Traumatic Cloaca; Surgical Treatment of a Disabling Deformity
Massimo Mongardini and Menelaos Karpathiotakis
DOI10.4172/2472-1905.100001
Department of Surgical Sciences, “Sapienza” University of Rome, “Umberto I” University Hospital, viale Regina Elena, Roma, Italy.
- *Corresponding Author:
- Menelaos Karpathiotakis
Department of Surgical Sciences, “Sapienza” University of Rome, “Umberto I” University Hospital
viale Regina Elena 324, 00161 Roma, Italy
Tel: +390649976440
E-mail: enimdisify@hotmail.it
Received date: September 19, 2015; Accepted date: September 23, 2015; Published date: September 30, 2015
Citation: Mongardini M, Karpathiotakis M. Traumatic Cloaca; Surgical Treatment of a Disabling Deformity. J Aesthet Reconstr Surg. 2016, 1:1. doi: 10.4172/2472-1905.10001
Editorial
Traumatic cloaca is a disabling deformity of the anus and vagina caused by the severe damage of the sphincter apparatus and of the perineal body, resulting in a common aperture for the rectum and vagina, as in congenital cloaca [1-4,9].
The most common cause is major obstetric injury occurred by median episiotomies that lead to third and fourth degree perineal lacerations, unrecognized or not repaired properly. The incidence is approximately 0.3% of all complicated vaginal deliveries. The resulting deformity is characterized by three-dimensional destruction of the perineal body, anterior disruption of the sphincter complex and loss of the distal rectovaginal septum of varying length. [1-4,7,9] Other rare causes of traumatic cloaca may be severe injuries in women victims of sexual violence or by grave accidents in sports like cycling.
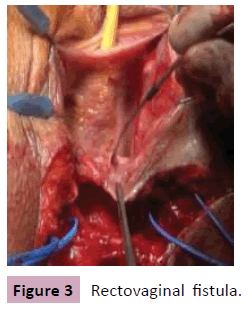
The disorders resulting by traumatic cloaca are mostly functional. These patients have severe fecal and flatus incontinence and symptoms similar to a rectovaginal fistula because of the lack of the distal rectovaginal septum. Consequently, most women suffer from grave perineal skin irritation and recurrent vaginal and urinary tract infections. Furthermore, difficulties con sexual activity is significant. Many women complain of dyspareunia or complete abstinence from sexual activity [1-4].
All these problems for the patients may lead to social distress and psychological disorders. The loss of voluntary evacuation control, although not a life threating disease, is a physical and psychological aggression to these women, resulting in progressive social isolation, alterations in the body image, anxiety and depression. A conservative approach from both the patients and physicians may lead to delay in treatment and diminished the quality of life [1-4,9].
A detailed history-taking and careful physical exam of the perineal body is often enough to make diagnosis of traumatic cloaca. Additional diagnostic tests, as endoanal ultrasound, anal manometry, transanal pudendal nerve stimulation, defecated MRI and Wexner incontinence score, can be performed in order to plan the appropriate surgical repair.
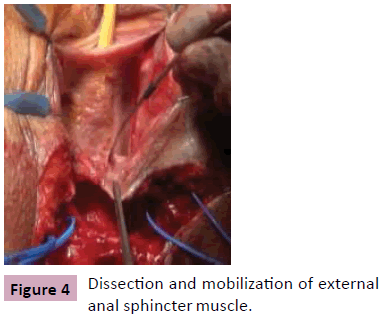
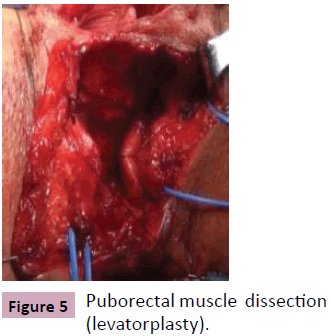
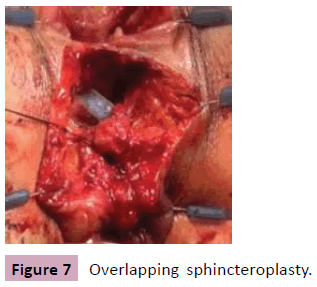
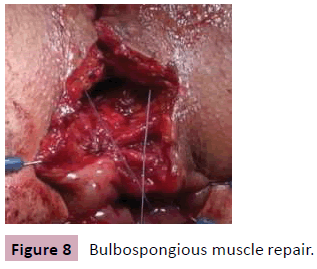
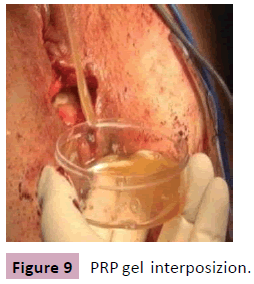
Various techniques have been described in the literature for repairing traumatic cloaca [1-9]. One of the surgical strategies most commonly used at our institution consists in a reconstructive plastic surgery of the perinal body (perineoplasty) and of the rectovaginal septum with puborectalis muscle interposition (levatorplasty) and overlapping external sphincteroplasty. In two cases we modified this procedure by introducing the use of PRP gel (Platelet Rich Plasma) with the aim to facilitate proper tissue regeneration and consolidate the plastic reconstruction of perineal body.
Thus, between 2010 e 2014 two women with traumatic cloaca were submitted to surgical treatment by our team. Either patient had an open rectovaginal communication with a large anterior sphincter defect and total incontinence. The mean patient age was 36 years and the cause of the cloaca was obstetrical trauma with fourth degree perineal laceration in one patient and sexual violence with severe perineal tearing in the other patient. Primary fecal diversion with loop sigmoidostomy was performed in one patient.
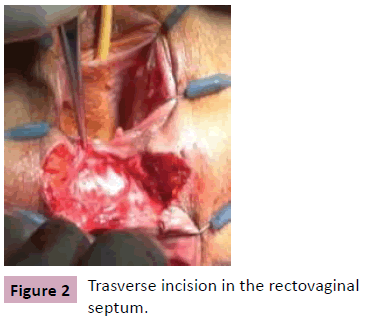
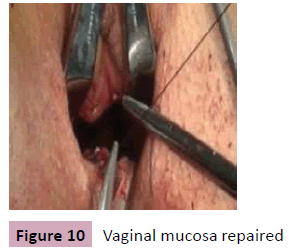
In both patients the surgical technique we performed consisted of a trasverse skin incision between the anus e vagina, dissection of the ischiorectal fossae bilaterally up to the level of the levator muscles, division of the rectovaginal septum up to the level of the puborectalis muscle, mobilizzation of the sphincter complex, overlapping sphincteroplasty of the external anal sphincter, reconstruction of the perineal body by plicating the puborectalis muscle to the midline (levatorplasty) and repair involving flats across the perineum in one patient [2-5,9]. In addition, we decide to proceed with the interposition of PRP gel over the levatorplasty e sphincteroplasty , while the skin closure was performed vertically in order to create a high –profile perineum (Figure 1-11).
With the aim to minimize the risk of complications (hematoma, wound infections, ischemia of flaps, fistulas or disruption of perineoplasty) and potentially failure of the repair we used, successfully, in both cases autologus Platelet Rich Plasma gel (PRP), recognized for its ability to promote wound healing and soft tissue sealing. Furthermore, PRP enhance the hemostatic response to injury and because of the high leukocyte concentration provides an antimicrobical effect [10]. Thus, once performing the plication of puborectalis muscle, the interposition of PRP gel fills dead spaces created by dissection and eliminates the possibility of fluid collections which may lead to failure. This consolidates the reconstruction of perineal body and supports the sphincteroplasty and we believe it is an important technical point in surgical treatment of traumatic cloaca.
In our experience, during the immediate postoperative period, there were no significant complications and after surgical followup of one month there was excellent healing of all wounds and after long-term follow-up of 6-12 months the patients reported fully recovered flatus and fecal continence, good cosmetic result and significant improvement in terms of psychological status and sexual activity.
In conclusion, surgical treatment of traumatic cloaca achieves good functional and aesthetic results, is safe and present low rates of complications [3,5,8]. The reconstruction of perineal body anatomy may be challenging and complicated. Therefore, consult a specialist colorectal surgeon familiar with the various surgical techniques can improve the long-term results and the quality of life of these patients [4-9].
References
- Corman ML (2005) Anal incontinence following obstetrical injury. Colon and Rectal surgery (5thedn).
- Venkatesh KS, Ramanujam P (1996) Surgical treatment of traumatic cloaca. Dis Colon Rectum 39: 811-816.
- Kaiser AM (2008) Cloaca-like deformity with fecal incontinence after after severe obstetric injury-technique and functional outcome of ano-vaginal and perinealre construction with X-flaps and sphincteroplasty.Colorectal Dis10: 827-832.
- Spanos CP, Mikos T, Kastanias E (2012) Surgical treatment of traumatic cloaca. Arch Gynecol Obstet 286: 815-818.
- Valente MA, Khanduja KS (2012) Layered surgical repair of traumatic cloacal deformities: technical details and functional outcomes. Tech Coloproctol 16: 153-156.
- Wexner SD,Marchetti F,Jagelman DG (1996) The role of sphincteroplasty for fecal inconti-nencere evaluated: prospective physiologic and functional review. Dis Colon Rectum 39: 1164-1170.
- Goldberg SM, Gordon PH, Nivatvongs S (1980) Essentials of anorectal surgery. J.B. Lippincott, Philadelphia.
- Malouf AJ,Norton CS,Engel AF, Nicholls RJ,Kamm MA(2000) “Long-term results of over lapping anterior analsphincter repair for obstetric trauma” Lancet 355:260-265.
- Abcarian H, Orsay CP, Pearl RK (1989) Traumatic cloaca. Dis Colon Rectum 32:783-787.
- Smith RG, Gassmann CJ, Campbell MS (2007) “Platelet-rich Plasma: Properties and Clinical Applications” The Journal of Lancaster General Hospital 2:73-78.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences