An Update on Hair Restoration
David Chan and Yadranko Ducic
DOI10.4172/2472-1905.100008
Fort Worth, TX 76104, USA
- *Corresponding Author:
- Yadranko Ducic
Otolaryngology and Facial Plastic Surgery Associates 923 Pennsylvania Avenue
Suite 100, Fort Worth, TX 76104, USA
Tel: 8179200484
Fax: 8179200068
E-mail: yducic@sbcglobal.net
Received: December 17, 2015, Accepted: December 29, 2015, Published: December 31 2015
Citation: Chan D, Ducic Y. An Update on Hair Restoration. J Aesthet Reconstr Surg. 2016, 1:8. doi: 10.4172/2472-1905.10008
Abstract
Hair restoration therapy has evolved significantly over the past few decades. Aesthetically pleasing and natural results are achieved with modern techniques utilizing follicular unit transfer. While the concept remains the same, various techniques have been developed for harvesting follicular units safely and reliably. Here, we review some of the techniques of obtaining follicular units for transplantation, medical treatment of androgenetic alopecia, and future directions in hair restoration therapy.
Introduction
Hair transplant surgery has made significant strides over the past 25 years that has resulted in highly satisfied patients. The movements from mini- and micro-grafting techniques to the now standard follicular grafting techniques have resulting in more aesthetically pleasing and natural appearance of transplanted hair [1,2]. While the strip technique is the most practiced method of donor harvest, follicular unit extraction (FUE) techniques are gaining ground, particularly with commercial products. In this review, we will discuss the current standard, emerging trends, and the future of hair restoration therapy.
Pathophysiology
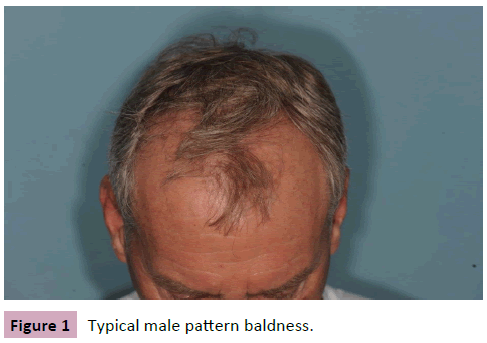
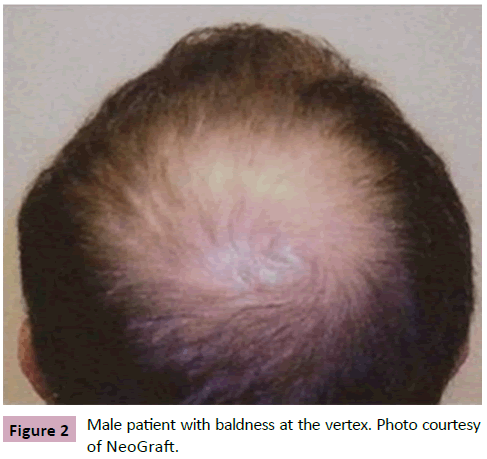
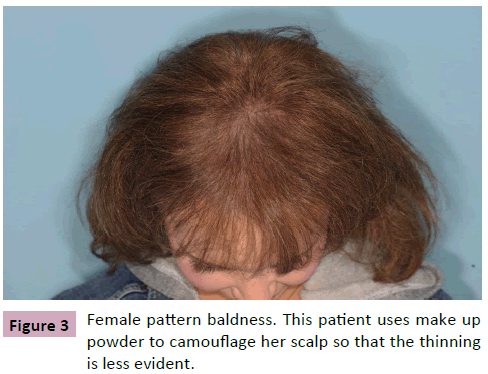
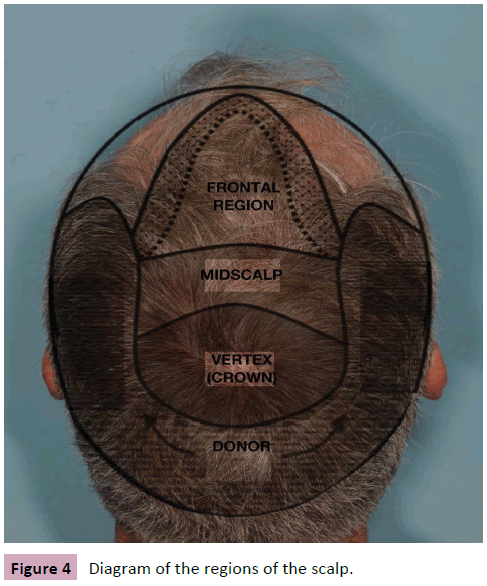
Androgenetic alopecia (AGA) is the most common form of hair loss in both men and women. By the age of 40 years, half the white male population is affected to some degree by this type of hair loss (Figures 1 and 2). Women are affected by this type of hair loss as young as 20 years old (Figure 3) [3]. In men, hair loss follows a progressive and stereotypical pattern. It begins with hair loss in the bitemporal regions and then progresses to the vertex (Figure 4). The occipital hair is usually spared. The reason for this pattern is due to the different sensitivities of the hair follicles to dihydrotestosterone (DHT). Type 2 5-alpha-reductase converts testosterone into the more potent DHT.
Medical treatment
TheFood and Drug Administration (FDA) has approved two medications, finasteride and minoxidil, to treat this form of hair loss [4]. Both of these drugs increase hair density and decreases further hair loss but does not promote new hair growth.
Finasteride is a selective type II 5-alpha-reductase inhibitor that prevents the conversion of testosterone to dihydrotestosterone. It is taken in 1-mg pill form once daily and is well tolerated. Finasteride can reduce serum DHT levels by up to 70% [5]. The most concerning side effect for men are decreased libido (1.8%), erectile dysfunction (1.3%), and ejaculatory dysfunction (1.2%), which are reversible with discontinuation of the medication [6]. There, however, have been reports of irreversible sexual dysfunction symptoms in some men [7]. Finasteride is contraindicated in women who are or may become pregnant due to concerns of abnormal fetal genitalia development. Furthermore, there was no difference shown in terms of hair loss when postmenopausal women who were given finasteride compared to placebo [4,8].
While not approved by the FDA for use in the United States, dutasteride is being used to treat AGA as well. It is a type I and II 5-alpha-reductase inhibitor that is 100 time and 3 times more potent than finasteride, respectively [9]. In a randomized study, 0.5 mg daily dutasteride performed better than both finasteride and placebo in terms of increased hair growth and width [10]. A meta-analysis showed a similar side effect profile for both finasteride and dutasteride [11]. In addition, patients who do not find benefit from finasteride may find benefit with dutasteride [12]. With increasing evidence, dutasteride may become FDA approved for use in the United States.
Minoxidil was developed as an antihypertensive medication but was found to increase hair survival by an unknown mechanism. It is a topical treatment that comes in 2% and 5% formulation and is approved for both men and women (only the 2% form is approved for women). It is applied to the scalp twice daily. Studies have shown that application of minoxidil improves hair growth. Adverse side effects include scalp irritation, and contact dermatitis. Hypertrichosis can also occur but is more common in women [4].
Ketoconazole is an imidazole antifungal which, when used in shampoo form, has been shown to increase hair growth [13,14]. The exact mechanism by which it works is still unknown. Some hypothesize that it inhibits the DHT pathway in the scalp [15].
Follicular unit transplant
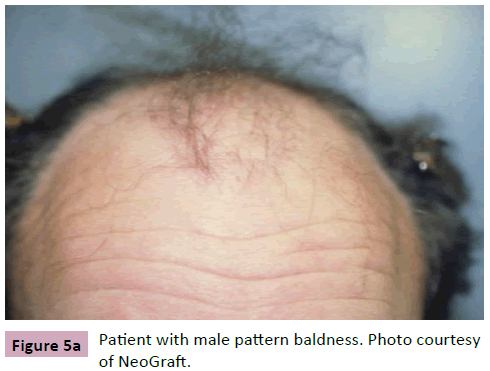
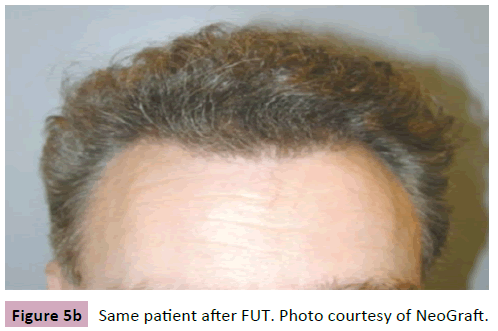
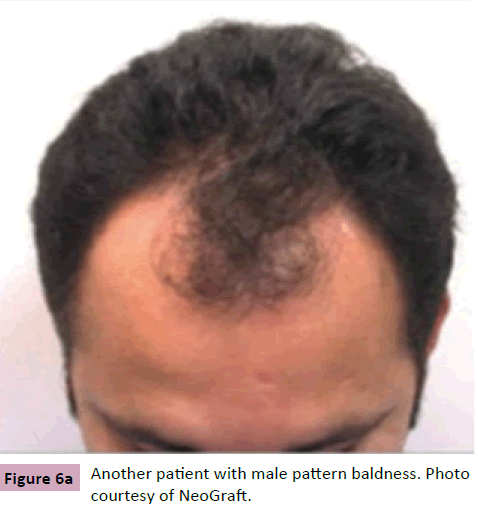
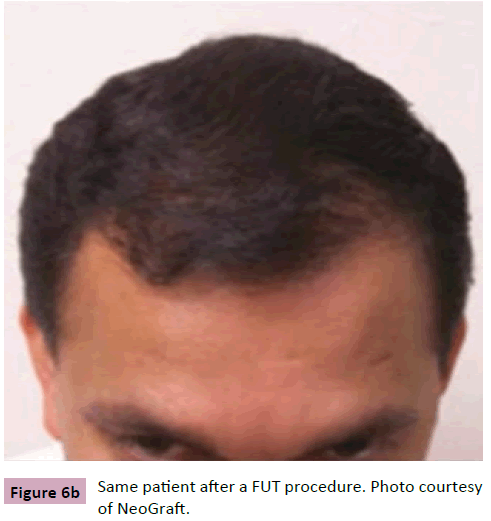
Now considered the gold standard in hair restoration surgery, follicular unit transplant was first described by Bernstein et al [16] Hair grows from the scalp in groupings called follicular units, which contain 1 to 4 terminal terminal hairs, sebaceous unit, and supporting structures [17]. On average, a person has approximately 100,000 to 150,000 hairs at a density of about 2 hairs/mm2 and alopecia is perceptible when hair density diminishes by 50% [18]. These follicular units are harvested from the occipital and temporal scalp (androgen insensitive areas). These follicular units are then placed into the recipient site individually. Utilizing the follicular unit allows for greater density, faster healing, and fewer traumas to the existing hairs in the recipient area. While the number of hairs has not changed, the redistribution gives the appearance of a fuller look (Figures 5a, 5b, 6a, and 6b). Follicular units can be harvested via the traditional strip method or the follicular unit extraction (FUE) method.
Strip method
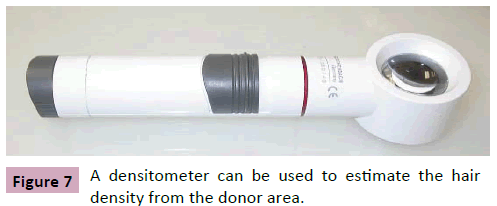
The occipital scalp is used as the donor area. A fusiform-shaped strip is excised from this area in a subcutaneous plane just deep to the hair follicles. The incisions are made parallel to the growth of the hair in order to not transect the follicles. The size of the strip is tailored to the number of grafts needed. The density of the donor region usually ranges from 70 to 120 follicular units per square centimeter, with a mean of 80 follicular units per square centimeter [17]. One can use a hair densitometer (Ellis Instruments Inc., Madison, NJ) to assist in estimating the density per square centimeter and then multiply by the square area to get an estimate of the number follicles harvested (Figure 7). The donor area is then closed primarily with either sutures or staples. In order to minimize the amount of tension on the wound, it is recommended to keep the width less than 10 to 12 mm [17].
The strip is then separated into fine slivers about 2 to 3 follicular units wide. This is performed under a microscope or with magnification. The individual slivers are then sliced into individual follicular units and separated into piles based on the number of terminal hairs. The grafts are then implanted into the recipient sites with careful attention paid to the direction of hair growth and placement to ensure a natural appearance. Recipient sites are created with needles or specialized scalpels. Single hairs are generally placed along the hair line for a more natural look. Using this method, Epstein reported excellent results with minimal complications over a three year period [17].
Follicular unit extraction
The downside of the strip method of harvesting follicular units is that it leaves a scar in the posterior scalp. For patients who want to wear their hair short, the scar becomes much more visible and a cause of distress for patients. Therefore, the FUE method was developed in which follicular units are harvested individually with small punch excisions. Rassman et al described this technique in 2002 [19]. Follicular units are incised with punches ranging from 0.8 to 1.5 mm in diameter and then manually removed with forceps. Their initial experience yielded a 30% transection rate due to difficulty in determining the depth and angle of the hair follicles. Over time, with increased understanding of follicular units and improved instrumentation, the transection rate is now as low as 6% [20]. In general, the complications are minimal with FUE. Hypo- or hyper-pigmentation can occur where the grafts are removed and thinning of the donor area can be seen if too many grafts are removed.
The FUE method is ideal for patients who have little scalp laxity, those who have undergone the strip method in the past, or those who are prone to hypertrophic scarring. FUE can also be used to repair a previous transplant that resulted in a linear hairline or a pluggy appearance [21]. The hairs can be extracted and placed elsewhere for a more natural appearance. The FUE technique can also be used to harvest hair follicles from other parts of the body [22] while the strip method is generally reserved for the posterior scalp.
Post-operative care after FUE is fairly minimal. A pressure dressing is placed on the donor site for a couple of days to help with hemostasis. The recipient site may be itchy and dry so patients are instructed to use a saline spray several times a day to keep the grafts moist. Any minor bleeding at the recipient site can usually be stopped with gentle pressure. The forehead usually swells after the procedure so patients are given steroids post-operatively and are asked to ice the forehead. Patients are asked to gently wash the graft site with cups of water for two weeks. Normal activity can be resumed two weeks after the procedure. Finasteride can be resumed immediately after the procedure. Minoxidil can be resumed one month after the procedure.
Advances in FUE
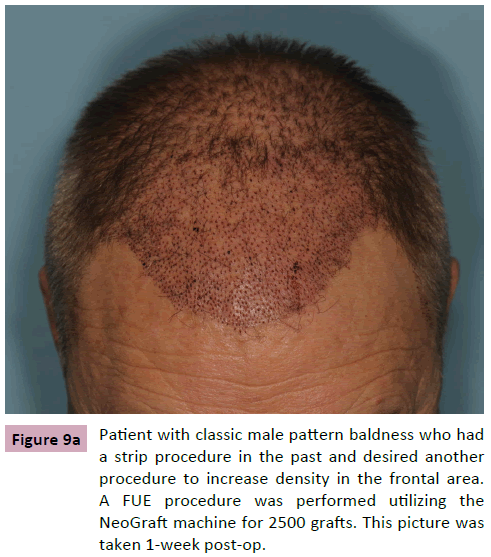
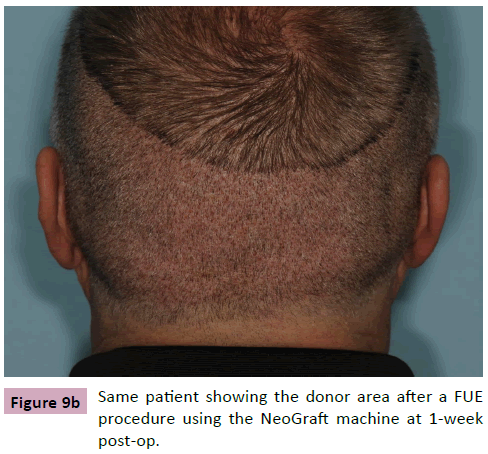
Various types of punches have been developed for FUE. Sharp and dull punches are available in both manual and powered hand pieces. The NeoGraft system (Medicamat, Malakoff, France) utilizes a motorized hand piece for follicular unit extraction. The hand piece has a dull cannula that rotates and incises the grafts and then suctions them into a canister (Figure 8). The assistant then takes the grafts and separates them according to the number of terminal hairs. Trimming of the grafts is rarely needed. The grafts can then be placed into the recipient sites manually with forceps (Figures 9a and 9b). One study showed faster harvest times compared to the traditional FUE method and a transection rate of 5.5% [23].
The ARTAS System (Restoration Robotics, San Jose, CA) is a robotic extraction system. Using a system of cameras and computer software, follicular units are mapped out and extracted. The physician can change the settings from a console. Once the software maps out the follicular units, a robotic arm with a 1 mm, blunt punch incises the graft. The software is also able to space out the extraction to minimize thinning of the donor area. The FDA has reported that the transection rate is as low as 8% for the robotic system. The robot will incise the grafts but does not collect it. The physician or assistant will have to go back and retrieve the grafts for implantation. The benefit of the robotic system is that it excels at repetitive tasks and can do it consistently without fatigue compared to humans [24].
Adjunctive treatments
Low-level light therapy: A Hungarian researcher discovered that by shining a low-powered ruby red laser on the backs of mice increased hair growth. This initial observation has led to other studies showing that low-level light therapy (LLLT) can improve wound healing, reduce inflammation, and reduce the symptoms of stroke [25-27]. The mechanism in which it improves hair growth is still unclear and there is a lack of good scientific studies to fully support its routine use [28].
Platelet rich plasma
Platelet-rich plasma (PRP) contains growth factors that have been shown to improve wound healing [29]. PRP is an emerging trend in hair restoration as a way to improve graft survival, increase hair yield rate, increase hair density and diameter [30]. Miao et al demonstrated significant hair growth in hairless mice when PRP was used [31]. Leo et al performed a systematic review of the aesthetic uses of PRP in dermatology and found current clinical studies suggest its utility in not only hair restoration, but also in scar revision, skin rejuvenation, and treatment of skin disease [32]. The authors also noted that there may also be added benefit of using PRP in combination with other modalities, such as lasers. While current clinical studies are suggestive of the benefits of PRP therapy, more studies are needed to evaluate the effectiveness of PRP in hair restoration.
Future of hair transplant
Prostaglandin therapy: When it was discovered that Latisse (Allergan Inc., Irvine, CA) increased eyelash growth, more studies were targeted at identifying prostaglandin’s role in hair growth. Now it is known that prostaglandin D2 (PGD2) inhibits hair growth and prostaglandin E2 and F2α (PGE2/F2α) promote hair growth [33]. A randomized, double-blinded, placebo-controlled study of a PGF2α applied topically to men with AGA showed an increase in hair density and also extended the anagen phase [34,35]. PGD2 has been found to be elevated in the scalp of bald men, but no clinical studies are currently available to assess a PGD2 antagonist’s effect on hair growth [33].
Stem cell therapy: The current standard in hair restoration is the use and redistribution of already existing hair follicles. For patients without an adequate donor supply, they are currently without any options for hair restoration. Stem cell research is underway in hopes of unlocking the potential for new hair growth. Some researchers are investigating methods to reactivate follicles that have lost their ability to grow hair due to AGA [11]. These follicles retain their stem cells within the bulge region but lack the ability to form new hair. Gene therapy may be the key to re-activating these follicles.
Conclusion
The evolution of hair transplantation surgery now offers patients natural and aesthetically pleasing results that can be achieved reliably. FUT, whether by the strip method or FUE, is the gold standard. Instrumentation for FUE has evolved from manual punches to modern tools such as the NeoGraft machine and the ARTAS robot that allow for quick and safe harvest of grafts. For patients with severe baldness, options are limited; therefore research dedicated to stem cell therapy and gene therapy may be the next frontier in hair restoration therapy.
References
- Gupta AK, Lyons DC, Daigle D (2015) Progression of surgical hair restoration techniques. J Cutan Med Surg 19: 17-21.
- Lee TS, Minton TJ (2009) An update on hair restoration therapy. Curr Opin Otolaryngol Head Neck Surg 17: 287-294.
- Rousso DE, Kim SW (2014) A review of medical and surgical treatment options for androgenetic alopecia. JAMA Facial Plast Surg 16: 444-450.
- Price VH (1999) Treatment of hair loss. N Engl J Med 341: 964-973.
- Drake L (1999) The effects of finasteride on scalp skin and serum androgen levels in men with androgenetic alopecia. J Am Acad Dermatol 41: 550-554.
- Kaufman KD (1998) Finasteride in the treatment of men with androgenetic alopecia. Finasteride Male Pattern Hair Loss Study Group. J Am Acad Dermatol 39: 578-589.
- Irwig MS, Kolukula S (2011) Persistent sexual side effects of finasteride for male pattern hair loss. J Sex Med 8: 1747-1753.
- Carmina E, Lobo RA (2003) Treatment of hyperandrogenic alopecia in women. Fertil Steril 79: 91-95.
- Yim E, Nole KL, Tosti A (2014) 5α-Reductase inhibitors in androgenetic alopecia. Curr Opin Endocrinol Diabetes Obes 21: 493-498.
- GubelinHarcha W, BarbozaMartínez J, Tsai TF, Katsuoka K, Kawashima M, et al. (2014) A randomized, active- and placebo-controlled study of the efficacy and safety of different doses of dutasteride versus placebo and finasteride in the treatment of male subjects with androgenetic alopecia. J Am Acad Dermatol 70: 489-498.
- Gupta AK, Charrette A (2014)The efficacy and safety of 5α-reductase inhibitors in androgenetic alopecia: a network meta-analysis and benefit-risk assessment of finasteride and dutasteride. J Dermatolog Treat 25: 156-161.
- Jung JY, Yeon JH, Choi JW, Kwon SH, Kim BJ, et al. (2014) Effect of dutasteride 0.5 mg/d in men with androgenetic alopecia recalcitrant to finasteride. Int J Dermatol 53: 1351-1357.
- Piérard-Franchimont C, De Doncker P, Cauwenbergh G, Piérard GE (1998) Ketoconazole shampoo: effect of long-term use in androgenic alopecia. Dermatology 196: 474-477.
- Jiang J, Tsuboi R, Kojima Y, Ogawa H (2005) Topical application of ketoconazole stimulates hair growth in C3H/HeN mice. J Dermatol 32: 243-247.
- Inui S, Itami S (2007) Reversal of androgenetic alopecia by topical ketoconzole: relevance of anti-androgenic activity. J DermatolSci 45: 66-68.
- Bernstein RM, Rassman WR (1997) Follicular transplantation. Patient evaluation and surgical planning.DermatolSurg 23: 771-784.
- Epstein JS (2003) Follicular-unit hair grafting: state-of-the-art surgical technique. Arch Facial PlastSurg 5: 439-444.
- Alfonso M, Richter-Appelt H, Tosti A, Viera MS, García, M (2005)The psychosocial impact of hair loss among men: a multinational European study. Curr Med Res Opin 21: 1829-1836.
- Rassman WR, Bernstein RM, McClellan R, Jones R, Worton E, et al. (2002) Follicular unit extraction: minimally invasive surgery for hair transplantation. Dermatol Surg 28: 720-728.
- Harris JA (2006) New methodology and instrumentation for follicular unit extraction: lower follicle transection rates and expanded patient candidacy. Dermatol Surg32: 56-61.
- Harris JA (2013) Follicular unit extraction. Facial Plast Surg Clin North Am 21: 375-384.
- Umar S (2011) Hair transplantation in patients with inadequate head donor supply using nonhead hair: report of 3 cases. Ann Plast Surg 67: 332-335.
- Onda M, Igawa HH, Inoue K, Tanino R (2008) Novel technique of follicular unit extraction hair transplantation with a powered punching device. Dermatol Surg 34: 1683-1688.
- Rose PT, Nusbaum B (2014) Robotic hair restoration. Dermatol Clin 32: 97-107.
- Al-Watban FA, Zhang XY, Andres BL (2007) Low-level laser therapy enhances wound healing in diabetic rats: a comparison of different lasers. Photomed Laser Surg 25: 72-77.
- Lampl Y, Zivin JA, Fisher M, Lew R, Welin L, et al. (2007) Infrared laser therapy for ischemic stroke: a new treatment strategy: results of the NeuroThera Effectiveness and Safety Trial-1 (NEST-1). Stroke 38: 1843-1849.
- Hamblin MR, Newman EL (1994) On the mechanism of the tumour-localising effect in photodynamic therapy. J Photochem Photobiol B 23: 3-8.
- Avram MR, Leonard RT, Epstein ES, Williams JL, Bauman AJ (2007) The current role of laser/light sources in the treatment of male and female pattern hair loss. J Cosmet Laser Ther 9: 27-28.
- Eppley BL, Pietrzak WS, Blanton M (2006) Platelet-rich plasma: a review of biology and applications in plastic surgery. PlastReconstrSurg 118: 147e-159e.
- Lopez V, Vaya A, Bautista D, Ricart JM (2013) Autologous platelet-rich plasma as a potential therapeutic tool in androgenetic alopecia. Journal of the American Academy of Dermatology 68: AB103-AB103.
- Miao Y, Sun YB, Sun XJ, Du BJ, Jiang JD, et al.(2013) Promotional effect of platelet-rich plasma on hair follicle reconstitution in vivo. Dermatol Surg 39: 1868-1876.
- Leo MS, Kumar AS, Kirit R, Konathan R, Sivamani RK (2015) Systematic review of the use of platelet-rich plasma in aesthetic dermatology. J Cosmet Dermatol.
- Keaney T (2015) Emerging Therapies for Androgenetic Alopecia. J Drugs Dermatol 14: 1036-1040.
- Choi YM, Diehl J, Levins PC (2015) Promising alternative clinical uses of prostaglandin F2α analogs: beyond the eyelashes. J Am AcadDermatol 72: 712-716.
- Blume-Peytavi U, Lönnfors S, Hillmann K, Garcia Bartels N (2012) A randomized double-blind placebo-controlled pilot study to assess the efficacy of a 24-week topical treatment by latanoprost 0.1% on hair growth and pigmentation in healthy volunteers with androgenetic alopecia. J Am Acad Dermatol 66: 794-800.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences