Venous Congestion Resolution in DIEP Flaps with Pedicle Division and Use of Cephalic Vein, Report of 2 Cases
Plastic and Reconstructive Surgery Division, Sanitas University Foundation Bogotá, Colombia
- *Corresponding Author:
- Dr. Camilo Mejia
Plastic and Reconstructive Surgery Division
Sanitas University Foundation Bogotá, Colombia
E-mail: mejiacami@gmail.com
Received Date: September 02, 2021; Accepted Date: October 05, 2021; Published Date: October 12, 2021
Citation: Sanchez M, Mejia C, Ramirez D (2021) Venous Congestion Resolution in DIEP Flaps with Pedicle Division and Use of Cephalic Vein, Report of 2 Cases. J Aesthet Reconstr Surg Vol.7 No.7:43.
Abstract
Background: Autologous Deep Inferior Epigastric Perforator (DIEP) breast reconstruction is a widely used method. Venous congestion is one of the most commonly reported complications. Our objective is to describe and analyze strategies for the therapeutic approach in situations of venous congestion in DIEP flaps.
Methods: We describe the surgical technique of two DIEP flap breast reconstruction cases in which venous congestion was presented as a late complication. Division pedicle strategy and use of cephalic vein as a receptor site for venous drainage are analyzed. Besides we propose a therapeutic approach algorithm.
Results: We found out that division pedicle strategy and use of cephalic vein is an excellent option for venous drainage in DIEP flaps when venous congestion occurs. This vessel allows easy dissection, has a suitable caliber and has a wide length to choose the appropriate anastomosis site.
Conclusion: Division pedicle and use of cephalic vein as a site receptor in cases of venous congestion in DIEP flaps allows adequate venous drainage and may be an option to resolve this complication.
Keywords
DIEP flap; TRAM flap; Division pedicle; Cephalic vein; Venous congestion
Introduction
Deep inferior epigastric perforator artery (DIEP) flap breast reconstruction has become one of the methods of choice since its introduction in 1989 by Koshima and Soeda [1]. Compared to breast reconstruction with transverse rectus abdominis muscle (TRAM) flap, advantages of DIEP flaps are multiple, they include reduction in hospitalization times, less postoperative pain, earlier recovery, less hernias development and preservation of abdominal strength [2,3]. Complications of TRAM vs. DIEP flaps have been compared, finding a higher risk infection (8.8% vs. 3.6%) delayed wound healing (17.9% vs. 6.0%) and presence of seroma (8.8% vs. 3.6%, respectively). Vascular complications represent the main risk of failure of breast reconstruction in the DIEP flaps. The most reported complication is venous congestion, reported on the literature to occur in 5% of DIEP flaps but it varies, ranging from 2% to 8% [4-6]. Venous congestion clinical manifestations are changes in flap color, from pink to purple, quick capillary filling and turgor of superficial veins as signs of hyperemia [7].
In a review with data from 17,096 DIEP flaps [8], 2 cases of flap loss were reported, of which 40.3% were due to venous causes and 28.4% corresponded to causes related to arterial problems [9,10]. Torsion of the vascular pedicle, occlusion of microsurgical anastomosis or a disruption in venous drainage are common causes of venous congestion [11,12]. For correcting this problem, several techniques have been described to supplement venous outflow in attempt of salvaging a congested flap [13,14]. Proposals for treatment algorithms have been published as an important tool to use in this situation. Pignatti and collaborators carried out a systematic review in June 2019 and in April 2020 they found that the majority of articles favor the use of the superficial inferior epigastric vein (SIEV) as an alternative for flap decongestion [15]. On the other hand, Bartlett et al. proposed an algorithm for venous congestion produced by DIEP flap, taking 813 flaps of which 4.8% presented this complication [11].
SIEV has been used as an alternate drainage method in cases of DIEP flap decongestion, this vein can be ipsilaterally anastomosed to the external jugular vein [13], basilic vein [16] Cephalic Vein (CV) [17] thoracodorsal vein, lateral thoracic or an intercostal vein [4]. Present study describes the profit of pedicle division and the use of CV in cases of venous congestion. Therefore, our objective is to describe and analyze strategies for the therapeutic approach in these situations.
Methodology
A literature search was performed with Mesh terms (DIEP flap) OR (deep inferior epigastric perforator) OR (DIEP) AND (hyperemia) OR (congestion venous) AND (cephalic vein) AND (pedicle division) during January 2020. Emphasis is placed on searching for articles that propose pedicle division and the use of CV as a venous drainage system in cases of venous congestion in DIEP flaps and the formulation of treatment algorithms as a tool to solve this complication. Two case reports are presented and we describe the surgical technique used as an alternative in cases of venous congestion in breast reconstruction with a DIEP flap. Additionally, a treatment algorithm is presented for making decision in cases of venous congestion in DIEP flaps.
Case Description
Case 1: A 49-year-old, nonsmoking woman, mastectomized, obese patient
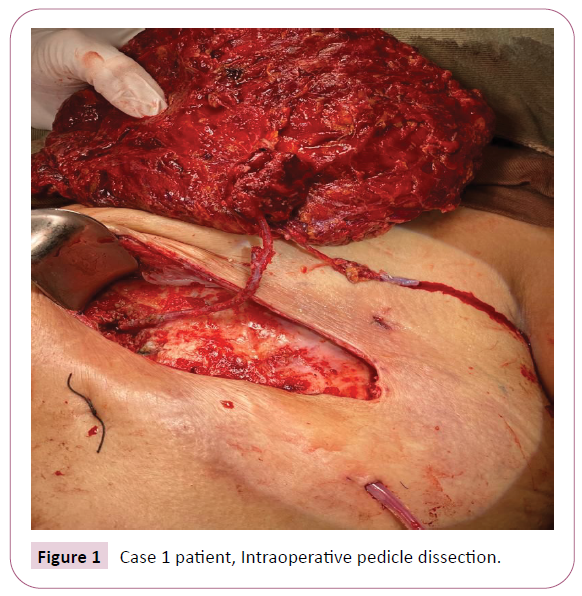
Perforant arteries identification was performed by doppler and Computed Tomography Angiography (CTA), pedicle dissection was completed, obtaining vessels of deep system and superficial system, DIEP and SIEV (Figure 1). We perform venous anastomosis to internal mammary vein and arterial anastomosis to internal mammary artery by microsurgical technique. Intraoperatively, congestion flap is evidenced with changes in flap color, from pink to purple and sings of local inflammation (Figure 2), thus we decided to repeat venous anastomoses without achieving adequate drainage. We identified the cause of this condition, related to the caliber of internal mammary vessels, which were too small for inferior epigastric vessels. Therefore, an attempt was made to correct the venous congestion by connecting the SIEV to internal mammary vein, however, venous congestion continued. Finally, an attempt was made to take CV as a recipient vessel to the DIEV and division pedicle was performed, achieving venous congestion resolution and the rescue of the flap.
Case 2: In a 55-year-old nonsmoking woman
In a 55-year-old nonsmoking woman, we performed the same dissection steps as the previous case, with flap correctly advanced and without signs of intraoperatively detected venous congestion. The patient was discharged from the hospital and on the sixth day she presented signs of venous congestion, with presence of an intra-flap hematoma with signs of local inflammation. A new intervention is performed and the flap is dissected again, the hematoma is cleaned and drained, we noticed that venous congestion was due to thrombosis of internal mammary vein and the deep system secondary to hematoma. A new anastomosis was tried using SIEV, however, due to persistence of venous congestion, we decided to use the cephalic vein and perform pedicle division to correct the problem and save the flap (Figure 3).
Results
The total surgery time was 7 hours and 30 minutes for the first case. In second case, two surgical times were performed each with 6 and 3 hours respectively. In the follow-up at 2 months after the surgical procedure, an adequate adaptation of the flap was identified without new signs of venous congestion, both cases.
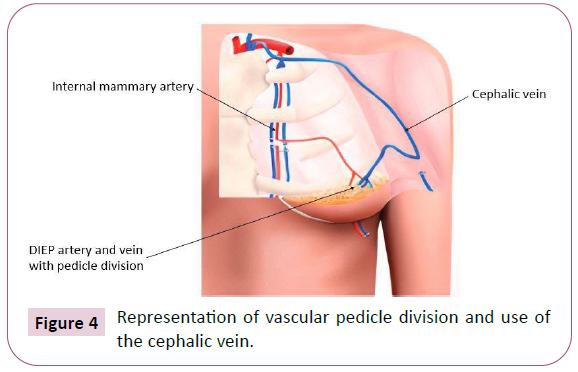
The follow-up at 5 months for both cases has shown no signs of venous congestion or other complications (Figure 4).
Discussion
In our experience, pedicle division and use of CV is a useful alternative to correct cases of venous congestion in DIEP flaps, since it allows easy dissection and due to its length, a suitable gauge can be selected for the recipient vessel. The use of CV as an alternative drainage method was shown to decrease the incidence of venous congestion in a series of 564 DIEP flap breast reconstructions, in which the reconstruction of 273 DIEP flaps was com-pared in which a single vein was used (7 of these flaps had venous congestion) with 291 DIEP flaps in which an alternative vein anastomosed to SIEV was used, the cephalic vein was used as the best recipient vein. Of these breast reconstructions, none had venous congestion [17]. In our experience with 413 DIEP flaps during the last five years, 4.8% had venous congestion. In relation to the cases mentioned above, in which we used CV as an alternative for venous drainage, the flap was salvaged. Limitations of this work are related to lack of evidence of use CV and pedicle division in cases of venous complication in DIEP flaps. Upper limb lymphedema using this technique has been described as a common complication [4,17]. However, this complication did not occur in any of the previously described cases. Intraflap methods de-scribed use microvascular mechanical suture with the Coupler® device, this technique can be a great solution to correct cases of venous complication, and however, only some countries in Latin America have the possibility of using this technology [18].
Therefore, strategies using CV for cases of venous congestion is a good option in countries such as Colombia where this technology is not available.
Conclusion
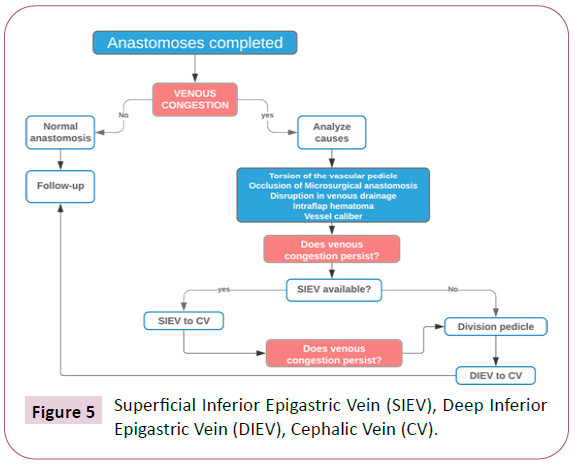
Venous congestion represents a significant obstacle for successful breast re- construction with the DIEP flap. Here, we present based on our experience, that pedicle division and use of the cephalic vein as a recipient vein demonstrated adequate venous drainage and salvage of the flap in 2 cases of venous congestion in breast reconstruction with DIEP flaps. However, subsequent comparative studies must be carried out due to the lack of evidence of use of this technique (Figure 5).
Algorithm
We propose the following algorithm as a strategy to save the flap in breast reconstruction with DIEP flaps. After completing anastomoses, DIEP vessels attached to internal mammary vessels, and then we check for flap congestion sings. If there is presence of venous congestion, we analyze the possible causes that can produce the congestion and, if possible, we solve them. If venous congestion flap still persists, we try to dissect the SIEV and anastomose it to cephalic vein. If congestion persists, we use DIEV and divide the pedicle to anastomoses to the CV. With this alternative, venous congestion is solved and the patient is followed for a period of 6 months.
References
- Koshima I, Soeda S (1989) Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg 42: 645-648.
- Futter CM, Webster MH, Hagen S, Mitchell SL (2000) A retrospective comparison of abdominal muscle strength following breast reconstruction with a free TRAM or DIEP flap. Br J Plast Surg 53: 578-583.
- Gill PS, Hunt JP, Guerra AB, Dellacroce FJ, Sullivaet SK, et al. (2004) A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg 113: 1153-1160.
- Wechselberger G, Schoeller T, Bauer T, Ninkovic M, Otto A, et al. (2001) Venous super drainage in deep inferior epigastric perforator flap breast reconstruction. Plast Reconstr Surg 108:162-166.
- Blondeel PN, Arnstein M, Verstraete K, Depuydt K, Van Landuyt KH, et al. (2000) Venous congestion and blood flow in free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps. Plast Reconstr Surg 106: 1295-1299.
- Schaverien MV, Ludman CN, Neil-Dwyer J, Perks AGB, Raurell A, et al. (2010) Relationship between venous congestion and intraflap venous anatomy in DIEP flaps using contrast-enhanced magnetic resonance angiography. Plast Reconstr Surg 126: 385-339.
- Galanis C, Nguyen P, Koh J, Roostaeian J, Festekjian J, et al. (2014) Microvascular lifeboats: A stepwise approach to in- traoperative venous congestion in DIEP flap breast reconstruction. Plast Reconstr Surg 134: 20-27.
- Gill PS, Hunt JP, Guerra AB, Dellacroce FJ, Sullivan SK, et al. (2004) A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg 113: 1153-1160.
- Knox ADC, HO AL, Leung L, Tashakkor YA, Lennox PA, et al. (2016) Comparison of outcomes following autologous breast reconstruction using the DIEP and pedicled TRAM flaps: A 12-year clinical retro- spective study and literature review. Plast Reconstr Surg 138: 16-28.
- Lie KH, Barker AS, Ashton MW (2013) A classification system for partial and complete DIEP flap necrosis based on a review of 17,096 DIEP flaps in 693 articles including analysis of 152 total flap failures. Plast Reconstr Surg 132: 1401‑1408.
- Bartlett E, Zavlin D, Menn Z, Spiegel A (2018) Algorithmic approach for intraoperative salvage of venous congestion in DIEP flaps. J Reconstr Microsurg 34: 404-412.
- Tran NV, Buchel EW, Convery PA (2007) Microvascular complications of DIEP flaps. Plast Reconstr Surg 119: 1397-1405.
- Mehrara BJ, Santoro T, Smith A, Arcilla ea, Watson JP, et al. (2003) Alternative venous outflow vessels in microvascular breast reconstruction. Plast Reconstr Surg 112: 448-455.
- Ali R, Bernier C, Lin YT, Ching WC, Rodriguez UP, et al. (2010) Surgical strategies to salvage the venous com- promised deep inferior epigastric perforator flap. Ann Plast Surg 65: 398.
- Pignatti M, Pinto V, Giorgini FA, Miralles MEL, D'Arpa S, et al. (2020) Different hydraulic constructs to optimize the venous drainage of diep flaps in breast reconstruction: Decisional algorithm and re- view of the literature. J Reconstr Microsurg 37: 216-226.
- Guzzetti T, Thione A (2008) The basilic vein: An alternative drainage of DIEP flap in severe venous congestion. Microsurgery 28: 555-558.
- Enajat M, Rozen WM, Whitaker IS, Smit JM, Acostaet R, et al. (2010) A single center comparison of one versus two venous anastomoses in 564 consecutive DIEP flaps: investigating the effect on venous congestion and flap survival. Microsurgery 30: 185-191.
- Andrades P, Maria ECG, Stefan DE, Cristian EC, Susana BC, et al. (2014) Microanastomosis venosa mecánica coupler®: Un importante aporte tecnológico a la microcirugía vascular. Revista chilena de ciru- gía 66.1: 52-58.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences