Basocellular Carcinoma and Pyoderma Gangrenosum: A Case Report
Ed Hartman, Emilie Pfeifle and Frans Koedijk
DOI10.4172/2472-1905.100010
Ed Hartman1*, Emilie Pfeifle1and Frans Koedijk2
1 Department of Plastic and Reconstructive Surgery, Elisabeth Hospital, Tilburg, The Netherlands
2 Department of Dermatology, Elisabeth Hospital, Tilburg, The Netherlands
- *Corresponding Author:
- Ed Hartman
Department of Plastic and Reconstructive Surgery
Elisabeth Hospital, Tilburg, The Netherlands.
Tel: 013-5391313
E-mail:hartman@nvpc.nl
Received date: December 05, 2015; Accepted date: January 02, 2016; Published date: January 12, 2016
Citation: Hartman E, Pfeifle E, Koedijk F. Basocellular Carcinoma and Pyoderma Gangrenosum: A Case Report. J Aesthet Reconstr Surg. 2016, 2:1. doi: 10.4172/2472-1905.100010
Abstract
Pyoderma gangrenosum is a rare acute noninfectious dermatosis. It can develop spontaneously, or be provoked by trauma, and can progress rapidly. The cause of pyoderma gangrenosum is unknown. It is thought to be a variant of vasculitis, and in about 50% of all cases it is associated with internal diseases, like colitis ulcerosa or Morbus Crohn. There is no test available, which can diagnose pyoderma gangrenosum with certainty. A biopsy can be taken, but the diagnosis is ultimately based on the clinical findings. The disease is treated with immunosuppressants, like Prednisone or Cyclosporine.
This case report describes a 61-year old female, who was operated on for multiple basocellular carcinomas of the skin. Four days after the operation, the patient was admitted for a suspected wound infection. Despite multiple debridements and broad-spectrum antibiotics, the wounds progressively deteriorated. The diagnosis pyoderma gangrenosum was considered. A biopsy showed an acute inflammation with abscess formation, which supported the diagnosis. Prednisone therapy was started and the patient recovered completely. This case report shows an unusual example of pyoderma gangrenosum, which to our knowledge has not been described before.
Keywords
Pyoderma gangrenosum; Dermatosis; Vasculitis
Introduction
Pyoderma gangrenosum was first described by Brunsting et al in 1930 [1]. It is a very rare, but serious and destructive noninfectious neutrophilic dermatosis. The general incidence has been estimated to be around three to ten per million per year. The peak incidence is between 20 and 50 years and occurs more in women than in men [2].
The lesions may appear on any part of the skin, with a preference for the pretibial aspect of the lower extremities. It can affect patients of every age, especially between 30 and 40 years and is rare in children and adolescents [3]. It can develop spontaneously or be provoked by trauma, such as injury, an insect bite, biopsy, but also operation, and can progress rapidly. In 25-50% of cases the pathergy test is positive; a prick with a needle causes a pustule or bulla. The skin lesion begins as a (painful) nodus or infiltrate with a red edge and there can be development of pustules, bullae or papules. Soon an irregular, deep (to the fat or the fascia) ulcer develops, from which a mucopurulent or hemorrhagic exudate flows. There can be necrosis on the edges of the wound that are still attached to the periphery. The ulcers have an undermined bluish border with surrounding erythema. Healing can occur spontaneously after weeks to months. This happens in episodes, and several scars from previous episodes can be seen. Systemic manifestations can occur, such as infiltrates in the lungs, intestines, eyes, bones and lymph nodes. Furthermore malaise, arthralgia and fever are seen.
The cause of pyoderma gangrenosum is unknown. It is thought to be a variant of vasculitis. In about half of all cases it is associated with internal diseases, especially colitis ulcerosa (0,6-5,0% of colitis ulcerosa patients develop pyoderma gangrenosum), Morbus Crohn and rheumatoid arthritis. Associated diseases can appear before, during or after the onset of the ulcers [4]. As stated in a review in 2011, pyoderma gangrenosum is one of the most common extra-intestinal manifestations of chronic inflammatory bowel disease [5]. About 25% of cases occur as an isolated process [3].
Case Report
A 61-year old female presented with four basocellular carcinomas of the skin on both arms and the neck. The lesions were excised under local anesthesia and sent for histopathology.
Two days after the operation, the patient was seen at the emergency department with complaints of pain. No signs of infection were noticed and no intervention was deemed necessary. Four days after the operation, she developed what seemed like an infection of two of the wounds. Antibiotics were prescribed (Amoxicillin/Clavulanic Acid). Two days later, the patient returned to the outpatient clinic with progression of her complaints and her temperature was above 38°C. Another wound was now infected as well and cultures were taken. The patient was admitted to the ward and IV antibiotics (Amoxicillin/ Clavulanic Acid) were started.
The same day the lesions were debrided in the or during surgery, a cellulitis with superficial fat necrosis was found and one wound on the left upper arm showed a deeper infection of the fat below Scarpa’s fascia. The diagnosis necrotizing soft tissue infection was made. The wounds were flushed, and again cultures were taken. The antibiotics were switched to Penicillin and Clindamycin because of progression of the infection under Amoxicillin/ Clavulanic Acid. All cultures remained negative.
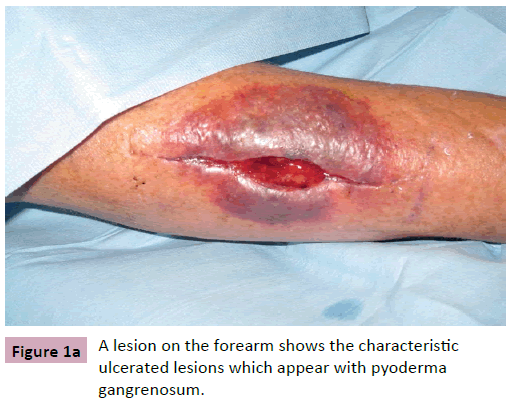
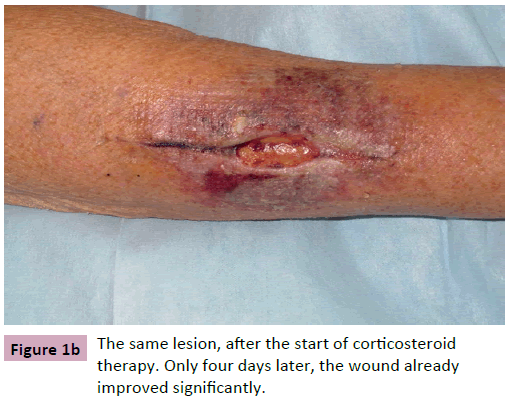
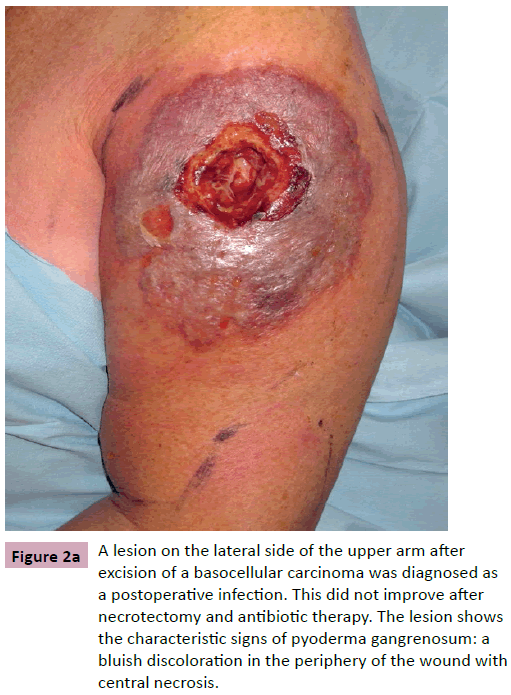
Despite the surgery, the wounds did not improve, but actually became worse (Figures 1a and 2a). Another debridement was needed and again antibiotics were changed, this time into Ceftazidim and Tobramycin.
Figure 2a: A lesion on the lateral side of the upper arm after excision of a basocellular carcinoma was diagnosed as a postoperative infection. This did not improve after necrotectomy and antibiotic therapy. The lesion shows the characteristic signs of pyoderma gangrenosum: a bluish discoloration in the periphery of the wound with central necrosis.
Because of the bad response to surgery and antibiotics, the diagnosis pyoderma gangrenosum was considered and the department of dermatology was consulted. A biopsy was taken and Prednisone intravenously 40mg daily was started. The biopsy showed an acute inflammation with abscess formation, but without any visible bacteria, consistent with pyoderma gangrenosum.
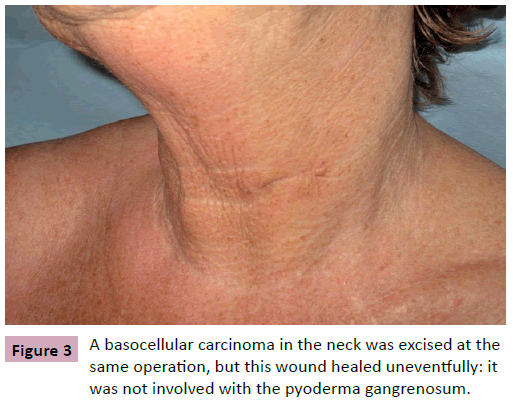
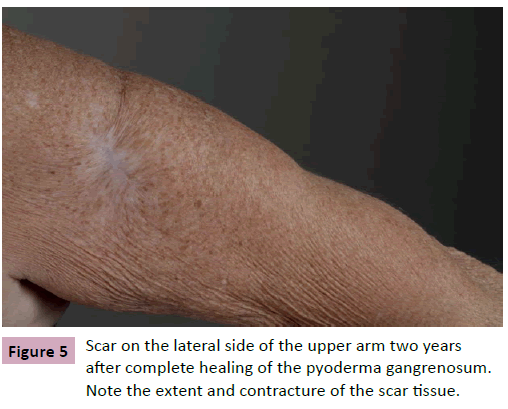
Four days after starting Prednisone, the patient improved. The fever subsided and the wounds became more superficial and granulation tissue occurred Figures 1b and 2b. The patient was discharged and in the following months, all wounds healed by secondary intention. After one week, the Prednisone was reduced to 30 mg daily. Because the clinical condition of the patient kept improving, the Prednisone was reduced to 25 mg daily per os. Every week the dose was lowered with 5 mg until it was stopped after six weeks. Full clinical remission was obtained after three months (Figures 3-5). Especially the affected area on the upper arm resulted in a contracted scar.
Now more than four years after the operation, no recurrences of the pyoderma were noted. Even after another excision of a basal cell carcinoma one year after the operation, no pyoderma developed despite the fact that patient did not receive any medical therapy as a prophylactic measure.
Discussion
There is no test available that can diagnose pyoderma gangrenosum. A biopsy can be taken and histological features show nonspecific inflammation by thrombosis and necrosis. Exclusion of infectious causes is necessary, as sometimes it can be indistinguishable from a necrotizing infection [4]. The diagnosis is made based on the clinical findings. The choice for therapy depends on the severity of the wounds and the rate of progression. In case of a fast progression with damage of the skin, it is important to stop the disease with immunosuppressants, preferably Prednisone, which takes effect directly. Cyclosporine is also effective, but has the disadvantage that it can take up to several weeks before the desired effect has been realized. In severe cases, the two medications may be combined. After improvement of the symptoms, the Prednisone can be phased out, and only Cyclosporine continued. Sometimes treatment is necessary for months or even years. Surgical debridement can occasionally worsen the condition by leading to extension of the disease; therefore surgical management of the wounds is controversial [4, 5].
Pyoderma gangrenosum after excision of skin malignancies is rare and to our knowledge has not been described before. In this case the diagnosis was considered only after the hypothesized infection did not react to the usual therapy and wound cultures remained negative for some time.
The diagnosis is frequently missed and often mistaken for an infection or sometimes even skin malignancy. Patients receive antibiotic treatment or surgical debridement unnecessarily. The latter can lead to further extension of the disease [6]. Therefore it is essential to know more about this disease and to recognize it early so unnecessary intervention and morbidity can be prevented or minimized.
Previous case reports and studies have shown that pyoderma gangrenosum reacts well to corticosteroids and resolution within ten days after treatment has been reported. Alternate choices of treatment are Azathioprine, Cyclosporine or other non-steroidal immunosuppressive agents [3].
Some dermatologists advise that surgery is contraindicated in patients with a past history of pyoderma gangrenosum and that, if surgery is really necessary, dermatological consultation and aggressive medical treatment with steroids is essential to prevent recurrence [7]. This was not supported by our case report: a second operation one year after the first one did not result in a recurrence of pyoderma.
Pyoderma gangrenosum has been described to occur after several plastic surgical procedures, such as reduction mammoplasty, skin grafts and breast reconstruction, and after burn wounds. Therefore it is important not only for dermatologists, but also for plastic surgeons to know and recognize this disease.
If a patient develops a wound infection that does not react to the regular surgical treatments and antibiotics, the diagnosis pyoderma gangrenosum should definitely be considered and a dermatologist should be consulted.
References
- Brunsting LA, Goeckerman WH, O'Leary PA (1930)Pyoderma (echthyma)gangrenosum: clinical and experimental observations in five cases occurring in adults. Arch Dermatol22: 655-680.
- Wollina U (2007) Pyodermagangrenosum--a review. Orphanet J Rare Dis 2:19.
- Caterson SA, Nyame T, Phung T, Lee B, Tobias AM (2010)Pyodermagangrenosumfollowing bilateral deep inferior epigastric perforator flap breast reconstruction. J ReconstrMicrosurg 26:475–479.
- Rajapakse Y, Bunker CB, Ghattaura A, Jallali N,Henton J, et al. (2010) Case report: pyodermagangrenosum following Deep Inferior EpigastricPerforator (Diep) free flap breast reconstruction. J PlastReconstrAesthetSurg 63:e395–e396.
- Wollina U, Haroske G (2011)Pyodermagangraenosum. CurrOpinRheumatol23:50–56.
- Jain A (2000)Pyodermagangrenosum occurring in a lower limb fasciocutaneous flap– a lesson to learn. British Journal of Plastic Surgery53:437–440.
- Souza B, Millard R, Flemming S (2001)Pyodermagangrenosum: beware, itdoes recur. British Journal of Plastic Surgery54: 82.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences