The Role of Doppler Ultrasound after Penile Replantation Surgery: A Case Report and a Systematic Review of the Literature
Fateme Tahmasbi1*, Farzin Soleimandzadeh2, Milad Shirvaliloo1, Mohammad H Dashti3 and Omidreza Sedigh4
1Department of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
2Department of Urology, Tabriz University of Medical Sciences, Tabriz, Iran
3Department of Surgery, Mubarak Al-Kabeer Hospital, Ministry of Health, Kuwait
4Department of Urologist, Molinette University Hospital, Turin, Italy
- *Corresponding Author:
- Fateme Tahmasbi
Department of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
Tel: 989039978444
E-mail: ftahmasbi997@gmail.com
Received Date:January 28, 2022, Manuscript No. IPARS-22-12402; Editor assigned date: January 31, 2022, Pre QC No. IPARS-22-12402 (PQ); Reviewed date: February 15, 2022, QC No. IPARS-22-12402; Revised date: March 30, 2022, Manuscript No. IPARS-22-12402 (R); Published date: May 09, 2022, DOI: 10.36648/2472-1905.8.3.006
Citation: Tahmasbi F, Soleimandzadeh F, Shirvaliloo M, Dashti HM, Sedigh O, et al. (2022) The Role of Doppler Ultrasound after Penile Replantation Surgery: A Case Report and a Systematic Review of the Literature. J Aestht Reconstrc Surg Vol:8 No:3
Abstract
Penile amputation is an uncommon surgical emergency in the urology field. Surgical replantation is one of the treatment options. The role of Doppler ultrasound in the post-operative period has not been sufficiently evaluated. We faced an equivocal condition in the case of penile replantation. This study is a report of this patient and a systematic review evaluating the available literature on the role of Doppler ultrasonography in this rare clinical condition. This is a case report of a patient with self-mutilation of the penis due to a psychological disorder managed by microsurgical replantation of the penis in which the early post-operative Doppler ultrasound results showed no arterial blood flow but the final result was quite satisfying. We performed a systematic review then to find the universal experience with Doppler ultrasound in penile replantation. We found a total of 14 reports that used Doppler ultrasound after penile replantation. These reports are quite rare and heterogeneous in terms of evaluation time and findings. We here summarized the results of all these studies narratively. Our experience like two other studies included in this systematic review shows that relying merely on the results of early post-operative Doppler ultrasound especially when it shows inappropriate blood flow, is not sufficient since the clinical result achieved with routine follow-up can be quite satisfactory in long term.
Keywords
Doppler ultrasonography; Penis; Replantation; Microscopic Replantation; Amputation
Introduction
In a urologic emergency, penile amputation is a severe type of penile injury, with iatrogenic or traumatic background, such as excessive excision during surgical procedures, or as a consequence of vehicular trauma, gunshot wounds, animal bites, and last but not least, self-mutilation [1]. In adults, partial or complete penile amputation is a rare condition that may occur following self-mutilation as a result of a psychotic episode mostly observed in individuals with an underlying psychological disorder, e.g., schizophrenia [2]. Regardless of the cause and immediate complications upon injury, the overwhelming squeal of severe penile injury necessitates timely management by expert clinicians [3].
Although a rare condition, several treatment modalities have been described for the management of penile amputation in the contemporary literature, each with different therapeutic outcomes [4]. As suggested; there are three primary surgical interventions for the management of an amputated penis based on the extent of injury: primary re-anastomosis or replantation, closure of the residual corpora cavernosa, or total phallic substitution [5]. Replantation is the intervention of choice, recommended to be attempted only if the injury is no more than 24 hours old or in other words when the amputated penis is still viable. Nearly 80 cases of penile amputation were reported from 1966 to 2007, according to a systematic review of the literature, with more than 30 successful cases of penile replantation.
In terms of prognosis, it would be difficult to determine the extent to which replantation of an amputated penis might be successful, as several factors can influence the therapeutic outcome [6]. The severity of the injury is perhaps the most important factor of all, followed by the duration of ischemia, incorporation of microscopy into the surgical repair of the severed neurovascular bundle, and last but not least, the expertise of the medical team available. Prior to the 1970 s, penile amputation was predominantly treated with macroscopic surgical procedures, in which corporal and urethral reapproximation or anastomosis was attained without microscopic repair of the dorsal neurovascular structures. As one should expect, such limited therapeutic intervention was often associated with unfavorable clinical outcomes such as penile skin and glans slough and necrosis, along with debilitating long-term effects, including urethral stricture and impotence. It was only after the 1975 when such poor clinical outcomes and complications began to show a descending trend in incidence, all thanks to the advent of microsurgical replantation techniques introduced first in Japan and the US. This novel surgical modality included the repair of dorsal arteries, the deep dorsal vein, and the dorsal nerve bundle, resulting in better post-operative genital sensation, erectile function and overall penile viability [4,7].
As the previous investigations suggest, a favorable outcome following penile replantation is mostly observed with cases in which the total duration of ischemia was less than 15 hours. Accordingly, primary closure of the residual penile stump is usually taken as the initial step in the management of penile amputation [8-12]. However, aside from an expertly conducted surgery, postoperative monitoring is also of significant importance in terms of clinical outcome. As such, early identification of vascular, particularly arterial compromise can significantly improve the prognosis of a penile replantation surgery. A cost-effective, time-friendly, and widely available imaging modality, Doppler ultrasound can be easily applied for point-of-care detection of potential postoperative disruptions in the blood flow of the re-anastomosed vessels [13]. Herein, we report a case of self-inflicted penile amputation, who was postoperatively monitored with Doppler ultrasound intermittently throughout his stay at the hospital.
Case Presentation
A 34 years old patient with self-inflicted penile amputation was admitted to the urology ward approximately two hours after amputation. The patient, with a history of psychotic disorder, had severed his penis with a kitchen knife following self-discontinuation of antipsychotic medications, which were not specified at the time.
Upon admission to the ED, the patient was conscious, with stable vital signs and ability to communicate verbally. However, he was reluctant to properly answer any questions of the attending physician. Allegedly, he did not have a history of substance or drug abuse. The severed penis had been brought to the hospital by his father in a small container filled with ice.
Subsequently, the patient was taken to the operating room in the fastest way, bypassing some of the time-consuming procedures. Careful examination under anesthesia revealed a fully and transversally transected urethra, as well as corporal bodies at the level of the penile base. The skin along with the penile stump and amputated penis was intact with no evidence of ischemia or necrotic changes. Prophylactic intravenous third-generation cephalosporin antibiotics were given. The patient was also vaccinated for tetanus.
During the surgery, the arteries were carefully designated and spatulated to be prospectively anastomosed. Similarly, the transected corpus spongiosum was spatulated and re-anastomosed. Corpus spongiosum was dissected from corpora cavernosain both sides for a tension free, spatulated anastomosis. Then, the ventral borders of the corpora cavernosa (3-0 PDS running sutures), followed by the left and right cavernosal arteries (five separate 9-0 Prolene sutures on each), dorsal margins of the corpora cavernosa (3-0 PDS running sutures), deep dorsal vein (six separate 9-0 Prolene sutures), and right dorsal artery of the penis (four separate 10-0 Prolene Sutures) were re-anastomosed under microscopic vision, respectively. Each of three anastomosed arteries was spatulated using tiny microvascular scissors on both sides prior to anastomosis. Due to the exceedingly low diameter, re-anastomosis of the left dorsal artery was not feasible and it was ligated carefully. Urethra was spatulated for about 6 mm on both sides and anastomosed by 4-0 Vicryl sutures on a 16 Fr silicone catheter. A Jackson-Pratt vacuum drain was placed finally, skin was circumferentially sutured and a low-press dressing was applied with a petroleum gauze layer directly on the suture line. Immediate psychiatric and forensic medical consults were implemented and their advice was re-ordered accordingly. Two days of complete bed rest with full dose heparin infusion was started right after surgery.
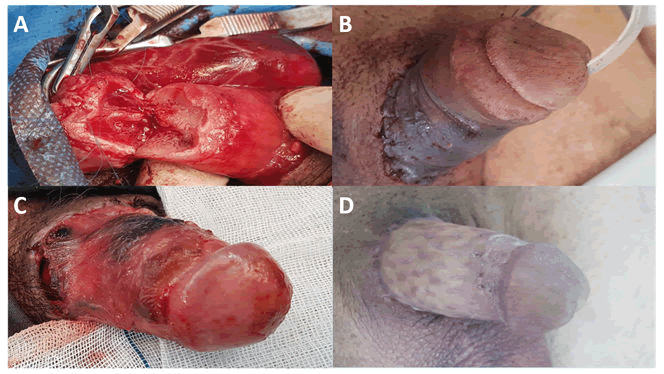
Skin color seemed nearly normal during the first 48 hours, but a color change appeared on the third day. We requested a penile Doppler ultrasound scan on the third post-operative day evening, which showed no arterial (neither cavernosal nor dorsal) blood flow, with only venous flow detectable at the dorsal vein. Doppler scan was repeated on postoperative day 4 and the result reported by another expert radiologist was the same. However, we followed the patient since glans was spongy and warm, although skin necrosis was established on postoperative day 5. On the postoperative day 11, due to complete replanted skin necrosis, we decided to do a necrotic skin debridement. This showed a quite normal penile body blood supply and viability. On postoperative day 16, patient was transferred to another university hospital for skin grafting he received a split thickness anterior thigh skin graft and discharged four days after second surgery. Patient was under supervision by his plastic surgeon for nearly two months after our last visit.
Seventy-four days after replantation, we visited the patient with a good skin graft condition, experiencing normal morning erections and voiding, as well as recovered penile glans sensation. Due to his clinical condition we did not evaluate for arterial patency or possible urethral stricture. He was, however, still reluctant to use his antipsychotic drugs in spite of his family’s attempts. Figure 1 demonstrates different post-operative stages.
Systematic Review
This systematic review was conducted in adherence to Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [14].
Information sources and search strategy
Online databases including PubMed, Scopus, Embase, Web of Science, and Google Scholar were thoroughly searched using the following keywords and their proper synonyms: "penile replantation", "penile amputation", "self-mutilation", "microsurgical replantation", "auto amputation". Different combinations of these terms were generated using Boolean operators. No time restriction was applied. The results were imported into the EndNote X8 reference manager. Two authors (F.T, M.S) excluded the studies if found irrelevant based on their title and abstract. Afterward, the remaining articles were evaluated, and if met the inclusion criteria, included in the study. Any disagreements between the two authors were resolved by referring to a third author (F.S).
Eligibility criteria
Studies that reported utilization of Doppler ultrasound after the replantation surgery for cases with penile amputation were included. Studies with amputation due to etiologies other than trauma, for instance, cancers, or other surgical methods including phalloplasty or reconstruction, non-English studies, animal studies, correspondences, editorials, commentaries, and review articles were excluded.
Data collection process
Two authors (F.T, M.S) independently extracted the following items in predefined Excel sheets; citation data (citation, publication date and origin), study design, causes of amputation, ischemia time, postoperative ultrasound and its results, skin condition after the replantation, and surgical outcomes.
Synthesis of results
Considering the type of the included studies and the vast heterogeneity among them, statistical analysis was neither feasible nor appropriate; therefore a narrative synthesis of the results was performed.
Results
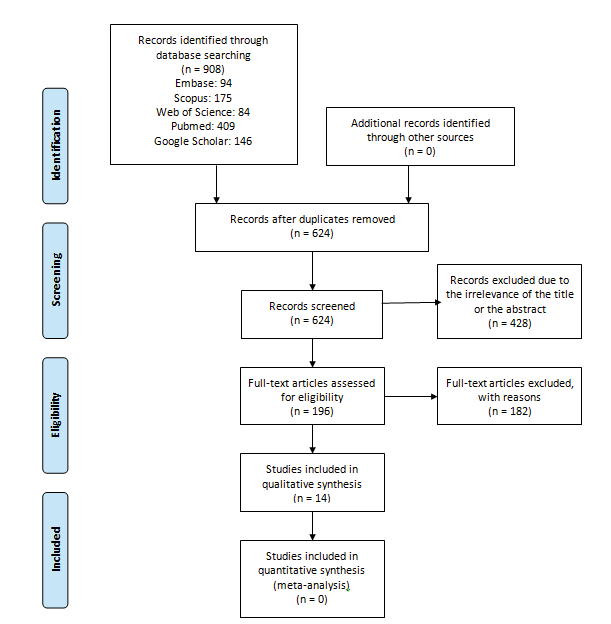
Figure 2 shows the study selection process. From a total of 908 studies, 624 studies remained after deduplication was eliminated. Based on a title and abstract review, 428 more studies were excluded and the remaining 196 were selected to be evaluated via full text and 182 articles were removed. We could not find the full-text manuscript of 16 studies. Finally, 14 were included in this systematic review [15-20].
All of the included studies were case reports of penile amputation with different causes, including assaults, accidents, circumcision complication, or self-mutilation induced by drugs and psychosis episodes [21-25]. One study reported self-amputation in a male patient without mentioning the underlying cause [26]. Different durations of ischemia were reported, ranging from immediate referral to a maximum of 16 hours' delay [27].
Postoperative Doppler ultrasound was conducted in 9 studies within one week 9 days 6 weeks [and 8 weeks following the replantation surgery. Furthermore, Doppler ultrasound was conducted in one study two months after the operation [4, 15-22, 24, 25]. In one study, Cook and transcutaneous Doppler were conducted during the surgery with no signals being detected [27].
Among all 14, two-third of the penis was lost in one study [19]. In another study, re-amputation was performed on day 10 due to the non-viability of the penis [26]. Other studies reported successful operation results in terms of the viability of replanted parts. Among the studies reporting first-week post-operative Doppler evaluation, two investigations reported no vascularity in Doppler ultrasound, three studies did not provide any information of the post-operative Doppler findings and one study reported that Doppler signal was positional, with complete loss of signal with adduction of the legs [18,19,26]. The rest of the studies reported adequate blood flow [16, 22, 25] Table 1.
| Author and year | Setting | Case | Cause of amputation | Ischemia time | Ultrasound use | Ultrasound findings | Post-surgical skin condition |
|---|---|---|---|---|---|---|---|
| Banihani | Panama | A7-day-old neonate | Ritualisticcircumcision | Lessthan 1 hour | Post-operation | Goodarterial signal at the end of the case | Theshaft and glans were swollen, warm and bled dark blood when punctured with aneedle |
| Yeniyol | Turkey | A56-year-old male | Self-amputation | 5hours to arrivaland 7 hours to revascularization | Afterone week | Novascularity | Afterone week the penis was darker while the glans seemed live |
| Raheem | USA | A19-year-old male | Traumaticself-amputation due to auditory hallucinations caused by methamphetamine use | >6hours | Post-operation,every 4 hour | AdequateDoppler flow | Excellentskin preservation and adequate wound healing |
| Patial | India | A9-year-old male | Traumaticamputation by patient's sister | Approximately12 hours | In4 days | Novascularity | Darkenedskin and necrosis set in by 4 days |
| Putra | Indonesia | A33-year-old male | Mechanicalgrass cutter trauma | 9hours | Fivedays after the surgery | Adequatedeep and superficial arterial flow at the distal end of the penis | |
| Razzaghi | Iran | A30-year-old male | Self-amputationdue to the schizophrenia | Approximately8 hours | 2ndand 9th postoperative day | Low-resistancearterial blood flow and normal venous flow distal to anastomosis | Necrosiswas observed at the base of the penile skin |
| Manganiello | USA | A24-year-old male | Self-amputationdue to the schizophrenia | Approximately3 hours and 15 minutes | For3 days post-operation | Edema,ecchymosis, and mild incisional skin necrosis | |
| Mosahebi | UK | A46-year-old male | Self-amputationdue to the psychosis | Approximately7 hours | 8weeks post-operation | Normalflow | Asmall area of skin necrosis of the degloved penile skin at the base of penile shaft |
| Facio | Brazil | A30-year-old male | Traumafrom a family conflict | 6hours (Warm ischemia: 5 hours, cold ischemia: 1 hour) | 2ndpostoperative day | Distalcavernous flow, with perviousness of the anastomosis and cavernous arteriesas well as the presence of peripheral venous flow. | Presenceof granulation tissue after slight necrosis of the skin |
| Garg | India | A34 year old male | Traumafrom an assault with a knife | 10hours (Warm ischemia: 2 hours) | 1.Post-op 2. Six weeks after the operation | Noresult for the post-op is reported but the Doppler US showed single dorsalpenile normal flow in addition to normal Doppler waveform changes in both ofthe cavernosal arteries suggesting the development of good collateral bloodflow | Necrosisin the scrotal skin and some skin over the dorsum of penis |
| Elmaraghi | USA | A52-year-old male | Boatingaccident | 1-2hours of cold ischemia time | Postoperative | TheDoppler signal was positional, with complete loss of signal with adduction ofthe legs | Lessthan 10% skin necrosis, requiring skin grafting |
| Salem | Egypt | A23-year-old male | Traumaticpenile amputation as a form of punishment for raping | 2hours | Duplexultrasound was performed 2 months after the operation | Gooderection after 10 min which lasted for 20 min for right cavernosal artery one and 35 ml/sfor the left one | Evidenceof venous stasis, oedema and segmental penile skin necrosis after 5 days ofsurgery |
| Roche | USA | A28-year-old male | Self-amputationdue to the schizophrenia | Immediately | Post-op,every 30 minutes | Moderatewound margin necrosis in 3 days on the ventral side of the penis | |
| Lu | USA | A22-year-old male | Self-amputationdue to psychosis | 16hours | Duringthe surgery | ACook Doppler over the repaired veins showed no signal, even though there wasclinical evidence of blood flow through the veins; transcutaneous Doppler didnot detect any signal over the veins as well |
Table 1: Summarizes the characteristics of the included studies in detail.
Discussion
With pertinent literature dating back to the 1850s, the first successful attempt at surgical correction of penile amputation, termed “penile replantation”, is perhaps the one reported by Ehrich in 1926 that discussed a case of self-mutilation with a radial saw [3]. Ever since, there has been a perceptible, though gradual, rise in the incidence of trauma-related penile amputation, with roughly 90 percent of cases being associated with a certain type of psychotic disorder [28].
A meta-analysis on successful reports of penile replantation in China, published over 48 years, from 1964 to 2012, revealed 109 cases that were successfully treated by surgery. According to this investigation by Li et al., the mean duration of ischemia in these patients was 6.3 ± 5.7 hours (varying from 1 to 38 hours). Out of 109 cases, 53 (49%) had undergone microscopic anastomosis of the amputated penis. Several postoperative complications were highlighted, the most prevalent of which, observed in 58 patients (53%), was penile skin necrosis; followed by decreased penile sensation (28%), urethral stricture (15%), erectile dysfunction (13%), and urethral fistulae (7%). The study suggested a positive correlation between the incidence of erectile dysfunction and non-microscopical methods of urethral and neurovascular bundle repair, as there was an increased incidence of this particular complication in patients who had undergone surgeries that did not adopt microscopy. A similar relationship was also denoted between the incidence of urethral stricture and the method of surgery. Not surprisingly, a higher number of anastomosed blood vessels was associated with less severe degrees of skin necrosis (P<0.05) [10].
A systematic review conducted by Jezior et al. on 19 cases of penile amputation reported a prevalence of 21% for erectile dysfunction. The study suggested a potential link between erectile function and meticulous approximation of dorsal structures and cavernously arteries in replantation surgery, in a way that more accurately placed anastomoses resulted in better erectile function. Nonetheless, it would still be a challenging task for the surgeon to precisely establish sufficient anastomoses in the case of distal penile injuries, due chiefly to the smaller size of vessels supplying the distal part of the penis. Accordingly, penile fibrosis and severe erectile dysfunction are the ultimate unfavorable outcomes in cases where microvascularsurgeryisnotfeasible[29].Theimportanceofmicrovascularrevascularization can be inferred from the literature, as it provides the penile shaft with a better blood flow, preserving the cavernosal and urethral structures from ischemia-induced fibrosis, and ultimate erectile and voiding dysfunction [25,29,30].
A highly practical imaging modality, Doppler ultrasound has mostly been overlooked in the management of penile amputation. To date, few studies have sought to evaluate the diagnostic and prognostic value of Doppler ultrasound in the postoperative monitoring of blood flow in the replanted penis, and estimating the therapeutic outcome, respectively. Over the last two decades, Doppler ultrasound was perhaps first mentioned in a case report, published in 2001, that noted intra and postoperative application of this modality aimed solely at monitoring the arterial blood flow immediately and 8 weeks after reanastomosis. A year later, Yeniyol et al. reported unsuccessful replantation of a case with the self-amputated penis, which was decided to undergo penile amputation surgery once Doppler ultrasound revealed no vascularity on the third day following replantation [26]. In 2009, two case reports of Middle-eastern origin were published, that addressed successful replantation of penile amputation. The first report from Egypt, by Salem et al., denoted acceptable erectile function and concomitant arterial blood flow, monitored with Doppler ultrasound, two months after the replantation of a traumatically amputated penis [17]. The other report from Iran, by Razzaghi et al., was concerned with a psychosis-induced case of self-amputation who had been referred to the hospital 8 hours after the injury. In this particular case, similar results were observed with Doppler ultrasound on the second and ninth days following replantation, indicating low-resistance arterial and normal venous blood flow distal to the anastomosis [24].
Further reports have been published on this condition throughout the last decade. In 2012, a paper by Roche et al., noted the intermittent application of Doppler ultrasound on a half-hourly basis for postoperative monitoring of a 28-year-old case with self-inflicted penile amputation, without providing further details [25]. Two years later, Doppler ultrasound was mentioned in a report on neonatal penile amputation due to ritualistic circumcision. In their paper, Banihani et al. reported successful penile replantation followed by immediate post-operative ultrasound monitoring that suggested good arterial flow [21]. In 2015, two reports included Doppler ultrasound in their case presentation, noting adequate arterial and venous blood flow in the distal section of the replanted penis [4,15]. One report, by Raheem et al., discussed the excellent prognosis achieved with a 19-year-old patient who had suffered traumatic amputation of the penis; highlighting satisfactory results observed with post-operative Doppler ultrasound examination [4]. In the other paper reported an interesting case of a severed penis as a result of trauma from a family conflict in Brazil. Following a successful penile replantation with a 6 hours’ time gap from the onset of injury, the 30 years old patient was postoperatively monitored with Doppler ultrasound on the second day after replantation and found to have sufficient distal cavernous arterial and peripheral venous flow [15]. In a similar account regarding a 34-year-old Indian patient in 2016, Garg et al. reported normal dorsal penile arterial flow, along with normal Doppler waveform changes in both cavernosal arteries, indicating successful development of collateral blood flow [16].
From 2017 to 2019, a total of three case reports of penile replantation, one from India and the others from the USA, were published. The oldest of the three reported an Indian 9-year-old case from 2017 with traumatic penile amputation, which underwent replantation with a poor prognosis, resulting in the necrosis of two-thirds of the reimplanted penis within 12 days from surgery. Doppler ultrasonography on the fourth day following surgery had failed to demonstrate any vascularity [19]. Later that year, Manganiello et al. mentioned the application of Doppler ultrasound in the post-operative monitoring of a 24 years old patient with self-amputation; without providing any detail regarding their findings [22]. Two years later, Lu KB, et al. reported negative results for Doppler ultrasound of a replanted penis in a 22-year-old patient despite significant clinical evidence regarding arterial and venous blood flow; denoting the ineffectiveness of this imaging technique in intraoperative monitoring of this patient, who continued to recover satisfactory urinary and sexual function within six months [27].
The most recent account, published in 2020, provides a more detailed perspective on the adoption of this imaging modality in the management of a 33 years old Indonesian male patient with incomplete penile amputation, who had been referred to the hospital 6 hours after the injury. The patient was immediately put under surgery, and evaluated with Doppler ultrasound on the fifth day following the surgery, shortly before being discharged, indicating the prognostic value of Doppler ultrasound in the follow-up of the surgery. Similar to the reports mentioned earlier, adequate deep and superficial arterial blood flow was revealed at the distal end of the penis [20]. In contrast to the clinically desirable findings reported by this study, a year earlier, in 2019, Elmaraghi et al. published an interesting and peculiar account of a 52 years old patient who had suffered severe traumatic avulsion penile injury following a boating accident. In this particular case, the arterial blood flow observed with post-operative Doppler ultrasound exhibited a position-dependent behavior, attenuating with adduction of the legs to the extent of complete loss of signal. Fortunately, the patient recovered his penile function, albeit, very gradually over three years [18].
Regarding other imaging modalities, predominantly Magnetic Resonance Imaging (MRI), previous work has only been focused on vascular abnormalities like priapism, Mondor disease, traumatic injuries including penile fracture and contusion, congenital anomalies in addition to penile malignancies [31-33]. Hence, current literature fails to provide adequate knowledge on the value of MRI in following clinical cases of penile amputation.
Strengths and limitations
Though bearing several limitations, this study is the first to address the role of Doppler ultrasound after microvascular penile replantation in the current literature. Lack of evidence for supporting scientific accuracy and reliability, in addition to the heterogeneous setting of the existing scholar, was among the obstacles that our study faced.
Conclusion
Regardless of the meager number of studies concerned with the clinical value of Doppler ultrasound in the management of penile amputation, the ultimate result reported by the majority of the investigations discussed above implies a correlation, albeit slight, between post-operative Doppler ultrasound monitoring and the final therapeutic outcome for the patient, warranting further research on this particular subject. Nonetheless, our experience –like two other studies included in this systematic review shows that relying merely on the results of early postoperative Doppler ultrasound especially when it shows inappropriate blood flow, is not sufficient since the clinical result achieved with routine follow-up is quite satisfactory in long term.
References
- Furr J, Culkin D (2017) Injury to the male external genitalia: a comprehensive review. Int Urol Nephrol 49:553-561
- Djordjevic ML, Bizic M, Stojanovic B, JoksicI, Bumbasirevic UV, et al. (2019) Outcomes and special techniques for treatment of penile amputation injury. Injury 50:131-136
- Salehipour M, A Ariafar (2010) Successful replantation of amputated penile shaft following industrial injury. Int J Occup Environ Med 1:198-200
- Raheem OA, Mirheydar SH, Patel ND, Patel HS, Suliman A, et al. (2015) Surgical management of traumatic penile amputation: a case report and review of the world literature. Sex Med 3:49-53
- Chang AJ, SB Brandes (2013) Advances in diagnosis and management of genital injuries. Urol Clin North Am 40:427-438
- Selby EA, Bender TW, Gordon KH, Nock MK, Joiner TE, et al. (2012) Non-suicidal self-injury (NSSI) disorder: a preliminary study. Personal Disord 3:167-175
- Rosenblum L, Burnett AL (2013) Microsurgical Penile Revascularization, Replantation, and Reconstruction. In: Sandlow J. (eds) Microsurgery for Fertility Specialists, Springer, New York.
- Abaka N, Ghoundale O, Touiti D (2013) Genital self-amputation or the Klingsor syndrome: Successful non-microsurgical penile replantation. Urol Ann 5:305-308
- Leyngold MM, Rivera-Serrano CM (2014) Microvascular penile replantation utilizing the deep inferior epigastric vessels. J Reconstr Microsurg 30:581-584
- Li GZ, Man LB, He F, Huang GL (2013) Replantation of amputated penis in Chinese men: A meta-analysis. Zhonghua Nan Ke Xue J androl 19:722-726
- Riyach O, Majdoub AE, Tazi MF, Ammari JEE, Fassi MJE, et al. (2014) Successful replantation of an amputated penis: a case report and review of the literature. J Med Case Rep 8:1-3
- Tazi MF, Ahallal Y, Khallouk A, Jamal Elfassi M, Farih MH, et al. (2011) Spectacularly successful microsurgical penile replantation in an assaulted patient: One case report. Case Rep Urol 2011:865489
- Klifto KM, Caresse F, Gurno MSN, Stella M. Seal MLS, et al. (2020) Comparison of arterial and venous implantable Doppler postoperative monitoring of free flaps: Systematic review and meta-analysis of diagnostic test accuracy. Microsur 40:501-511
- Moher D, Altman DG, Liberati A, Tetzlaff J (2011) PRISMA statement. Epidemiol 22:128
- Facio Jr FN, Spessoto LC, Arruda P, Paiva CS, Arruda JG, et al. (2015) Penile replantation after five hours of warm ischemia. Urol Case Rep 3:77-79
- Garg S, Gupta A, Baliarsing AS (2016) Successful microsurgical replantation of an amputated penis. Indian J Plast Surg 49:99-105
- Salem H, T Mostafa (2009) Primary anastomosis of the traumatically amputated penis. Androl 41:264-267
- Elmaraghi S, Chen TJ, Heckman JE, Shiau MJ, Williams HD, et al. (2020) Functional penile replantation after traumatic avulsion amputation below the pubis: a case report. Microsur 40:70-73
- Patial T, G Sharma, P Raina (2017) Traumatic penile amputation: a case report. BMC Urol 17:1-4
- Putra DE, Kusbin TBA, Satyagraha P, Widodo ST (2020) Case Report: Non-microscopic surgical management of incomplete penile amputation. F1000Res 9:681
- Banihani OI, Fox JA, Gander BH, Grunwaldt LJ, Cannon GM, et al. (2014) Complete penile amputation during ritual neonatal circumcision and successful replantation using postoperative leech therapy. Urol 84:472-474
- Manganiello MD, Knaus WJ, Cohen JB, Lee BT (2017) Penile Self-amputation. J Reconstr Microsurg Open 2:58-62
- Mosahebi A, Butterworth M, Knight R, Berger L, Kaisary A, et al. (2001) Delayed penile replantation after prolonged warm ischemia. Microsurg 21:52-54.
- Razaghi MR, Rezaei AR, Mazloumfard MM, Javanmand B, Mojtaba MH, et al. (2009) Successful macrosurgical reimplantation of an amputated penis. Urol J 6:306-308
- Roche NA, Vermeulen BT, Blondeel PN, Stillaert FB (2012) Technical recommendations for penile replantation based on lessons learned from penile reconstruction. J Reconstr Microsurg 28:247-250
- Yeniyol CO, Yener H, Keçeci Y, Ayder AR (2002) Microvascular replantation of a self-amputated penis. Int Urol Nephrol 33:117-119
- Lu KB, Sanneic K, Stone JA, Morey A, Amirlak B, et al. (2019) Success of penile replantation using combination of cialis, hyperbaric oxygen, and SPY technology. Eplasty 19:2
- Simopoulos EF, Trinidad AC (2012) Two cases of male genital self-mutilation: an examination of liaison dynamics. Psychosom 53:178-180
- Jezior JR, Brady JD, Schlossberg SM (2001) Management of penile amputation injuries. World J Surg 25:1602-1609
- Biswas G (2013) Technical considerations and outcomes in penile replantation. In Seminars in plastic surgery, Thieme Medical Publishers 333 Seventh Avenue, New York, USA.
- Lindquist CM, Nikolaidis P, Mittal PK, Miller HF (2019) MRI of the penis. Abdom Radiol 45:2001-2017
- Vossough A, Pretorius E S, Siegelman E S, Ramchandani P, Banner M P, et al. (2002) Magnetic resonance imaging of the penis. Abdom Radiol 27:640-659
- Tu LH, Spektor M, Ferrante M, Mathur M (2020) MRI of the Penis: Indications, Anatomy, and Pathology. Curr Probl Diagn Radiol 49:54-63
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences