction is in proportion to the results of the actions employed for each case. The ultimate focus has always been on success with “zero death” results.
Discussion and Conclusion
It was difficult in the past when there was no liposuction or bariatric surgery. We had to improvise with a fabulous courage to decide what to do if we wanted to keep such patients alive. We recognize that saying “it's easy to lose weight” is nothing more than a fantasy of the individual. All specialties have been perfected and have had great developments in obesity studies in recent years.
We came to the simple conclusion, but difficult to communicate that to be thin, to have surgical conditions is very important the collaboration and participation of patients. During all these years, we also found that after the first 5 kg of weight loss, the patient feels much better. Blood pressure, diabetes, general condition, disposition and quality of life improve, but losing weight is a difficult task!
When we implemented the Obese Workshop, in which we had 352 obese people in a single meeting, we saw the advance and a new hope emerging for those with this pathology. We create choral, occupational therapy, exchange of food recipes, appropriate physiotherapy, optimism activities and the main one for everyone, say: “I want, I will win, I am beautiful, I love myself, I like myself!” After the weight loss, in which we do not take into account the BMI, but the numerical proportion weight/height, as for example: 1.80 m=80 kg; 1, 58 m=58 kg; 1.64 m=64 kg, it was very easy for us and everyone said that only by decreasing the amount of food they started to lose weight. The success was so great that we had a case where the boy lost 103 kg without bariatric surgery and he was contemplated only with small reparative procedures: breasts and abdomen. Why do not we take BMI into account? Because an artist who did bodybuilding was considered strong and the owner of the bakery with the same weight was considered obese.
References
- Almeida ALJ, Amaral TCN (2008) Proper nutrition. Treat Plas Surg Obes, Rio de Janeiro. pp: 3-9.
- Pontes MBBF (2008) Nutritional evaluation. Treat Plas Surg Obes, Rio de Janeiro. pp: 11-41.
- Santos AC, Barroso LMBS (2008) The beginning of speech therapy in patients with obesity. Treat Plas Surg Obes, Rio de Janeiro. pp: 63-67.
- Okano CB (2008) Psychological evaluation for bariatric surgery. Treat Plas Surg Obes, Rio de Janeiro. pp: 87-88.
- Okano CB (2008) Criteria for release for plastic surgery. Treat Plas Surg Obes, Rio de Janeiro. pp: 103-104.
- Laun IC, Costa, RA, Benchimol IT, Mendes TP (2008) Obesity: Concept, etiology and classification. Treat Plas Surg Obes, Rio de Janeiro. pp: 107-110.
- Roitman IM (2008) Obesity and cardiovascular disease. Treat Plas Surg Obes, Rio de Janeiro. pp: 141-143.
- Diniz JAC (2008) Preanesthetic evaluation in the obese patient. Treat Plas Surg Obes, Rio de Janeiro. pp: 169-174.
- Chead MH, Kam PCA (2005) Obesity: Basic science and medical aspects relevant to anesthesia 60: 1009-1021.
- França AMAP, Lima M (2008) Physiotherapy in the preoperative and postoperative periods of plastic surgery in obesity. Treat Plas Surg Obes, Rio de Janeiro. pp: 197-214.
- Silveira VG, Carneiro JRI (2008) Clinical preparation of the patient with morbid obesity for bariatric surgery. Treat Plas Surg Obes, Rio de Janeiro. pp: 217-221.
- Silveira VG (2008) Surgical treatment of morbid obesity. Treat Plas Surg Obes, Rio de Janeiro. pp: 223-236.
- Meira AAM, Andrade IF, Ferreira FPM (2008) Plastic surgery after gastroplasty: A preoperative and postoperative approach. Rev Bras Cir Plást. 23(1): 15-21.
- Resende JHC (2008) Obesity workshop in plastic surgery or life workshop. Treat Plas Surg Obesity, Rio de Janeiro. pp: 239-244.
- Resende JHC (2008) Resende technique for correction of gigantism-surgery for body relief. Treat Plas Surg Obes, Rio de Janeiro. pp: 357-365.
- Daniel ASS. Circumferential excisions in the trunk and associations in obesity.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences