Use of Adipofascial Superficial Circumflex Iliac Artery Perforator Flap in Amniotic Band Syndrome to Improve Contour Following Amniotic Band Resection in the Upper Extremity: A Report of Two Cases
Gonzalo Mallarino1*, José Rodrigo Foti-Barreto1, Carlos David Gutierrez2 and Camilo Romero-Barreto3
1Department of Head & Neck Oncologic and Reconstructive Surgery, Centro Policlinico el Olaya, Bogotá, Colombia
2Department of Plastic and Reconstructive Surgery, Hospital Militar Central, Bogotá, Colombia
3Department of Hand and Reconstructive Microsurgery, Instituto Roosevelt, Colombia
- *Corresponding Author:
- Dr. Gonzalo Mallarino
Plastic Surgeon, Microsurgeon
Carrera 20 # 23-23 Sur Centro Policlínico del Olaya
Bogotá, Colombia
E-mail: gonzalo_mallarino@hotmail.com
Received Date: July 06, 2021; Accepted Date: July 30, 2021; Published Date: August 07, 2021
Citation: Mallarino G, Foti-Barreto JR, Gutierrez CD, Romero-Barreto C (2021) Use of Adipofascial Superficial Circumflex Iliac Artery Perforator Flap in Amniotic Band Syndrome to Improve Contour Following Amniotic Band Resection in the Upper Extremity: A Report of Two Cases. J Aesthet Reconstr Surg Vol.7 No.5:36.
Abstract
Amniotic Band Syndrome is a congenital disease that causes a variable degree of deformity and tissue disruption. The present study aims to show the use of adipofascial Superficial Circumflex Iliac Artery perforator (SCIP) flap to improve contour following amniotic band resection in the upper extremity of two cases of Amniotic Band Syndrome. Surgical excision of fibrotic tissue and advancement of local flaps is the gold standard for bands constricting the upper limb, proximal to the wrist. This case report exhibit a refinement technique additional to band exeresis using SCIP flaps in order to improve long-term extremity contour in Amniotic Band Syndrome. SCIP flaps surgical technique and three-year follow up of two patients who underwent the procedure are discussed.
Keywords
Amniotic Band Syndrome [MeSH]; Congenital; Perforators; Scip flap
Introduction
Amniotic Band Syndrome (ABS) constitutes a rare congenital disease, affecting 1 out of 15.000 live births [1]. Depending on the severity and affected structures by tissue disruption, ABS in the upper extremity can derive diverse clinical presentations including mild and incomplete forms to more severe types that represent a threat to limb viability requiring urgent surgical intervention [2].
Surgical excision of fibrotic bands and reconstruction with local flap advancement represents the current ex-utero treatment for ABS affecting the upper extremity. The techniques for local tissue arrangement have evolved over time from direct closure, to adipofascial flap advancement and w-plasty skin closure which has led to considerable improvements in extremity appearance and contour [3]. However, in some patients, a local tissue rearrangement might result insufficient to provide enough volume for obtaininig an optimal contour [4]. We aim to report our experience treating moderate complete upper extremity ABS with band resection, adding an adipofascial free flap to improve long-term contour in two pediatric patients.
Case Presentation
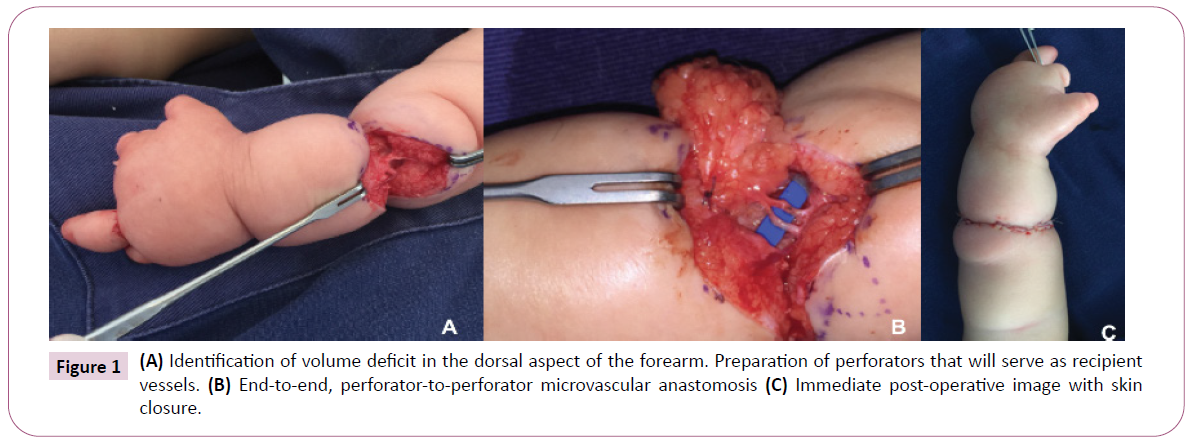
The patients are induced under general anesthesia. After fibrotic tissue resection, local fasciocutaneous and skin flaps are advanced to identify areas lacking volume (Figure 1A). Once the approximate amount of missing tissue is estimated, SCIP from the donor area are identified using a hand-held doppler. SCIP flap is marked in a standardized way [5]. Groin superficial fascia is exposed by elevation of skin flaps and subsequently harvested based on the larger perforator found. Adjacent perforators from the recipient side (usually arising from the Radial Artery) are dissected and the donor’s vessels are ligated. An end-to-end, perforator-to-perforator microvascular anastomosis is carried out (Figure 1B). The flap is fixated in order to address volume deficiency with absorbable sutures, and when its viability is ascertained, skin closure is conducted using a regular w-plasty pattern (Figure 1C). No skin paddle is used, and flap viability is closely monitored using Doppler ultrasound. Usually, the patient discharge occurs after 24 hours of monitoring when there are no complications.
Case 1
A 1-year-old male with no other relevant familiar or personal history presented with complete moderate ABS in the left upper extremity. Examination revealed multiple digit amputation and a more proximal circumferential band at the middle third of the forearm causing limb deformity (Figure 2A). Resection and reconstruction of amniotic bands were performed. After complete excision of fibrotic tissue and initial advancement of local adipofascial flaps, a dorsal depression was evidenced. A 5 × 3 cm adipofascial flap was harvested and fixed in the dorsal aspect of the forearm where soft tissue deficiency was initially noted. Cutaneous closure was conducted with a w-plasty design. Immediate postoperative went by uneventfully. Three years later during follow-up, an adequate contour of the limb was observed with no donor-site morbidity (Figure 2B).
Case 2
A 3-year-old female presented with complete moderate ABS in the left upper extremity. During the physical examination, proximal third constriction due to amniotic bands in the forearm was appreciated. The reconstructive procedure was performed as previously described. Flap monitoring was conducted with a hand-held doppler during the following 24 hours and the patient was discharged. During three year follow-up a harmonic contour was observed with no flap bulkiness, and no donor site complications.
Discussion
Amniotic Band Syndrome is a broad group of congenital anomalies that can affect multiple parts of the foetus [1]. Extremity ABS can be further classified in mild, when the compromised limb has an incomplete or superficial band with no distal constriction, moderate when it has a circumferential configuration and spares deeper structures, and severe when constriction threatens member viability due to compromise of its main vessels [4].
Surgical excision and reconstruction with local flaps remains the gold standard for the ex-utero treatment of ABS. Even though ABS has a predilection for the digits, proximal compromise in the arm or forearm might be seen [6]. Simple excision with local flap comes across as a simple procedure that improves the limb appearance and allows better lymphatic drainage, improving limb contour; however, long term outcomes might result in a suboptimal appearance due to scarring of local tissue, especially in the paediatric population where higher fat deposits in the extremities are observed (Figure 2C). Adding vascularized tissue by the means of free flaps is an innovative refining technique that surgeons can use to improve contour in patients suffering from ABS that undergo surgical resection. From what we presented above, long-term follow-up in one of the patients showed that flap bulkiness was not an issue as extremities becomes leaner during growth, nevertheless, this might not be the case in patients presenting at a later age with less volume of subcutaneous tissue. A perforator-to-perforator microvascular anastomosis allows for the main vascular axis of the upper extremity to be spared, which makes both the donor and the recipient site morbidity of this technique almost absent, except for a conspicuous scar in the groin area.
Conclusion
The use of adipofascial SCIP flap is an alternative to the widely used gold standard, for the treatment of ABS. We treated two patients with SCIP flap, both presented excellent results in the long-term follow-up. SCIP flap is being used to treat other pathologies. This is the first report of SCIP flap being used for ABS treatment showing a significant improvement in the contour of the extremities in both cases.
Even though the procedure described in the present study might come across as an intricate solution to a problem that has already a simple solution, authors firmly believe that as microsurgical techniques become available, reconstructive surgeons should be willing to go the extra mile, and make an effort to access their creativity in order to rethink and improve existing procedures with the purpose of delivering better outcomes to their patients.
Consent Statement
The authors have obtained the prior informed consent from parents of the two newborns for developing and publishing this manuscript. Considering age of the participants they weren’t able to give assent.
Conflict of Interest
No conflict of interest has been declared by the authors.
Ethical Standards
This manuscript was approved by the ethics committee of the Roosevelt Institute, Bogotá, Colombia.
References
- Koskimies E, Syvänen J, Nietosvaara Y, Mäkitie O, Pakkasjärvi N (2015) Congenital constriction band syndrome with limb defects. J Pediatr Orthop 35: 100-103.
- Kawamura K, Chung KC (2009) Constriction band syndrome. Hand Clin 25: 257-264.
- Mutaf M, Sunay M (2006) A new technique for correction of congenital constriction rings. Ann Plast Surg 57: 646-652.
- Chung KC, Kim SE (2008) Operative technique; hand and wrist surgery. 2nd edn. Philadelphia: Saunders Elsevier p. 837-846.
- Suh HSP, Jeong HH, Choi DH, Hong JPJP (2017) Study of the Medial Superficial Perforator of the Superficial Circumflex Iliac Artery Perforator Flap Using Computed Tomographic Angiography and Surgical Anatomy in 142 Patients. Plast Reconstr Surg 139: 738-748.
- Moran SL, Jensen M, Bravo C (2007) Amniotic band syndrome of the upper extremity: diagnosis and management. J Am Acad Orthop Surg 15: 397-407.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences