Three-Layer Aesthetic and Functional Reconstruction of Full-Thickness Nasal Defects: Patient and Surgeon Subjective Evaluation
Sherif A Hantash, Ahmed A Elhefnawy, Wael H Mahmoud*, Tarek G Shoukr and Mohamed M Khedr
Department of Plastic Surgery, Tanta University, Tanta, Egypt
Published Date: 2023-09-19DOI10.36648/2472-1905.9.3.160
Sherif A Hantash, Ahmed A Elhefnawy, Wael H Mahmoud*, Tarek G Shoukr and MohamedMKhedr
Department of Plastic Surgery, Tanta University, Tanta, Egypt
- *Corresponding Author:
- Wael H Mahmoud
Department of Plastic Surgery,
Tanta University, Tanta,
Egypt,
E-mail: waelhussein558@gmail.com
Received date: August 18, 2023, Manuscript No. IPARS-23-17718; Editor assigned date: August 21, 2023, PreQC No. IPARS-23-17718 (PQ); Reviewed date: September 05, 2023, QC No. IPARS-23-17718; Revised date: September 12, 2023, Manuscript No. IPARS-23-17718 (R); Published date: September 19, 2023, DOI: 10.36648/2472-1905.9.3.160
Citation: Hantash SA, Elhefnawy AA, Mahmoud WH, Shoukr TG, Khedr MM (2023) Three-Layer Aesthetic and Functional Reconstruction of Full- Thickness Nasal Defects: Patient and Surgeon Subjective Evaluation. J Aesthet Reconstr Surg Vol.9 No.3: 160.
Abstract
Background: Reconstruction of large full-thickness nasal defects poses a challenge to reconstructive surgeons. We aimed in this prospective study to subjectively evaluate aesthetic and functional outcomes of three-layer reconstruction of large full-thickness nasal defects, with a cross-paramedian forehead flap as the skin coverage, a turnover nasolabial flap and/or septal mucoperichondrial hinge flap as the lining, and a conchal cartilage graft as the framework, using specific validated scores.
Methods: Between March 2020 and March 2023, 35 patients (28 males; mean: 58.4 ± 7.94 years), with large full- thickness nasal defects secondary to oncological resection, underwent nasal reconstruction by our adopted technique. Evaluation of the outcomes was done by the Nasal Appearance and Function Evaluation Questionnaire (NAFEQ) score and the Visual Analog Scale (VAS) score.
Results: All the flaps survived without major complications. The complication rate was 17.2% (n=6); 1 wound infection, 2 marginal superficial necroses, 1 hypertrophic forehead scar and 2 bulkiness of the nasal ala. Regarding the NAFEQ score, the mean values were (30.1 ± 3.2) and (32.9 ± 1.7) for the functional and aesthetic parts respectively. The mean value for the VAS score was (31.3 ± 3.5). All subjects were satisfied with the nasal appearance while 86% were satisfied with the nasal functioning. The follow-up period ranged from 9 to 24 months.
Conclusion: This method is a feasible, safe and reliable reconstructive option for large full-thickness nasal defects. Usage of specific validated scores for outcomes evaluation enables us to understand the nuances between different techniques that could possibly result in higher patient satisfaction.
Keywords
Nasal reconstruction; Full-thickness nasal defects; Cross-paramedian forehead flap
Introduction
The nose plays an important role in facial harmony and proportions. It serves not only as an aesthetic facial subunit, but also as a functional organ [1]. Nasal defects are commonly encountered following trauma and tumor extirpation [2]. The nose is particularly vulnerable to cutaneous malignancies, making it the most common location for presentation. About 15%-50% of the basal cell carcinomas within the head and neck region are found on the nose [3]. Local excision of nasal tumors with the requisite safety margin may result in a full-thickness defect [4]. Reconstruction of nasal defects created by oncological resection, especially with the duality of the nasal form and function, can be quite challenging [5].
In full thickness defects, all three layers; the mucosa or lining, the osteo-cartilaginous framework or support and the skin or cover needs to be replaced optimally. Otherwise, the reconstruction will be unstable and functional impairment not solved [6]. The forehead has been acknowledged as the finest donor site for external nose covers due to its similarity to the nasal skin [7]. To shape the nose, create a strong support and brace the repair against gravity and subsequent contractions, the middle layer should be reconstructed using conchal or rib cartilage grafts [8]. Reconstruction of the lining is still the most challenging part of nose reconstruction. Ideally, this layer should be thin, soft and well vascularized [9]. In the past, the undersurface was allowed to heal secondarily, leading to alar retraction and/or vestibular stenosis [10]. Subsequently, different techniques have been described such as turnover flaps, pre-laminated forehead flaps, septal mucosal hinge flaps, skin grafts, composite grafts and free tissue transfer [11,12].
A great variety of reconstructive techniques has been developed by many authors. A unique reconstructive procedure or a combination of them can be utilized to achieve complete restoration attending to cosmetic and functional regard [13]. However, full-thickness nasal defect generally necessitates the use of axial pattern flaps such as the forehead flap and/or the nasolabial flap to provide an adequate blood supply to sustain the flaps themselves and for the interposed cartilage graft [4]. The authors of the current study have adopted a technique for reconstruction of large full-thickness nasal defects, using a combined cross-paramedian forehead flap as a skin coverage, a subcutaneously pedicled turnover nasolabial flap and/or septal mucoperichondrial hinge flap as the nasal lining and a conchal cartilage graft as the cartilaginous framework. We aimed in this study to subjectively evaluate the aesthetic and functional outcomes of our adopted technique in three-layer reconstruction of large full-thickness nasal defects using specific validated scores for nasal reconstruction.
Materials and Methods
This prospective study included 35 patients, 28 male and 7 female, with nasal defects secondary to oncological resection that were admitted to the Plastic Surgery Department, Tanta University Hospitals between March 2020 and March 2023. Included were patients with large (>1.5 cm) and full-thickness (including mucosa) nasal defects. Patients aged <18 years, and those with history of prior nose surgery or bleeding disorders were excluded. All patients underwent three-layer nasal reconstruction with a combined cross-paramedian forehead flap as a skin coverage, a subcutaneously pedicled turnover nasolabial flap and/or septal mucoperichondrial hinge flap as the nasal lining and a conchal cartilage graft as the cartilaginous framework after approval of our University Ethical Committee and written informed consent regarding the treatment, photography and research publishing was obtained.
Surgical technique
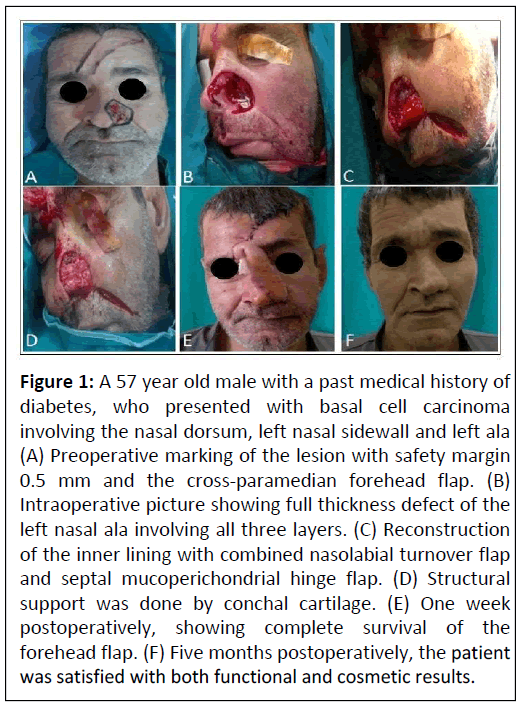
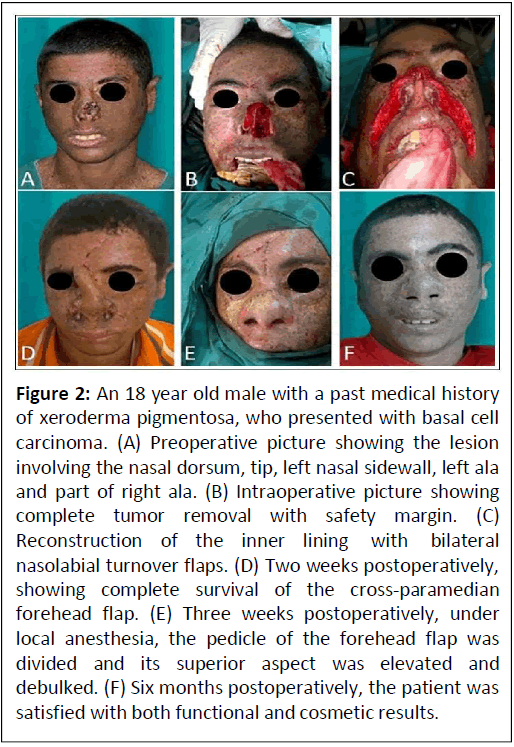
All procedures were performed under general anesthesia. The lesion was resected with at least 0.5 cm margin of the surrounding tissue and a tumor-free margin was confirmed by frozen section. At first, each defect exceeded 50% of the respective nasal subunit; adjacent normal tissue was discarded to reconstruct the subunit as a whole. The lining was reconstructed using subcutaneously pedicled turnover nasolabial flap, or ipsilateral septal mucoperichondrial hinge flap or a combination of these techniques. The flaps were reversed sutured to the remaining nasal mucosa with multiple closely situated interrupted absorbable sutures (Vicryl 4-0, Ethicon). A crescent-shaped conchal cartilage graft was inserted over the internal lining for stabilization of the nasal ala. The medial and lateral edges of the cartilage graft were secured into the tip region and the base of the ala respectively by non-absorbable mattress sutures (Prolene 4-0, Ethicon). After marking the size of the lost skin, an oblique paramedian forehead flap from the contralateral side (cross-paramedian forehead flap) was dissected as skin coverage. The forehead flap was elevated in the sub-cutaneous plane distally (2 cm) and then converted to sub-muscular plane up to arterial origin (1.5 cm above the orbit), where the plane was converted to sub-periosteal. The forehead flap was meticulously sutured to the wound edges of the surrounding external skin with interrupted sutures (Prolene 6-0, Ethicon). Tension-free closure of all donor sites with(Prolene 6-0, Ethicon) was accomplished in all cases. Vaseline- soaked gauze or plastic stent was inserted into the nasal hole tosupport the reconstructed ala (Figures 1 and 2).
Figure 1: A 57 year old male with a past medical history of diabetes, who presented with basal cell carcinoma involving the nasal dorsum, left nasal sidewall and left ala (A)Preoperative marking of the lesion with safety margin0.5 mm and the cross-paramedian forehead flap. (B)Intraoperative picture showing full thickness defect of theleft nasal ala involving all three layers. (C) Reconstructionof the inner lining with combined nasolabial turnover flapand septal mucoperichondrial hinge flap. (D) Structuralsupport was done by conchal cartilage. (E) One weekpostoperatively, showing complete survival of theforehead flap. (F) Five months postoperatively, the patientwas satisfied with both functional and cosmetic results.
Figure 2: An 18 year old male with a past medical history of xeroderma pigmentosa, who presented with basal cell carcinoma. (A) Preoperative picture showing the lesion involving the nasal dorsum, tip, left nasal sidewall, left ala and part of right ala. (B) Intraoperative picture showing complete tumor removal with safety margin. (C) Reconstruction of the inner lining with bilateral nasolabial turnover flaps. (D) Two weeks postoperatively, showing complete survival of the cross-paramedian forehead flap. (E) Three weeks postoperatively, under local anesthesia, the pedicle of the forehead flap was divided and its superior aspect was elevated and debulked. (F) Six months postoperatively, the patient was satisfied with both functional and cosmetic results.
Intravenous antibiotics were prescribed for 48 hours followed by five days of oral antibiotics. Suture removal was done at 10-14 postoperative days. After three weeks, under local anesthesia, the pedicle of the forehead flap was divided and its superior aspect was elevated and debulked. In the following, all patients were evaluated for the occurrence of early postoperative complications in terms of hematoma, venous congestion, partial or total flap necrosis, wound dehiscence and infection. The follow-up visits were designed to be once monthly for 6 months and then every 3 months for two years. Standardized digital photographs were taken prior to the treatment and during the follow-up visits.
Outcome assessments
Patient evaluation: The Nasal Appearance and Function Evaluation Questionnaire (NAFEQ) score, a validated 14-item questionnaire for evaluation of the outcomes following nasal reconstruction [14]. Table 1 was used to measure subjective functional and aesthetic self-evaluation of the outcomes. Function (questions: 1-7) and appearance (questions: 8-14) are the two parts that make up this score on a scale of 1 to 5. Increased scores indicate higher satisfaction, where 35 is the maximum score for each part.
| Observations | Always | Mostly | Every now and then | Hardly ever | Never |
|---|---|---|---|---|---|
| 1. How often do you have trouble breathing through your nose? | 1 | 2 | 3 | 4 | 5 |
| 2. How often do you snore? | 1 | 2 | 3 | 4 | 5 |
| 3. How often can you smell odors? | 1 | 2 | 3 | 4 | 5 |
| 4. How often do you have trouble with nasal crusts? | 1 | 2 | 3 | 4 | 5 |
| 5. How often do you have a bloody nose? | 1 | 2 | 3 | 4 | 5 |
| Very poor | Poor | Moderately | Good | Excellent | |
| 6. How do you assess your quality of speech? | 1 | 2 | 3 | 4 | 5 |
| Very dissatisfied | Dissatisfied | Moderately | Satisfied | Very satisfied | |
| 7. How satisfied are you with your total nasal functioning? | 1 | 2 | 3 | 4 | 5 |
| 8. How satisfied are you with your nasal tip appearance? | 1 | 2 | 3 | 4 | 5 |
| 9. How satisfied are you with your nasal wing(s) appearance | 1 | 2 | 3 | 4 | 5 |
| 10. How satisfied are you with your nasal dorsum appearance? | 1 | 2 | 3 | 4 | 5 |
| 11. How satisfied are you with the size of your nostril(s)? | 1 | 2 | 3 | 4 | 5 |
| 12. How satisfied are you with the color of your nasal skin? | 1 | 2 | 3 | 4 | 5 |
| 13. How satisfied are you with your nasal position? | 1 | 2 | 3 | 4 | 5 |
| 14. How satisfied are you with your total nasal appearance? | 1 | 2 | 3 | 4 | 5 |
Table 1: Items of the Nasal Appearance and Function Evaluation Questionnaire (NAFEQ) [13].
Surgeon evaluation: Subjective evaluation of the aesthetic outcomes was also accomplished by three independent plastic surgeons who were blinded to the nature of the study and evaluated postoperative clinical photographs using Visual Analog Scale (VAS) scores on a scale of 1 to 5 (1=least satisfied and 5=most satisfied). Increased scores indicate better appearance. In this regard, nose aesthetics were assorted into 8 categories: Nose contour, nostril, alar shape, nasal symmetry, flap thickness, hair growth, color matching and donor site scar.
SPSS for Windows (Version 18.0, SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Quantitative data were expressed as range and mean ± Standard Deviation (SD), whereas qualitative data were expressed as number and percent.
Results
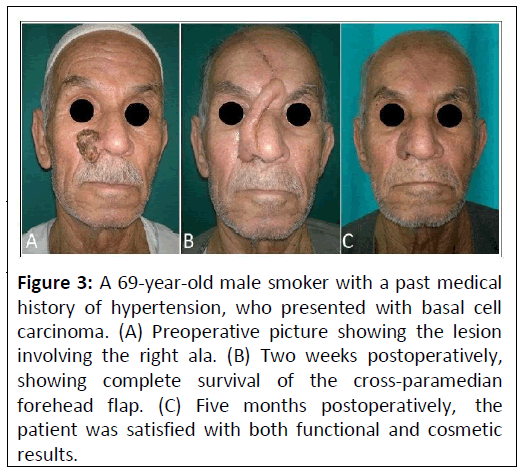
Over a 3-year period, 35 patients with large full-thickness nasal defects after oncological resection were included in the study. Out of these, 28 patients were males (80%) and 7 were females (20%). The mean age of patients was 58.4 ± 7.94 years (range: 18-70 years). Table 2 shows that five patients were smokers (14.3%), 3 had Type II diabetes (8.6%), 2 had arterial hypertension (5.7%) and 1 had ischemic heart diseases (2.9%). The tumor removed was Basal Cell Carcinoma (BCC) in thirty-four patients (97.1%), while was Squamous Cell Carcinoma (SCC) in one patient (2.9%) and was classified as T1N0M0 according to the "7th American Joint Committee on Cancer Staging Manual". Defect sizes ranged from 1.6 to 5.7 cm (mean: 2.8 ± 0.75 cm). In most of the cases (n=25) (71.5%), three aesthetic subunits including the ala were reconstructed. One patient (2.9%) had an isolated alar defect (Figure 3). We reconstructed five aesthetic subunits in one patient (2.9%), four subunits in three patients (8.6%) and two subunits in five patients (14.3%). The lining was reconstructed using subcutaneously pedicled turnover Nasolabial (NL) flap (n=27) (77.1%), ipsilateral septal mucoperichondrial hinge flap (n=3) (8.6%) and a combination of flaps (n=5) (14.3%). Separation of the para median forehead flap pedicle was performed after a mean period of 3.06 ± 0.2 weeks (range: 3-4 weeks).
| Characteristic | Value |
|---|---|
| Age, years | |
| Range | 18-70 |
| Mean ± SD | 58.4 ± 7.94 |
| Sex, n (%) | |
| Male | 28 (80%) |
| Female | 7 (20%) |
| Co-morbidities, n (%) | |
| Diabetes mellitus | 3 (8.6%) |
| Hypertension | 2 (5.7%) |
| Ischemic heart disease | 1 (2.9%) |
| Smoking | 5 (14.3%) |
| Tumor type, n (%) | |
| Basal Cell Carcinoma (BCC) | 34 (97.1%) |
| Squamous Cell Carcinoma (SCC) | 1 (2.9%) |
| Size of defect, cm | |
| Range | 1.6-5.7 cm |
| Mean ± SD | 2.8 ± 0.75cm |
| Internal nasal lining, n (%) | |
| Nasolabial (NL) turnover flap | 27 (77.1%) |
| Septal mucoperichondrial hinge flap | 3 (8.6%) |
| Combination of flaps | 5 (14.3%) |
| Follow up, months. | |
| Range | 9-24 |
| Mean ± SD | 13.2 ± 2.55 |
| Complications, n (%) | 6 (17.2%) |
| Wound infection | 1 (2.9%) |
| Marginal superficial necrosis | 2 (5.7%) |
| Hypertrophic forehead scar | 1 (2.9%) |
| Bulkiness of the nasal ala | 2 (5.7%) |
Table 2: Summary of patient data (N=35).
Figure 3: A 69-year-old male smoker with a past medical history of hypertension, who presented with basal cell carcinoma. (A) Preoperative picture showing the lesion involving the right ala. (B) Two weeks postoperatively, showing complete survival of the cross-paramedian forehead flap. (C) Five months postoperatively, the patient was satisfied with both functional and cosmetic results.
All the flaps survived without major complications and no tumor recurrences occurred in our population. All donor sites healed with inconspicuous scar except in one case that developed hypertrophic forehead scar. The total complication rate was 17.2% (n=6). One patient (2.9%) had infection of the auricular donor site that resolved with oral antibiotic therapy, two patients (5.7%) developed marginal superficial partial- thickness necrosis of the paramedian forehead flap that was treated conservatively, one patient (2.9%) developed hypertrophic forehead scar that was treated by topical silicone gel sheet and two patients (5.7%) suffered from bulkiness of the nasal ala which was treated by debulking of the flap.
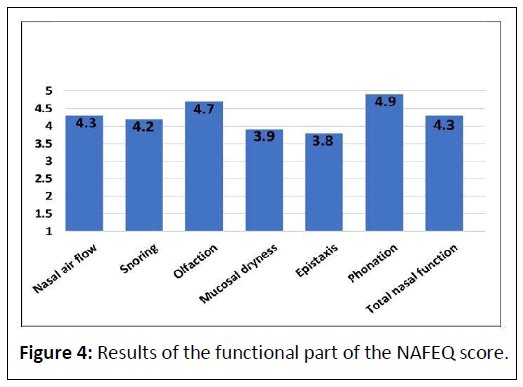
After a mean follow-up period of 13.2 ± 2.55 months (range: 9-24 months), 86% of our cases were satisfied with the overall nasal functioning. Regarding the functional part of the NAFEQ score, the mean was 30.1 ± 3.2 (range: 26-35). The detailed results of the functional part are shown in Figure 4.
In general, all the subjects were satisfied with the overall nasal appearance (68% were very satisfied and 32% were satisfied). With respect to the aesthetic appearance part of the NAFEQ score, the mean was 32.9 ± 1.7 (range: 30-35). Importantly, 90% of cases were satisfied with the nasal position and 85% with their nasal tip appearance and nasal dorsum appearance, whereas 80% of cases were satisfied with their nasal wings’ appearance and nasal skin color and 75% with their nostrils’ size. Concerning the independent plastic surgeon’s evaluation of the aforementioned nasal aesthetic perspectives using VAS scores, the mean was 31.3 ± 3.5 (range: 28-40). The detailed results of the subjective plastic surgeons’ evaluation are shown in Table 3.
| Characteristics | Mean ± SD |
|---|---|
| Nose contour | 4.0 ± 0.87 |
| Nostril shape | 3.7 ± 0. 91 |
| Alar shape | 3.6 ± 0.91 |
| Nasal symmetry | 4.0 ± 0.96 |
| Flap thickness | 3.2 ± 0.73 |
| Hair growth | 4.0 ± 0.82 |
| Color matching | 4.3 ± 0.56 |
| Donor site scar | 4.5 ± 0. 96 |
Table 3: Results of the subjective plastic surgeons’ evaluation.
Discussion
The nose provides a smooth transition from eyes to lips, so deformed one is very noticeable and can destroy the overall facial harmonics. It plays a functional role as well by providing airway patency [7]. The reconstruction of nasal defects especially large full-thickness ones can pose a significant challenge to the reconstructive surgeon, due to the complex three-dimensional anatomy which is difficult not only to recreate but also to maintain [6]. In this respect, reconstruction goal includes elegant restoration of near normal nasal form and function with a concomitant little morbidity in a cost-effective fashion [15]. Reconstructive technique or a combination of them must be selected according to the size and location of the defect created, what remains after complete tumor removal and medical comorbidities, taking into consideration the desired outcomes and the expertise of the surgeon. Therefore, a meticulous anatomical reconstruction, must be achieved as far as possible trying to restore the nasal lining, skeletal support and skin coverage to achieve satisfactory outcomes [13]. In this study, we aimed to subjectively evaluate aesthetic and functional outcomes of three-layer reconstruction of large full- thickness nasal defects, with a cross-paramedian forehead flap as a cutaneous coverage, a turnover nasolabial flap and/or septal mucoperichondrial hinge flap as the nasal lining and a conchal cartilage graft as the framework, using specific validated scores for nasal reconstruction; the Nasal Appearance and Function Evaluation Questionnaire (NAFEQ) score and the Visual Analog Scale (VAS) score.
We considered nasal defects greater than 1.5 cm in diameter to be large. Comparable to our study, Rohrich, et al., [16] and Shah, et al., [17] deemed defects >1.5 cm as large, 1-1.5 cm as medium, and less than 1 cm in diameter as small. In contrast to our work, Yoon, et al., [13] and Yong, et al., [18] classified defects larger than 2.5 cm as large defects, 1.5-2.5 cm as medium defects and defects less than 1.5 cm as small defects. According to our observations, basal cell carcinoma predominates (97.1%) among our patients, which is consistent with other studies [1,4,10].
In this study, the nasal lining was resurfaced by ipsilateral septal mucoperichondrial hinge flap in 3 cases (8.6%), subcutaneously pedicled turnover Nasolabial (NL) flap in 27 cases (77.1%) and a combination of both flaps in 5 cases (14.3%). We demonstrated that replacement of the nasal lining ought to be the primary consideration in full-thickness nasal defects. In the study of Yoon, et al., [13], the nasal lining was reconstructed by nasolabial turnover flap in 4 cases, folded forehead flap in one case, ipsilateral septal mucoperichondrial hinge flap in one case and composite graft from the root of the helix in one case. In another study Menick, et al., [19] elucidated that the residual intranasal lining could be elevated, based on either the septal branch of the superior labial artery; the ipsilateral septal mucosa can pivot from the septal surface to line the lower lateral nose, or on the superior ethmoidal arteries; the contralateral septal mucosa can be swung laterally entering via a slit in the ipsilateral septum. Although, these pliable and thin intranasal lining flaps serve as a support for primary cartilage grafts they are destructive to the residual intranasal anatomy, may be unavailable because of previous injury and are limited in dimension. Gostian, et al., [10] evaluated the efficacy of multiple quilting sutures to secure full- thickness skin grafts, as a nasal lining, on the undersurface of the forehead flap for reconstruction of full-thickness nasal defects in 16 patients. They found that this technique allows for reliable survival of the skin grafts and amends the reconstruction of the inner nasal lining in full-thickness nasal defects.
In our study, we effectively used the conchal cartilage graft as the structural support in all patients. We noticed that any attempt to reconstruct a full-thickness nasal defect without structural support will likely result in both an unaesthetic reconstruction and incompetence of the external nasal valve. Boyd, et al., [20] utilized auricular cartilage in 41 patients, septal cartilage in 6 patients, combined auricular and septal cartilage in 17 patients and combined septal cartilage and bone in 2 patients as structural support for full-thickness nasal defects. They noted that septal cartilage is usually flat and is particularly useful in middle-third defects, while conchal cartilage is curved and is ideal for providing support to alar and tip defects. In another study, Westerveld, et al., [21] used a composite nasal septum flap for lateral support and internal lining in reconstruction of large three-layer nasal vestibular defects. They demonstrated that the combination of a composite hinged-door septal flap with a paramedian forehead flap is an effective reconstruction procedure for lateral nasal wall and alar region defects. Fernández, et al., [6] recommended the use of titanium mesh as a structural support for reconstruction of large full-thickness nasal defects, where the use of cartilage grafts could be compromising.
We used the cross-paramedian forehead flap for skin coverage in all our patients, which is based on the contralateral supratrochlear artery and designed obliquely across the forehead and may extend along the inferior hairline. We noticed that this extension allowed us to add flap length without including the hair-bearing scalp. This design also provides a better arc of rotation, which enables the creation of a thinner pedicle and, as a result, a more aesthetically pleasing donor site scar that can be hidden in the glabellar crease. In a similar study Rudolph, et al., [22] reported that the cross-paramedian forehead flap is a reliable tool in the reconstructive armamentarium for large and complex nasal defects. In another study, Agostini, et al., [23] used the bi-pedicled forehead flap to reconstruct large full-thickness defects by restoring the nasal lining with a transposition flap and the nasal skin by a contralateral specular flap. Consequently, this reconstructive technique is feasible for reconstructing full-thickness nasal defects of varying sizes of the whole nasal framework. Saleh, et al., [7] advocated the use of the island forehead flap in total nasal reconstructions even in the multi-morbid patient. They noted that the forehead represents a maximum tissue reservoir for reconstructing large full-thickness defects of the nose, any subunit can be reconstructed even the alar rim and the vestibular lining by the paramedian forehead flap. Yoo, et al., [24]used the nasolabial flap and septal mucosal hinge flap forreconstruction of full-thickness alar defects and found thatforehead flaps might be inadequate in Korean patients with arelatively short forehead length.
In our series, we observed that no tumor recurrences during the follow up period or significant flap necrosis occurred in our population. However, few complications were encountered in six patients (17.2%), of whom four were smokers (11.4%); 1 patient had wound infection, 2 developed marginal superficial partial- thickness necrosis, 1 developed hypertrophic forehead scar and 2 suffered from bulkiness of the nasal ala which were treated by debulking of the flap, while all other complications were managed conservatively. In a similar study, El-shaer, et al., [25] observed that there were no major complications and no recurrences of the tumor during the follow-up period, while minor complications in the form of mild to moderate infection occurred in 2 cases and superficial sloughing affected 2 cases. All complications were treated conservatively, with no need for reoperations. In another study Javaid, et al., [26] found that the incidence of complications was (20%); 1 had flap tip necrosis, 2 had hyper pigmented and hypertrophic scar at suture line, 1 had bulkiness of the nasal ala, 1 had alar collapse and 2 had alar retrusion. In a larger study, Yong, et al., [18] noticed that complications were encountered in 27 patients (8.6%), of whom 2 were smokers; 11 patients had pin cushioning, 5 had wound dehiscence, 4 had wound infections, 3 had lateral ala and/or facial webbing, 2 had hematomas, 1 had a standing cutaneous deformity that was revised, and 1 patient had composite graft failure.
Our study demonstrated that all the subjects were satisfied with the overall nasal appearance while 86% were satisfied with the total nasal functioning. Regarding the subjective patient evaluation of the outcomes using the NAFEQ score, the mean values were (30.1 ± 3.2) and (32.9 ± 1.7) for the functional and aesthetic parts respectively. Concerning the subjective plastic surgeon evaluation of the aesthetic outcomes using VAS scores, the mean value was (31.3 ± 3.5). Similar to our findings, Noel, et al., [1] reported that 84% of the patients were satisfied with their total nasal functioning and all the patients were satisfied with their total nasal appearance. They noted that the median NAFEQ scores were 31 and 30 for the functional and aesthetic parts respectively. Moolenburgh, et al., [14] showed that the NAFEQ can be utilized as a standardized questionnaire for a thorough assessment of the outcomes of nasal reconstruction. Widespread use would make it possible to compare various techniques, surgeons and centers in a standardized and reproducible manner, which could also affect the outcome satisfaction. Also, Kim, et al., [8] demonstrated that the subjective plastic surgeon evaluation of the outcomes after full nasal reconstruction with a forehead flap using VAS scores were (4.36 ± 0.76), (4.26 ± 0.80) and (3.21 ± 1.03) for nose contour, nasal asymmetry and nostril shape respectively. In a similar study, Ghassemi, et al., [4] utilized a reverse nasolabial flap to restore the nasal lining, an auricular cartilage for structural support and a forehead flap for skin coverage of the full- thickness nasal defects in 21 patients following tumor extirpation. They noticed that all patients were satisfied with the aesthetic and functional outcomes and only 3 cases needed revision for the correction of the residual deformities. In a larger study, Boyd, et al., [20] assessed the functional and aesthetic results of forehead flap in reconstruction of 147 cases of nasal defects after Mohs excision of non-melanoma skin cancer and found that 68 patients (46.3%) needed debulking of the flap. However, high aesthetic and functional goals were achieved in all patients.
A limitation of the present study is the rather small sample size and the short follow-up period. To address this problem, we recommend further larger controlled studies with longer follow up periods for better evaluation of the esthetic and functional outcomes of full-thickness nasal defects reconstruction by our adopted technique.
Conclusion
This method is a feasible, safe and reliable option that can be applied successfully for the reconstruction of large full-thickness defects of the nose. Moreover, flaps originate from different donor sites that can be reduced in size, allowing for easier and tension-free primary wound closure which will ultimately offer low surgical morbidity and amend the functional and aesthetic outcomes. Furthermore, usage of specific validated scores for detailed evaluation of the outcomes after nasal reconstruction would enable us to understand the nuances between different techniques that could possibly result in higher patient satisfaction.
References
- Noel W, Duron JB, Jabbour S, Revol M, Mazouz-Dorval S (2018) Three-stage folded forehead flap for nasal reconstruction: Objective and subjective measurements of aesthetic and functional outcomes. J Plast Reconstr Aesthet Surg 71: 548-56.
[Crossref], [Google Scholar], [Indexing]
- Zelken JA, Reddy SK, Chang CS, Chuang SS, Chang CJ et al. (2017) Nasolabial and forehead flap reconstruction of contiguous alar-upper lip defects. J Plast Reconstr Aesthet Surg 70: 330-335.
[Crossref], [Google Scholar], [Indexing]
- Angermayer ME, Rangwani SM, Anderson SR, Johnson RM, Kadakia SP (2023) Forked paramedian forehead flap combined with nasolabial flap for pre-radiation coverage of exposed maxilla in the total rhinectomy patient. Am J Otolaryngol44: 103825.
[Crossref], [Google Scholar], [Indexing]
- Ghassemi A, Ahmed SS, Ghanepur H, Modabber A (2017) Three-layer reconstruction of lower third nasal defects using forehead flap, reversed nasolabial flap, and auricular cartilage. Int J Oral Maxillofac Surg 46: 36-40.
[Crossref], [Google Scholar], [Indexing]
- Madattigowda R (2020) Total nasal reconstruction using three layered forehead paramedian pedicle flap, rib graft and skin graft. Br J Oral Maxillofac Surg 58: e178.
[Crossref]
- Fernández CP, Castiñeiras GJ, Rodríguez PMÁ (2020) Reconstruction of a full-thickness nasal alar defect with a titanium mesh. Actas Dermosifiliogr (Engl Ed) 111: 265-268.
[Crossref], [Google Scholar], [Indexing]
- Saleh DB, Dearden AS, Smith J, Mizen KD, Reid J et al. (2020) Single-stage nasal reconstruction with the islanded forehead flap. J Plast Reconstr Aesthet Surg 73: 1692-1699.
[Crossref], [Google Scholar], [Indexing]
- Kim MJ, Choi JW (2021) Total nasal reconstruction with a forehead flap: Focusing on the facial aesthetic subunit principle. J Plast Reconstr Aesthet Surg 74: 1824-31.
[Crossref], [Google Scholar], [Indexing]
- Haack S, Fischer H, Gubisch W (2014) Lining in nasal reconstruction. Facial Plast Surg 30: 287-299.
[Crossref], [Google Scholar], [Indexing]
- Gostian A, Balk M, Stegmann A, Iro H, Wurm J (2020) Full-thickness skin grafts and quilting sutures for the reconstruction of internal nasal lining. Facial Plast Surg 36: 297-304.
[Crossref], [Google Scholar], [Indexing]
- Seth R, Revenaugh PC, Scharpf J, Shipchandler TZ, Fritz MA (2013) Free anterolateral thigh fascia lata flap for complex nasal lining defects. JAMA Facial Plast Surg 15: 21-28.
[Crossref], [Google Scholar], [Indexing]
- Zenga J, Chi JJ (2017) Reconstruction of the intranasal lining. Facial Plast Surg 33: 67-73.
[Crossref], [Google Scholar], [Indexing]
- Yoon T, Benito-Ruiz J, García-Díez E, Serra-Renom JM (2006) Our algorithm for nasal reconstruction. J Plast Reconstr Aesthet Surg 59: 239-247.
[Crossref], [Google Scholar], [Indexing]
- Moolenburgh SE, Mureau MA, Duivenvoorden HJ, Hofer SO (2009) Validation of a questionnaire assessing patient's aesthetic and functional outcome after nasal reconstruction: The patient NAFEQ-score. J Plast Reconstr Aesthet Surg 62: 656-662.
[Crossref], [Google Scholar], [Indexing]
- Lu GN, Kriet JD, Humphrey CD (2017) Local cutaneous flaps in nasal reconstruction. Facial Plast Surg 33: 27-33.
[Crossref], [Google Scholar], [Indexing]
- Rohrich RJ, Griffin JR, Ansari M, Beran SJ, Potter JK (2004) Nasal reconstruction-beyond aesthetic subunits: A 15-year review of 1334 cases. Plast Reconstr Surg 114: 1405-1416.
[Crossref], [Google Scholar], [Indexing]
- Shah AR, Zoumalan R, Constantinides MS (2008) Aesthetic repair of small to medium-sized nasal defects. Facial Plast Surg 24: 105-119.
[Crossref], [Google Scholar], [Indexing]
- Yong JS, Christophel JJ, Park SS (2014) Repair of intermediate-size nasal defects: A working algorithm. JAMA Otolaryngol Head Neck Surg 140: 1027-1033.
[Crossref], [Google Scholar], [Indexing]
- Menick FJ (2007) Defects of the nose, lip, and cheek: Rebuilding the composite defect. Plast Reconstr Surg 120: 887-898.
[Crossref], [Google Scholar], [Indexing]
- Boyd CM, Baker SR, Fader DJ, Wang TS, Johnson TM (2000) The forehead flap for nasal reconstruction. Arch Dermatol 136: 1365-1370.
[Crossref], [Google Scholar], [Indexing]
- Westerveld GJ, Middelweerd RJ, Leemans CR (2001) The hinged-door composite septal flap as structural support and lining of nasal reconstruction by a forehead flap. Rhinology 39: 5-8.
[Google Scholar], [Indexing]
- Rudolph MA, Walker NJ, Rebowe RE, Marks MW (2019) Broadening applications and insights into the cross-paramedian forehead flap over a 19-year period. J Plast Reconstr Aesthet Surg 72: 763-770.
[Crossref], [Google Scholar], [Indexing]
- Agostini T, Perello R, Russo GL, Spinelli G (2013) Through-and-through nasal reconstruction with the bi-pedicled forehead flap. Arch Plast Surg 40: 748-753.
[Crossref], [Google Scholar], [Indexing]
- Yoo HM, Lee KS, Kim JS, Kim NG (2014) Reconstruction of full thickness ala defect with nasolabial fold and septal mucosal hinge flap. Arch Craniofac Surg 15: 133-137.
[Crossref], [Google Scholar], [Indexing]
- El-Shaer W, Enab A, El-Noamani S (2010) Aesthetic reconstruction of composite alar base defects after rodent ulcer excision. Kasr El Aini J Surg 11: 29-36.
- Javaid M, Ahmad A, Khan Q, Wahid F, Afridi HR (2011) Outcome of nasolabial flap in reconstruction of the nasal alar defect. J Med Sci 19: 163-166.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences