Vertical Improvement SMAS Suspension (VIPS) Facelift: Combining SMAS Plication and Retaining Ligament Preservation for Optimal Long-Term Results
Antonio Distefano1, Andrea Dotto2*, Ugo Catrambone3, Adriana Panayi4, Samuel Knoedler5, Leonard Knoedler6, Michael Alfertshofer7 and Giuseppe Colombo8
1Department of Plastic surgeon, Rigenera Clinic, Milan, Italy
2Department of Maxillofacial Surgery, Private Practice, Milan, Italy
3Department of Surgery, Thyroid Centre, Milan, Italy
4Department of Hand, Plastic and Reconstructive Surgery, Microsurgery, University of Heidelberg, Ludwigshafen, Germany
5Department of Plastic and Hand Surgery, Technical University of Munich, Munich, Germany
6Department of Oral and Maxillofacial Surgery, University Hospital in Berlin, Berlin, Germany
7Department of Oral and Maxillofacial Surgery, Ludwig Maximilians University Munich, Munich, Germany
8Department of Plastic and Aesthetic Surgery, Sant’Anna Clinic, Lugano, Switzerland
- *Corresponding Author:
- Andrea Dotto
Department of Maxillofacial Surgery, Private Practice, Milan, Italy
E-mail: info@andreadotto.it
Received date: February 27, 2025, Manuscript No. IPARS-25-20298; Editor assigned date: March 01, 2025, PreQC No. IPARS-25-20298 (PQ); Reviewed date: March 14, 2025, QC No. IPARS-25-20298; Revised date: March 21, 2025, Manuscript No. IPARS-25-20298 (R); Published date: March 28, 2025, DOI: 10.36648/2472-1905.11.1.90
Citation: Distefano A, Dotto A, Catrambone U, Panayi A, Colombo G, et al. (2025) Vertical Improvement SMAS Suspension (VIPS) Facelift: Combining SMAS Plication and Retaining Ligament Preservation for Optimal Long-Term Results. J Aesthet Reconstr Surg Vol.11 No.1: 090.
Abstract
Background: Facelift surgery, or rhytidectomy, aims to provide a rejuvenated appearance by addressing sagging skin, deep creases, and loss of muscle tone in the face and neck. The herein proposed technique combines both plications of the superficial musculo-aponeurotic system (SMAS) and the platysm, as well as preservation of integral retaining ligaments of the face to allow for optimal results in facial rejuvenation.
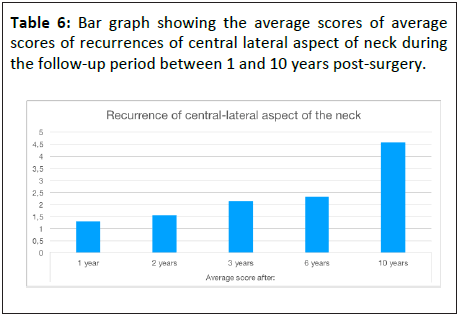
Methods: A retrospective study was performed on n=209 cases undergoing our novel facelift procedure. During the follow-up period with an average of 3.5 years [range: 1-10] post-operatively, we evaluated the recurrences of nasolabial fold, jowls, marionette lines, and the centrallateral aspect of the neck.
Results: Significant improvements were reported in jawline contour, nasolabial folds, marionette lines, and neck appearance, with the most stable results observed in the jawline area. Over the 10-year follow-up, a slight decline in these results was noted, but overall patient satisfaction remained high.
Conclusions: The novel face-lifting technique combines the plications of the SMAS and platysm with the preservation of retaining ligaments, offering a new surgical approach for facelift surgery. This approach provides reliable long-term results comparable to more invasive methods, yet with a lower risk of postoperative complications. Future studies are warranted to determine long-term outcomes in a multicenter and multi-surgeon setting.
Keywords
Rhytidectomy; SMAS; Platysma plications; Facial retaining ligaments; Facelift; Facial aesthetic surgery
Introduction
Surgical rejuvenation of the face, commonly referred to as facelifts or rhytidectomy, has grown increasingly popular in an age-conscious society [1]. Modern techniques such as the SMAS lift, deep plane facelift, and short-scar facelift have advanced significantly, addressing a wide range of different patient expectations and offering more natural (i.e., less visible scarring, shorter downtime) and longer-lasting results. These procedures involve repositioning and tightening of the SMAS layer, rather than just tucking the skin, to achieve a more youthful contour and balanced facial aesthetics.
The Superficial Musculoaponeurotic System (SMAS) is a complex layer of facial tissue and plays a crucial role in facial expression and surgical facial rejuvenation. Initially described by Mitz and Peyronie in 1976 [2], the SMAS has become an anatomical landmark and conceptual hallmark in facial plastic surgery, particularly in facelift procedures [3]. This fibromuscular network is situated between the subcutaneous and deep fat compartments of the face, providing structural support and transmitting the forces of facial muscles to the skin, thereby influencing facial aesthetics and aging.
Despite the advancements and benefits of facelift surgeries, they come not without the risk of complications [4]. One of the primary concerns is facial or trigeminal nerve damage, which can lead to facial muscle weakness, numbness, or even paralysis. Techniques that involve more extensive undermining and releasing of the SMAS and facial ligaments, such as the extended sub-SMAS, high lateral SMAS, deep plane, and composite rhytidectomy, are often associated with a higher rate of temporary or permanent nerve injuries compared to more conservative SMAS techniques (e.g., SMAS plication, imbrication, or SMASectomy) [5]. Specifically, the facial nerve, which innervates the muscles of facial mimicry, is at risk during these procedures. Damage to the temporal branch of the facial nerve can impair raising of the eyebrows, whilst injury to the marginal mandibular branch may cause asymmetry in the smile [6]. Other common complications include hematoma, seromas, infection, and scarring. The list of potential complications reinforces the need for of refined surgical techniques and thorough patient consultation and planning.
This study aims to propose a novel facelift surgical technique that is safe, reliable, easily applicable, and comes with a steep learning curve. Unlike SMAS techniques, our approach relies on a specific sequence of SMAS plications, that ultimately involves platysma manipulation. Overall, this technique may help reduce perioperative complications and improve patient outcomes.
Materials and Methods
In this retrospective study, 209 female patients were enrolled. The average age of the patients at the time of surgery was 59.3 ± 6.8 years [range: 48 – 83], and the average BMI was 24.3 ± 1.88 kg/m2 [range: 21.5 – 28.0]. The patients underwent facelift surgery for aesthetic and rejuvenation purposes between January 2012 and December 2022 in the private practice of the study’s first author (G.C.). Only 5% (n=10) of all patients underwent secondary facelift procedures. None of the patients reported any surgically relevant preoperative comorbidities or health conditions. Notably, no diabetic or anticoagulationtreated patient or strong smoker (more than 10 cigarettes per day) was included in the study group.
Each patient presented with an inferior descent of facial soft tissues of moderate to severe extent. The study adhered to the principles of the Declaration of Helsinki; however, since the surgery was conducted in a private practice, the study was not approved by an institutional review board. All patients provided written informed consent for the facelift procedure, as well as for the use of their photographs and data for scientific purposes including publication.
Surgical technique
All facelift procedures were performed under general anesthesia or under deep sedation associated to local anesthesia.
The primary incision of the skin begins at the caudal aspect of the temporal hairline, extends to the superior pole of the ear then caudally along the contours of the ear and the tragus (preferentially post-tragal). The preparation continues by circumscribing the external ear and proceeding into the hair of the occipital region.
The subcutaneous flap was uniformly elevated until the location of the zygomatic muscles, until reaching 1 cm medially to the midpupillary line. The postauricular skin was then dissected in a similar subcutaneous fashion and connected to the anterior facial dissection.
In the cervical region, the subcutaneous flap was elevated with the same medial extension as the anterior dissection at the mandibular line, reaching the level of the cricoid cartilage, inferiorly.
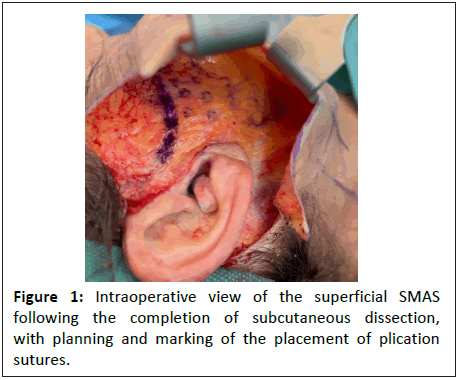
Once the subcutaneous flap has been raised and the SMASplatysma system exposed from the temporal region superiorly, to the nasolabial fold medially, and the platysma inferiorly, plications were performed in the deep subcutaneous layer, as shown in Figure 1.
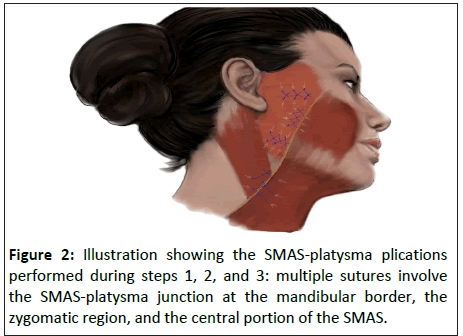
SMAS-Platysma junction plications: Three to four vertical plications (equidistant approximately 0.5 cm to 1 cm to each other) are performed to shorten the SMAS-platysma junction. This allows the definition of the jawline and puts the platysma back into vertical tension. Unlike the facial SMAS, the platysma ages by collapsing downwards what causes herniation of deep subplatysmal fat.
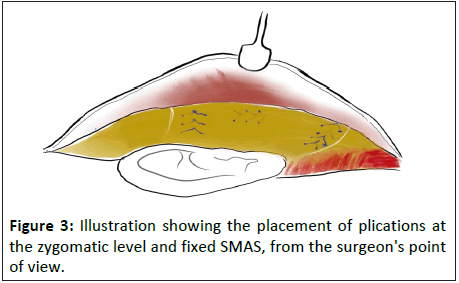
Zygomatic plications: Another series of three plications is done approximately 1 cm caudal to the zygomatic arch, oriented parallel to the zygomatic arch, aiming to tension the SMAS fascia and consequently redraping the descended fat of the superficial compartment.
Nasolabial fold plications: After the initial horizontal plications (points 1-2), parallel plications are made along the nasolabial fold (3-4 cm laterally the groove) to further shorten the SMAS in a latero-medial direction. This part of the procedure follows the SMA Sectomy technique proposed by Baker, but without the avulsion of the fascial tissue, instead adhering to its direction [7].
This fist three steps are visualized in Figures 2-3.
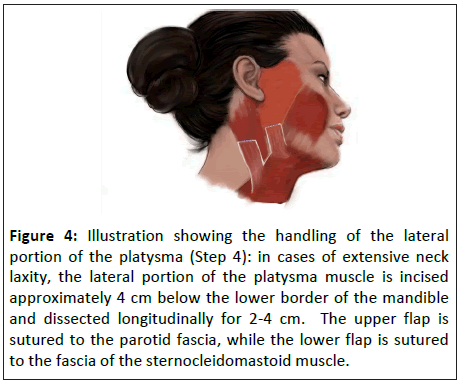
Neck treatment: Concerning neck manipulation (which is under tension after the first step), an incision is made 4 cm below the mandibular line, parallel to the mandibular border, approximately 2-4 cm in length.
Two platysma flaps are created: The superior flap is fixed to the fascia of Lore, if accessible; otherwise, it is fixed more caudally but always posterior to the angle of the mandible, while respecting the nervous structures. The inferior flap is then sutured more supero-laterally to the fascia of the sternocleidomastoid muscle. This dual fixation approach ensures a firm and defined neck contour, as seen in Figure 4.
Figure 4: Illustration showing the handling of the lateral portion of the platysma (Step 4): in cases of extensive neck laxity, the lateral portion of the platysma muscle is incised approximately 4 cm below the lower border of the mandible and dissected longitudinally for 2-4 cm. The upper flap is sutured to the parotid fascia, while the lower flap is sutured to the fascia of the sternocleidomastoid muscle.
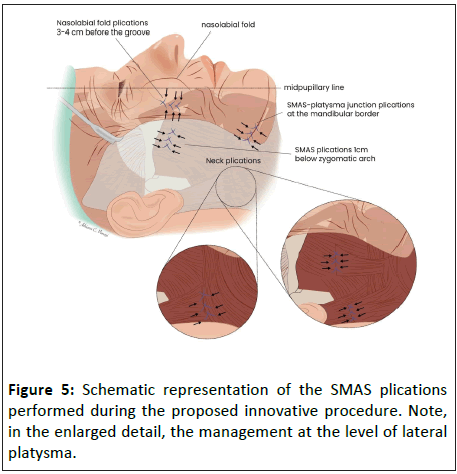
This combination of plications prevents integumental overextension by preserving individual, dynamic and anatomical boundaries, while maintaining excellent mobility (Figure 5).
Throughout all steps of this surgical approach, a nerve stimulator (Neuropacer – F1745, FIAB, Firenze, Italy) was utilized to identify and protect superficial terminal nerve branches of the facial nerve within the tissue to be plicated, thereby helping the surgeon avoid direct or indirect damage to these nerve branches.
The plication of the SMAS was carried out using a nonresorbable polyester-coated suture (3.0 Ethibond®, Johnson&Johnson, NY, USA).
Once the SMAS-platysma has been thickened and tightened, the redundant skin was meticulously excised and resuspended to allow a tension-free skin closure.
Outcome evaluation
To validate the outcomes of our face-lift technique, we reviewed postoperative photographs of 209 patients who underwent the procedure. These standardized photographs were taken at intervals of 1, 2-, 3-, 6-, and 10-years post-surgery from frontal, 45-degree, and lateral angles.
Three facial plastic surgeons, blinded to patient identities and treatment specifics, assessed the photographs. They evaluated four facial and neck features—jawline contour loss (jowls), nasolabial fold prominence, marionette lines, and the centrallateral neck region—using a 7-point Likert scale (1 = "None" to 7 = "Severe"). These evaluation criteria were selected based on the authors' clinical expertise.
A 7-point visual analog scale was employed for rating at each time point, as summarized in Table 1.
| Severity of jawline continuity loss (or jowls) | ||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| None | Moderate | Severe | ||||
| Severity of nasolabial fold | ||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| None | Moderate | Severe | ||||
| Severity of marionette line | ||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| None | Moderate | Severe | ||||
| Severity of central-lateral aspect of the neck | ||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| None | Moderate | Severe | ||||
Table 1: The observers used this visual analog scale to rate the patients’ photographs.
Results
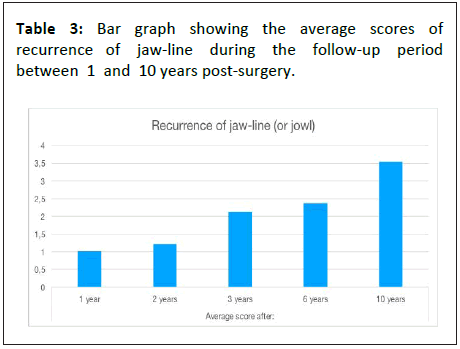
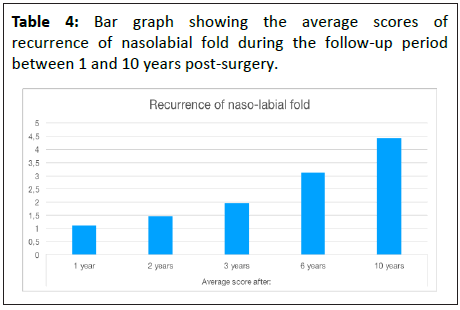
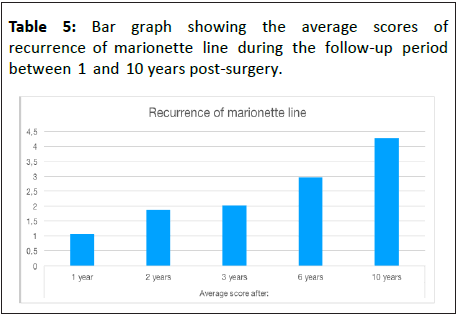
Each parameter in this retrospective, rating-based study demonstrated significant improvement in the severity of jawline contour loss, nasolabial fold, marionette lines within the first three years following surgery. Among the areas assessed, jawline contour loss showed the least severity over time, with an average rating of 3.54 at the ten-year mark.
Table 2 provides a summary of the average scores for each parameter at 1, 2, 3, 6, and 10 postoperative years.
| Parameters evaluated | Average score after | ||||
|---|---|---|---|---|---|
| 1 year | 2 years | 3 years | 6 years | 10 years | |
| Recurrence of jawline (or jowl) | 1,02 | 1,21 | 2,13 | 2,37 | 3,54 |
| Recurrence of nasolabial fold | 1,10 | 1,46 | 1,96 | 3,12 | 4,43 |
| Recurrence of marionette line | 1,05 | 1,87 | 2,02 | 2,97 | 4,28 |
| Recurrence of central-lateral aspect of the neck | 1,31 | 1,56 | 2,14 | 2,32 | 4,58 |
Table 2: Average scores of each parameter evaluated during the follow-up at 1, 2, 3, 6 and 10 years.
Subsequently, a gradual, consistent decline in scores was observed for each parameter, as shown in Table 3-6, indicating a reduction in tissue tone quality and a moderate recurrence of facial.
Discussion
The development of facial lifting techniques has led to various approaches, such as Hamra's super extended rhytidectomy [14] and Ramirez's subperiosteal technique [15] according to Stuzin [16], with additional endoscopic support or the opening of retaining ligaments. These methods, while advanced, always involve complete SMAS-platysma detachment, repositioning and fixation of their margins, often with undesirable effects such as facial volume reduction and exacerbation of aging. Furthermore, these techniques are associated with a relatively high complication rate, such as palsy, hematomas.
Selecting the appropriate facelift technique has long been a complex decision for plastic surgeons, as a as a technique that delivers optimal results for one patient may not yield the same outcome for another. The pursuit of consistent and reproducible results has led to the development and refinement of diverse techniques, with the ultimate goal of achieving maximum safety and efficacy. The technique presented in this article represents the culmination of decades of experience in the field of facial rejuvenation surgery. It provides targeted lifting and harmonious contouring of the mid, and lower face, as well as the neck, while effectively preserving the patient’s unique facial features and identity [8].
Many facelift techniques involve extensive manipulation of the SMAS-platysma complex, often resulting in prolonged recovery periods and an increased risk of medium- and longterm complications. According to a meta-analysis of Jacono et al., the rate of nerve injury in such procedures can reach 1.85%, a non-trivial risk that highlights the need to prioritize patient safety, especially in elective surgeries for cosmetic purposes. In this context, nerve injury rates of up to 1.85% have been described in a meta-analysis by Jacono et al. [5] While this rate is relatively low compared to other surgical procedures, it is important to consider that any facial complication can profoundly impact a patient’s quality of life, underscoring the importance of minimizing such risks.
In our experience of 209 procedures over a 10-year period, we observed only three cases of complications: two instances of delayed superficial wound healing disorder in the sideburn area and one case of cervical hematoma, which developed 48 hours postoperatively and was drained via a subcutaneous pathway in the occipital region.
It is important to note that these complications are more attributable to general risks of surgical procedure itself rather than the specific facelift technique. Importantly, we encountered no cases of temporary palsy or facial nerve injury, as our technique does not involve opening or lifting the SMAS layer, which remains intact to shield the underlying facial nerve branches. In addition, the intraoperative use of a nerve stimulator further safeguarded against unintentional involvement of terminal nerve branches in the suturing process.
Based on the blinded evaluations by surgeons, a series of conclusions can be drawn regarding the effectiveness of the surgical technique presented in this study. The parameter showing the least recurrence during the follow-up period is jawline appearance, particularly concerning jowl recurrence. This stability can likely be attributed to a key technical maneuver in the first phase of the procedure: plication sutures are placed in the platysma muscle near its junction with the SMAS. This technique, involving both adipose tissue and platysma muscle fibers, creates durable support and enhances the longevity of the lift. This approach addresses multiple vectors simultaneously. A vertical shortening vector defines and reinforces the mandibular angle by repositioning the adipose tissue and tightening the septum and mandibular ligament. In addition, plications at the zygomatic level, performed in the second step, elevate the descended fat pads of the cheek, alleviating strain on the jawline. Finally, a superolateral traction vector is established in the fourth step, where the posterior upper portion of the platysma is securely anchored to Lore’s fascia, ensuring stability and support over time.
In the correction of nasolabial folds and marionette lines (step 3), the approach to the SMAS in the midface focuses on enhancing fibroadipose tissue thickness through plications, effectively restoring lost volume at the zygomatic eminence. This technique preserves the deep bony support of the zygomatic and masseteric cutaneous retention ligaments. While it is traditionally believed that the SMAS forms a continuous sheet extending anteriorly to the parotid region, our findings suggest that this may vary due to the layered arrangement of facial muscles in the medial face. Literature increasingly supports the idea that SMAS structure and continuity differ across facial regions [9]. We developed this technique, drawing on our extensive experience in facial lifting, and concluded that deep dissections under the SMAS, medially to the midpupillary area, are ineffective for increasing its tightness. This is often due to the SMAS in the mid-cheek area not presenting as a distinct, continuous sheet during surgery, making it challenging to clearly identify and dissect. It is frequently encountered as a less defined and more variable plane. The limited structural integrity in this area reduces its ability to provide adequate tissue support.
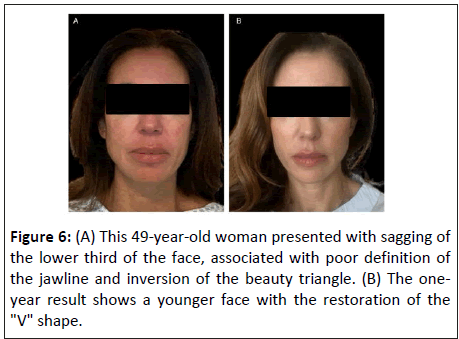
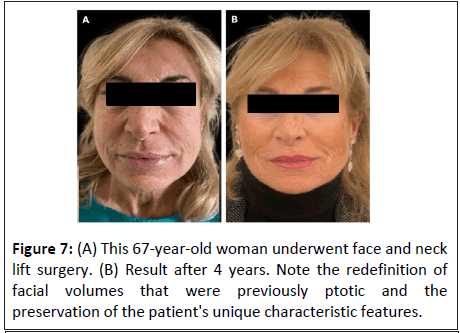
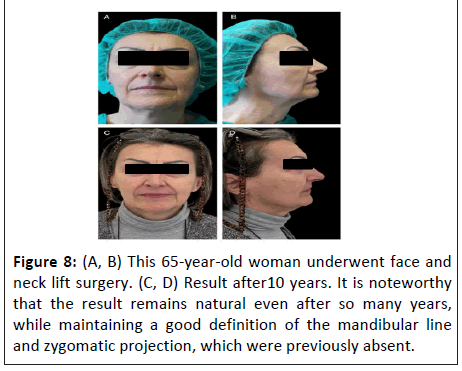
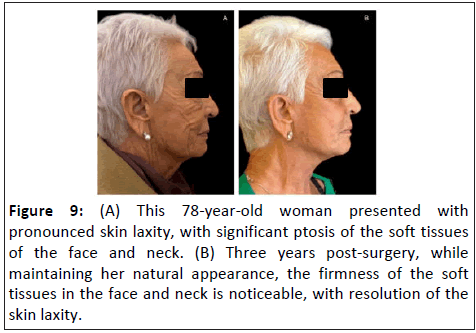
The critical concept underlying this innovative facial lifting technique is the preservation of facial retaining ligaments. Cutting these ligaments during surgery can disrupt the architectural integrity of the face, leading to premature sagging and compromised results [10]. The available body of research supports our idea that maintaining the natural ligamentous structures helps sustain facial contour and function [11]. Another important detail is that the facial SMAS, composed fibrous, muscular and adipose tissue, is often cited as the primary structure involved in facial aging. However, this process is influenced not only by photoaging damage of the skin and by the natural loss of collagen and elasticity but also by the resorption of bony structures and their volumetric and positional changes, as well as a redistribution of both superficial and deep adipose tissue [12]. As we previously demonstrated [10], facial retaining ligaments are the most resilient support structures for facial soft tissues, in contrast to other layers that are subject to remodeling and aging. Our technique prioritizes the preservation of facial ligamentous structures and reinforces SMAS thickness through strategic plications, effectively preventing soft tissue sagging while simultaneously maintaining each patient’s unique aesthetic features. Clinical results are shown in Figures 6-9.
Figure 9: (A) This 78-year-old woman presented with pronounced skin laxity, with significant ptosis of the soft tissues of the face and neck. (B) Three years post-surgery, while maintaining her natural appearance, the firmness of the soft tissues in the face and neck is noticeable, with resolution of the skin laxity.
The individuality of a person's facial expression is sometimes diminished after conventional facelift techniques, which can lead to over- or under-correction of key facial features, leading to an altered appearance. Other potential issues include excessive lateral tension around the mouth, inadequate lifting of the midface, over-enhancement of midface structures, unnatural volume in the cheeks, and a “mask-like”, expressionless look.
Our technique follows two core objectives: on one hand, reinforcing the SMAS-platysma layer through targeted plication without altering its natural architecture; and on the other, preserving each patient's facial identity after the surgical rejuvenation. A major advantage of this surgical technique lies in its preservation of the structural architecture of the fat compartments in the the deep subcutaneous tissue, which is highly structured and divided into defined, cosmetically relevant anatomical zones. By maintaining this intersegmental connection between these zones, both segmental compression and excessive dilatation effects can be avoided.
The plication pattern in this technqiue is designed to selectively and precisely thicken the various adipose compartments underlying key anatomical regions aligning with to Rohrich and Pessa’s fat compartment theory. This posits that facial aging does not occur unifromly but compartment-specific, whereby deep fat is prone to atrophy, while superficial fat tends to shift downward within its boundaries. This inferior displacement is thought to be the results from a combination of ligamentous laxity and pseudoptosis driven by deep fat compartment volume loss, with no consensus as to which cause plays a greater role. The goal of our novel facelift technique is to restore the proper volumes of each compartment while counteracting the age-related natural downward facial sagging.
It is important to highlight that our technique allows for a comprehensive facial reshaping, while providing an integrated safeguard to prevent excessive tension that could alter the face’s natural identity. Another key advantage over other SMAS facelift techniques is its durability: the SMAS is a solid structure that stabilizes the tissues, yet it remains flexible enough to enhance the elasticity and stability in the treated areas. We believe that a deep dissection of the SMAS is justified only in the neck region. This is because it does not involve a thin fascia; rather, it entails dissecting and consequently suspending an actual muscle, the platysma, which has considerable thickness compared to the SMAS and it is equipped with contractile and tensile force.
Importantly, the detachment of the platysma does not exceed 6 cm from the mandibular edge downwards. Research showed that only the upper 5–6 cm of the platysma influence lower face structures, while the lower segment primarily lifts tissues toward the clavicle [13].
In this study, neck recurrence showed the highest score among all parameters (Table 2). This is likely because, in none of the treated cases, the neck was opened centrally. The recurrence of the platysmal bands, along with the progressive hypertrophy of the submental adipose tissue, would require also a central neck approach, including direct lipectomy and midline platysmal band suturing.
Conclusions
The current technique is based on two main components: SMAS tethering through multiple SMAS-platysma plications and the preservation of facial retaining ligaments. We believe this approach represents a significant advancement, maintaining the patient’s natural aesthetics while avoiding common pitfalls associated with traditional techniques including facial nerve injury, and ensuring a more harmonious and lasting tissue repositioning.
Facelift surgery demands a nuanced understanding of facial anatomy and meticulous planning. By re-evaluating traditional SMAS concepts and emphasizing the preservation of facial retaining ligaments, the proposed technique aims to deliver natural and enduring outcomes. Continued research and clinical observation will be essential in refining this method, further contributing to the evolution.
References
- (2022) Surgery, American Society of Plastic. ASPS Procedural Statistics Release. USA
- Vladimir M, Martine P (1976) The superficial Musculo-Aponeurotic System (SMAS) in the parotid and cheek area. Plast Reconstr Surg 58: 80-88.
[Crossref] [Google Scholar] [Indexed]
- Gamboa GM, de La Torre JI, Vasconez LO (2004) Surgical anatomy of the midface as applied to facial rejuvenation. Ann Plast Surg 52: 240-245.
[Crossref] [Google Scholar] [Indexed]
- Baker DC (1983) Complications of cervicofacial rhytidectomy. Clin Plast Surg 10: 543-62.
[Crossref] [Google Scholar] [Indexed]
- Jacono AA, Alemi AS, Russell JL (2019) A meta-analysis of complication rates among different SMAS facelift techniques. Aesthet Surg J 39: 927-942.
[Crossref] [Google Scholar] [Indexed]
- Rocha FS, Rocha CM, Viterbo F, Labbé D (2019) Facelift and facial nerve injury: How to deal with? Rev Bras Cir Plást 32: 299-305.
- Baker DC (1997) Lateral SMASectomy. Plast Reconstr Surg 100: 509-513.
[Crossref] [Google Scholar] [Indexed]
- Connell BF (2008) Pushing the clock back 15 to 20 years with facial rejuvenation. Clin Plast Surg 35: 553-566.
[Crossref] [Google Scholar] [Indexed]
- Minelli L, van der Lei B, Mendelson BC (2024) The superficial musculoaponeurotic system: Does it really exist as an anatomical entity? Plast Reconstr Surg 153: 1023-1034.
[Crossref] [Google Scholar] [Indexed]
- Distefano A, Dotto A, Garlaschi A, Colombo G (2024) Instrumental analysis of retaining ligaments and literature review. What can we deduce? Journal of Craniofacial Surgery 2: e0018.
- Funk W (2017) Presto lift-a facelift that preserves the retaining ligaments and SMAS tethering. Oral Maxillofac Surg 21: 33-39.
[Crossref] [Google Scholar] [Indexed]
- Mendelson B, Wong CH (2013) Anatomy of the aging face. Plastic Surgery 2: 78-92.
- Ohana O, Fezza JP, Sykes J, Yoelin SG, Lee JH, et al. The platysma contraction pattern in healthy adults: A vector analysis study. Plast Reconstr Surg 153: 601-607.
[Crossref] [Google Scholar] [Indexed]
- Hamra ST (1998) The zygmorbicular dissection in composite rhytidectomy: An ideal midface plane. Plast Reconstr Surg 102: 1646.
[Crossref] [Google Scholar] [Indexed]
- Ramirez OM (1995) Endoscopic facial rejuvenation. Perspect Plast Surg 9: 22.
- Stuzin JM, Baker TJ, Gordon HL, Baker TM (1995) Extended SMAS dissection as an approach to midface rejuvenation. Clin Plast Surg 22: 295.
[Crossref] [Google Scholar] [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences