Treatment of the Aging Midface and Neck with a Mini Sub-SMAS Lift and Lower Blepharoplasty with Fat Repositioning and Orbitalis Oculi Muscle Suspension Under Local Anesthesia
Sonam Dodhia*, Rachel Weitzman and Oscar Trujillo
DOI10.36648/2472-1905.8.1.0147
Sonam Dodhia*, Rachel Weitzman, Oscar Trujillo
Department of Otolaryngology, Columbia University, New York Presbyterian Hospital, New York
- *Corresponding Author:
- Sonam Dodhia
Department of Plastic and Reconstructive Surgery, Cambridge University Hospitals NHS Foundation Trust, Cambridge, United Kingdom
E-mail:drondero@bronxleb.org
Received date: December 07, 2021, Manuscript No. IPARS-22-12409; Editor assigned date: December 09, 2021, PreQC No. IPARS-22-12409 (PQ); Reviewed date: December 23, 2021, QC No. IPARS-22-12409; Revised date: December 28, 2021, Manuscript No. IPARS-22-12409 (R); Published date: January 07, 2022, DOI: 10.36648/2472-1905.8.1.147
Citation: Oldas C (2022). Treatment of the Aging Midface and Neck with a Mini Sub-Smas Lift and Lower Blepharoplasty with Fat Repositioning and Orbitalis Oculi Muscle Suspension under Local Anesthesia. J Aesthet Reconstr Surg Vol.8 No.1:147.
Abstract
Introduction: Many facial plastic surgeries for the aging face may now be performed in-office, under local anesthesia and oral sedation. This is a result of innovation in surgical technique and rejuvenation technology, and in response to patient preferences for faster recovery times and lower costs. This paper presents a novel combination of in office techniques to address the midface and neck, two critical areas in the treatment of aging face.
Methods: We present an approach to restore a youthful face with a mini sub-SMAS lift, lower blepharoplasty with fat repositioning, and orbitalis oculi muscle/arcus marginalis release and suspension, all performed under local anesthesia and oral sedation with minimal post-operative downtime. Results: Our patient treated with this technique recovered well and had a favorable cosmetic outcome with zero complications and minimal downtime.
Conclusion: The mini sub-SMAS lift combined with lower blepharoplasty including orbital fat repositioning and orbicularis oculi muscle/arcus marginalis release and suspension performed under local anesthesia and oral sedation is a novel approach for restoring a youthful appearance to the face and neck. The patient avoids the risks associated with general anesthesia and benefits from a more affordable and convenient option for an elective cosmetic surgery with minimal post-operative downtime.
Introduction
The midface is a primary target for treatment of the aging face. Loss of tissue elasticity due to collagen breakdown, repetitive motion from muscle contraction, and the effects of gravity all contribute to soft tissue descent. In the upper midface, the descent of fat compartments over time results in decreased volume and narrowing of the upper midface, as well as increased volume and widening of the inferior midface peri-orally. These effects in combination result in a facial proportion that appears less healthy and less youthful [1].
In the infraorbital region, aging results in loss of tone and downward descent of the orbicularis oculi muscle, creating the appearance of a redundancy in an inferolateral vector, in other words, a lower lid "V" deformity [2]. Regarding the nasolabial region, Rohrich and Pessa demonstrated through cadaveric studies that augmentation of the deep medial cheek fat created an improved midface projection, effacement of the deepened nasolabial fold, and improvement in the lower lid "V" deformity. Deflation of the deep medial cheek fat, they posit, can create pseudoptosis of the overlying superficial fat and skin, and is therefore the cause of the characteristic midface changes in volume loss with aging [3].
A centrally visible part of aging thus occurs in the midface and periorbital area because of the combined effects of medial cheek fat descent, exposure of the orbital rim/deep nasojugal grooves, and excess pseudoherniation of orbital fat [4]. Treatments targeted to address these effects have evolved immensely in recent years [5].
Earlier techniques including the excision of redundant skin [6] and the repositioning of subcutaneous fat, fascia and muscles [7] later evolved to identify and incorporate the Superficial Musculoaponeurotic System (SMAS) [8] Skoog's work led to the development of the deep plane rhytidectomy to address the deepening nasolabial fold through the use of fat repositioning. From the deep plane rhytidectomy, Hamra developed the composite rhytidectomy by exposing the orbicularis oculi muscle [2]. The composite rhytidectomy aims to reposition the platysma muscle, cheek fat and orbicularis oculi muscle while retaining their normal anatomic relationships with one another. Hamra achieved this by undermining the orbicularis oculi muscle and employing a facelift dissection to create a bi-pedicled composite facelift flap, and then repositioning the flap with a superomedial vector for the orbicularis oculi muscle. The result is that the deep elements are effectively repositioned but still maintain normal anatomical relationships with one another other and with the skin.
With aging, skeletonization of the inferior orbital rim occurs as soft tissue descends, resulting in observable defects. The technique of mobilizing intraorbital fat to provide thicker coverage over the bony orbital rim was described by Loeb and Hamra [8,9]. Conventional lower lid blepharoplasty involves removal of the orbital fat which improves the lid contour for a number of years, but can be associated with the development of a "sunken" eye look over time [4]. The repositioning of orbital fat, with less removal, to efface a prominently visible inferior bony rim may offer better long-term success.
Facial plastic surgery procedures are exceedingly popular. According to the aesthetic plastic surgery national databank statistics for 2020, facelift was the most common surgical procedure in those ages 70 and over, and blepharoplasty was the third most commonly performed aesthetic surgical procedure in men. The total number of cosmetic surgeries in 2020 is 22% higher than that performed in 2000 [9]. This high demand, as well as patient preferences for faster recovery times and lower costs, has created an ideal environment for innovation in developing safe and effective in-office techniques.
General anesthesia presents risk, especially for the aging population that is likely to pursue elective facial plastic surgery procedures. Patients over the age of 60 have significantly more complications from general anesthesia than younger patients [2]. General anesthesia also substantially adds to the cost of an elective procedure. This suggests that in office procedures under local anesthesia and oral sedation, to the extent they can be performed safely and effectively, would be a viable if not preferred alternative. This is also true for those patients who have significant medical co-morbidities with increased risk of complications associated with general anesthesia. Only a limited number of studies have explored the safety and efficacy of in office local anesthesia and oral sedation facial plastic surgery procedures [6]. To our knowledge, no study has yet described the specific procedure of a mini sub-SMAS face and neck lift with submentoplasty (including liposuction and platysmaplasty) combined with lower blepharoplasty, including fat repositioning and orbitalis oculi muscle/arcus marginalis release and suspension, performed under local anesthesia and oral sedation.
Objective
We present an approach to address facial aging with a mini sub-SMAS face and neck lift with submentoplasty (including liposuction and platysmaplasty) combined with lower blepharoplasty including fat repositioning and orbitalis oculi muscle/arcus marginalis release and suspension performed under local anesthesia with minimal post-operative downtime.
Methods
Patient history
This patient is a 72-year-old woman with a history of hypertension who presents for possible facial rejuvenation with no previous facial plastic surgery. She states she does not like the bags under her eyes and feels that she looks tired all the time. She also does not like the sagging appearance of her neck and jawline due to aging.
On exam, she had excessive pseudoherniation of fat in lower lids with excess skin and upper lids without significant excess skin. She had an overall good midface and cheek bony structure, but moderate jowls with skin laxity along the jawline, and mild central submental fat, mild platysmal banding and moderate skin laxity. She expressed disinterest in general anesthesia for any procedure and a preference for a procedure that would give her as little "downtime" as possible. She also understood that the result may not be as grand as with a full face/neck lift but will still offer significant and natural improvement. Importantly, she was not an anxious patient at baseline and was alright with undergoing a procedure under local that may take up to 5 hours or 6 hours.
Therefore, the patient was offered the option of an in-office mini sub-SMAS face/neck lift with submentoplasty and plastymaplasty and lower blepharoplasty with fat repositioning to address the most significant facial aging concerns as expressed by the patient, without the need for general anesthesia.
Procedure preparation
Prior to the procedure, the patient was advised that the duration would be approximately 5 hours or 6 hours. For pain control and anxiolysis, she was given one tablet of Percocet 5 mg/325 mg and 2 mg of Ativan (equally divided and administered between the eyelid surgery and face/neck lift). For local anesthesia to numb the face and neck, a tumescent solution was created containing 50 cc of 1% lidocaine plain, 50 cc of 0.25% Bupivacaine plain, 50 cc of bacteriostatic 0.9% saline, and 1 cc of epinephrine 1:1000. A different local anesthetic tumescent solution was made for the eyelids from 10 cc of 1% lidocaine plain, 10 cc of 0.25% bupivacaine plain, and 0.2 cc of epinephrine 1:1000. Skin was prepped with betadine and she was draped in the standard sterile fashion. Patient was also given a capsule of Keflex 250 mg antibiotic one hour prior to start the procedure, which was continued four times a day for the subsequent week post-operatively.
Submentoplasty with central and jawline liposuction and platysmaplasty: A 2.5 cm incision was marked in the submental crease. A submental incision was made through the skin, and wide undermining was done with scissor dissection in the pre-platysmal plane. Redundant fat was removed with fenestrated and spatula microliposuction cannulas. The medial margins of the platysma were identified and the subplatysmal fat was injected with tumescent solution. Some was also removed with liposuction for an improve cervical-mental angle. The medial edges of the platysma muscle were then undermined with facelift scissor, 2 cm on both sides, lateral from the submental area to the hyoid bone. The platysmal muscle edges were then back-cut at the hyoid bone area and sewn together with buried, interrupted, alternating 3-0 PDS and 3-0 Prolene sutures. Hemostasis was obtained with bipolar cautery. At the conclusion of the case, hemostasis was confirmed and the skin incision was closed with 5-0 Prolene sutures.
Mini sub-SMAS face and neck lift: An incision was marked as extending inferiorly from 2 cm superior to superior aspect of the auricle within the temporal hair, curving posteriorly along the posterior aspect of the tragus, into the cheek-lobule crease, then curving posteriorly post-auricularly over the mastoid process, and continuing posterioinferiorly one to two rows of follicles into the posterior hairline, 1 cm-2 cm in vertical length. With a 15-blade scalpel, the facial incision was made and the subcutaneous dissection proceeded over the tragus, with care not to disrupt the tragal perichondrium. The superficial aspect of the SMAS was identified and dissection proceeded anteriorly to a vertical line at the level of the angle of the mandible for a short, skin-only flap. The skin-only flap was continued inferiorly into the neck two fingerbreadths below the mandible and then posteriorly to the posterior hairline. Tumescent solution was injected into the sub-SMAS plane prior to beginning the dissection.
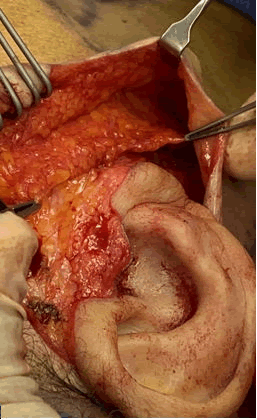
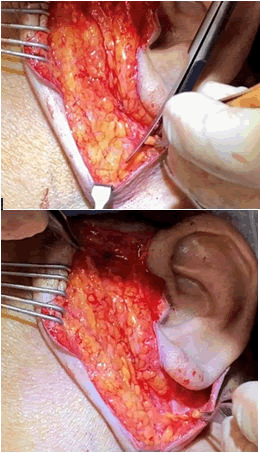
To enter the sub-SMAS plane, an incision was made through the SMAS starting approximately 2 cm anterior to the tragus over the parotid gland, with care to leave behind adequate SMAS to which to suture later in the procedure. The sub-SMAS plane was dissected anteriorly to the edge of the parotid gland and ensuring the parotidomasseteric fascia was left undisturbed, as seen in (Figure 1). This dissection was carried superior to the zygomatic area and inferiorly into the neck in a sub-platysmal plane two fingerbreadths below the mandible.
In the neck, the sub-platysmal dissection was entered from behind the angle of the mandible, under the ear anteriorly, 3 cm past the angle of the mandible, with care not to injure the marginal mandibular branch of the facial nerve. A myotomy of 2 cm was performed at the level of the inferior border of the mandible, to allow a mobilized SMAS-platysmal flap to be pulled in two different vectors of advancement to achieve the desired aesthetic result, as seen in (Figure 2).
The superior aspect of the SMAS flap was cut horizontally at the level of the zygoma to allow for superior vector of advancement. Therefore, the superior (face) flap was pulled superior first, and a SMASectomy was performed to trim the excess SMAS prior to anchoring it in superior direction to the undissected SMAS near the zygoma with a 3-0 Prolene suture in a horizontal mattress fashion. The remaining portions of the superior (face) flap were pulled in a posterior-superior vector and the excess SMAS was trimmed prior to anchoring the SMAS flap to the undissected SMAS over the parotid at various points using 3-0 Prolene suture in horizontal mattress fashion. Then, the inferior (neck) flap was pulled more posteriorly-horizontally and anchored to the mastoid periosteum using two 3-0 Prolene suture in horizontal mattress fashion. A clamp was used to hold the knot during maximal advancement while suturing to achieve the maximum pull/suspension of the platysmal muscle in the neck.
Once the SMAS-playstmal flaps were mobilized and suspended, the excess in the skin-only flap was trimmed to allow for a tension-free closure. To further relieve tension on the skin closure, the skin flap was also suspended in 4 locations (near the hair tuft, under the lobule, at the post-auricular area, and at the posterior hairline) with taching sutures using 5-0 Vicyl. The skin was then closed with running 5-0 Prolene sutures. No drains were used. A pressure dressing was placed after all fluid from the flaps was evacuated at the end of the surgery.
Lower blepharoplasty with fat repositioning and orbitalis oculi muscle suspension: An incision was marked 2 mm-3 mm inferior to the ciliary margin in the first natural eyelid crease and extended from just prior to the medial punctum of the lower eyelid horizontally, following the natural curvature of the eyelid, to about 1 cm lateral to the lateral canthus were it was extended in an inferior direction at the level of the lateral canthus. The lower eyelid was injected with a local anesthetic. A pinch excision of the skin was performed (to create a standing ridge of skin with Adson-Brown forceps). Lateral to the lateral canthus, the incision was made with a 15-blade scalpel and the orbicularis muscle was dissected through with Bovie cautery.
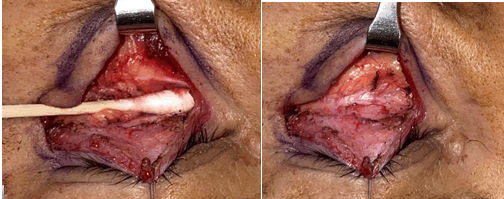
Once dissected through laterally, the muscle was carefully elevated off the orbital septum with a curved, blunt Metzenbaum scissor along an avascular plane. Then, using blunt dissection with a freer and q-tips, the orbital septum was fully released from the orbicularis oculi muscle. Next, a stair-stepped incision was made with needlepoint Bovie cautery, leaving intact a 4 mm-5 mm sling of orbicularis oculi muscle around the tarsal plate in order to maintain eyelid tone.
Once dissected through the muscle in a horizontal linear fashion, the eyelid was retracted superiorly with a 6-0 Prolene suture and a clamp on the head drape to close/protect the eye/cornea. A freer was then used to release the orbicularis oculi muscle/arcus marginalis from the orbital rim at least 1 cm below the orbital rim, as seen in Figure 3. Once released, the septum was incised and with gentle manipulation with q-tips, the orbital fat was released from the septum, ready to be mobilized to over the orbital rim (Figure 3). It is very important to fully release the orbital fat so that during the post-op healing period it does not tether the orbital septum or tarsal plate, thereby avoiding complications such as ectropion.
The orbital fat was then sewn to the periosteum along the inferior orbital rim with several 6-0 Prolene sutures, thereby covering the orbital rim and adding volume/fat to the upper cheek/infraorbital area. Figure 3 shows the orbital rim exposure with a q-tip. Figure 3 shows the orbital fat release from the septum to be sewn tension-free to cover the orbital rim and improve the nasojugal groove.
Using a 5-0 Prolene suture in a horizontal mattress fashion, the lateral aspect of the orbicularis oculi muscle was suspended to the periosteum of the lateral bony orbital rim, just above the level of the lateral canthus. At this point, a skin-only flap is elevated laterally, only to conservatively remove the excess lateral lower eyelid skin that was advanced with suspension of the orbicularis oculi muscle. The lower blepharoplasty incision was then closed with a running 6-0 Prolene suture under the eyelid with one end left untied and steri-stripped to the glabella area for swelling. The incision lateral to the lateral canthus was closed with simple, interrupted 6-0 Prolene sutures.
Total operative time for the procedure was five hours with the mini-SMAS face/neck lift requiring three hours and the eyelid surgery two hours to complete. The patient was given 1 mg of Ativan at the start of the case and 1 mg after the face/neck lift prior to starting the eyelid surgery. She also fell asleep during the face/neck lift and part of the eyelid surgery and tolerated the procedure well with no complications. She was then picked up by her escort and went home from the office.
Results
The patient described above had an uneventful post-operative course and was seen on post-op day 1 to remove the pressure dressing, and then again on post-op day 7 for suture removal. The patient was asked to always wear the submental soft pressure band during the first week and then only at night for the following 2 weeks to allow for even distribution of the submental skin after the submentoplasty portion of the procedure. Figure 4 shows the patient's pre-operative and post-operative day 14 photos to illustrate the clear improvement in signs of facial aging with minimal bruising and swelling. Figure 5 shows the pre-operative and 3 month post-operative photos to demonstrate the improvement in the midface and eyelid-cheek junction, as well as improvement in the jawline and neck (Figures 4 and 5).
Discussion
We have presented an approach to address the midface/eyelid-cheek junction and jawline/neck aging with a mini sub-SMAS face and neck lift, submentoplasty (with liposuction and platysmaplasty), lower blepharoplasty with fat repositioning, orbitalis oculi muscle/arcus marginalis release and suspension, all performed in-office under local anesthesia and oral sedation. To our knowledge, this approach to facial aging has not been described elsewhere in the literature.
Facial plastic surgery procedures improve patients' quality of life. In fact, rhytidectomy was shown to result in patient satisfaction via a statistically significant improvement in FACE-Q score [7]. Not with standing, facial plastic surgery procedures are expensive and generally not covered by insurance. The average surgeon fees for blepharoplasty are over $3000, facelift over $8000, brow lift over $3500, chin augmentation over $2000, and cheek implants over $3000 [9]. Innovation in developing in-office techniques for facial rejuvenation under local anesthesia, like those described in this paper, has the strong potential to make these procedures more affordable and therefore more available for patients without sacrificing safety or efficacy.
Conclusion
This approach is unique and presents a strong value proposition for several reasons. First, this approach is effective in restoring a youthful appearance and addressing key signs of facial aging in the following areas: Periorbital, upper midface, jawline and neck. Second, that this approach is safely performed in-office under local anesthesia and oral sedation obviates the added costs and associated risks of general anesthesia. Finally, it is unique in that patients require minimal downtime to recover from the procedure. In the present case study, the patient was already back to work on post-operative day 14.
The nature of the short skin flap employed in this procedure supports it as a preferred option for older patients with co-morbidities such as diabetes mellitus and hypertension, or those or simply do not want general anesthesia. The short skin flap also decreases substantially the recovery time for the patient, with the slightly more extensive sub-SMAS flap causing little visible swelling or bruising in the two-week post-operative period. It is important to inform patients preoperatively that this technique is not meant to replace the cosmetic result that a full deep plane face/neck lift with dissection to the midface offers. However, it does give significant improvement in the midface/upper cheek, jawline and neck without the need for extended downtime, general anesthesia, or high cost.
Authorship Confirmation Statement
All authors have participated in the study to a significant extent. All authors have read and agreed to the submitted version of the paper and bear responsibility for it.
Disclosures
All authors have no disclosures to report.
References
- Alghoul M, Codner MA (2013) Retaining ligaments of the face review of anatomy and clinical applications. Aesthetic Surg J 33: 769-782.
[Crossref], [Google Scholar], [Indexed]
- Hamra ST (1992) Composite rhytidectomy. Plast Reconstr Surg 90: 1-13.
[Crossref], [Google Scholar], [Indexed]
- Rohrich RJ, Pessa JE, Ristow B (2008) The youthful cheek and the deep medial fat compartment. Plast Reconstr Surg 121: 2107-2112.
[Crossref], [Google Scholar], [Indexed]
- Kamer FM, Mingrone MD (2005) Deep plane rhytidectomy: A personal evolution. Facial Plast Surg Clin North Am 13: 115-126.
[Crossref], [Google Scholar], [Indexed]
- Mitz V, Peyronie M (1976) The Superficial Musculo-Aponeurotic System (SMAS) in the parotid and cheek area. Plast Reconstr Surg 58: 80-88.
[Crossref], [Google Scholar], [Indexed]
- Hamra ST (1992) Repositioning the orbicularis oculi muscle in the composite rhytidectomy. Plast Reconstr Surg 90: 14-22.
[Crossref], [Google Scholar], [Indexed]
- Baker SR (1999) Orbital fat preservation in lower-lid blepharoplasty. Arch Facial Plast Surg 1: 33-37
[Crossref], [Google Scholar], [Indexed]
- Frojo G, Dotson A, Christopher K, Kaswan S, Lund H (2019) Facelift performed safely with local anesthesia and oral sedation: Analysis of 174 patients. Aesthetic Surg J 39: 463-469.
[Crossref], [Google Scholar], [Indexed]
- Berger M, Weigert R, Pascal E, Hufschmidt K, Casoli V (2019) Assessing improvement of patient satisfaction following facelift surgery using the FACE-Q scales: A prospective and multicenter study. Aesthetic Plast Surg 43: 370-375.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences