A Rare Case of Juvenil Giant Fibroadenoma
Zeynep Altuntas
DOI10.4172/2472-1905.100030
Mehmet Emin Cem YÃÆââ¬Å¾ÃâñldÃÆââ¬Å¾ÃâñrÃÆââ¬Å¾Ãâñm1, Sidika Findik2 and Zeynep Altuntas1*
1Department of Plastic, Reconstructive and Aesthetic Surgery, School of the Medicine, Necmettin Erbakan University, Konya,Turkey
2Department of Pathology, School of the Medicine, Necmettin Erbakan University, Konya, Turkey
- *Corresponding Author:
- Zeynep Altuntas
Department of Plastic and Reconstructive and Aesthetic Surgery
School of the Medicine
Necmettin Erbakan University
42080 Meram, Konya, Turkey
Tel: +90 332 223 60 00-7033
Fax: +90 332 323 61 81
E-mail: zeynepkaracor@yahoo.com
Received Date: August 12, 2016; Accepted Date: August 22, 2017; Published Date: August 30, 2017
Citation: YÃÆââ¬Å¾ÃâñldÃÆââ¬Å¾ÃâñrÃÆââ¬Å¾Ãâñm MEC, Findik S, Altuntas Z (2017) A Rare Case of Juvenil Giant Fibroadenoma. J Aesthet Reconstr Surg. 3:7. doi: 10.4172/2472-1905.100030
Introduction
The most common cause of breast masses seen in young women is fibroadenomas. It is characterized as benign. Etiologically, increased estrogen and receptor susceptibility have been accused [1]. Mass growth usually stops when it reaches 2 cm in size. Those with a size greater than 5 cm are called giant fibroadenomes [2]. Juvenile giant fibroadenomas are very rare cases and constitute 0.5% of all fibroadenomas. In this study, we present a 12-year-old female patient of giant juvenile fibroadenoma.
Case Report
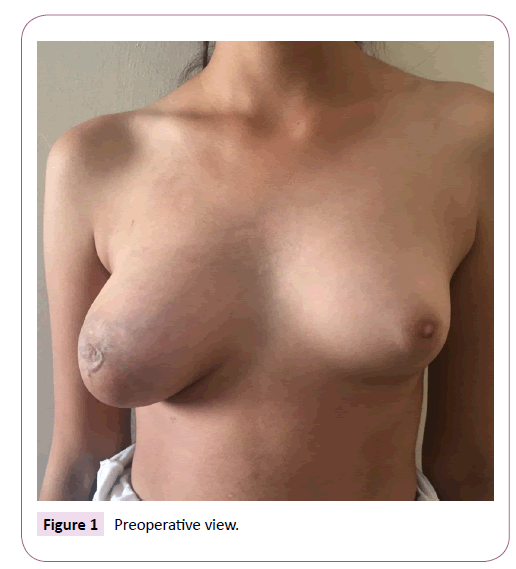
12 years old female patient was admitted to our clinic with complaints of rapid and excessive growth in her right breast. This complaints had existed for 2-3 months and there was not any systemic disease in the history of the patient A painless, circumferentially aligned, mobile mass covering the entire of both lower quadrants and upper inner quadrant was detected on the breast examination (Figure 1). Her armpit examination was normal. Other physical examination findings were normal. Biochemical tests and hormone levels were normal. Ultrasonographic imaging of the patient revealed a solid mass, that has well defined border, with a heterogeneous structure of vascular blood vessels at the 100 × 65 × 45 mm retroareolar placement. Magnetic Resonance ÃÆââ¬Å¾Ãâðmagination (MRI) revealed mass lesions covering both the lower and upper inner quadrants of the breast which was hyperintense and well defined border in the fat-suppressed T2-weighted series.
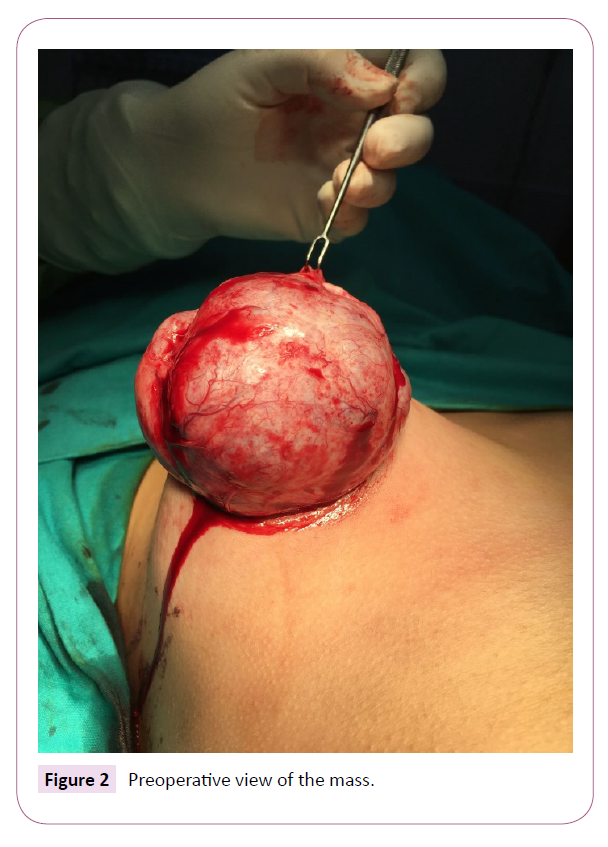
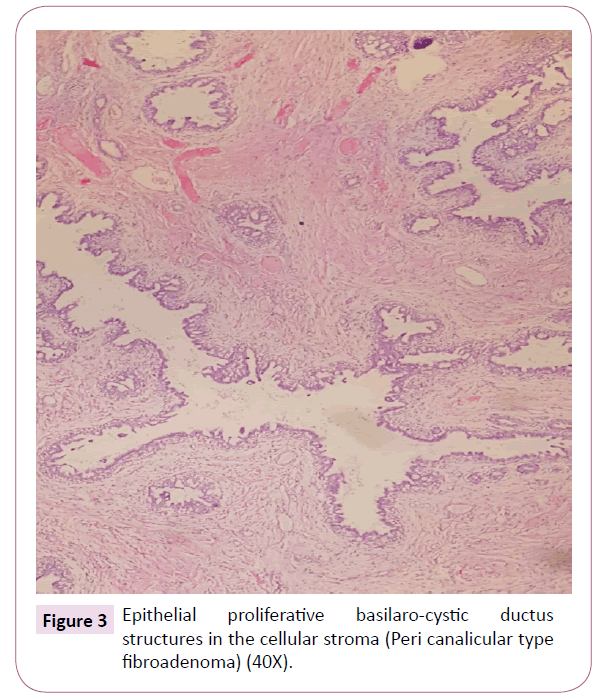
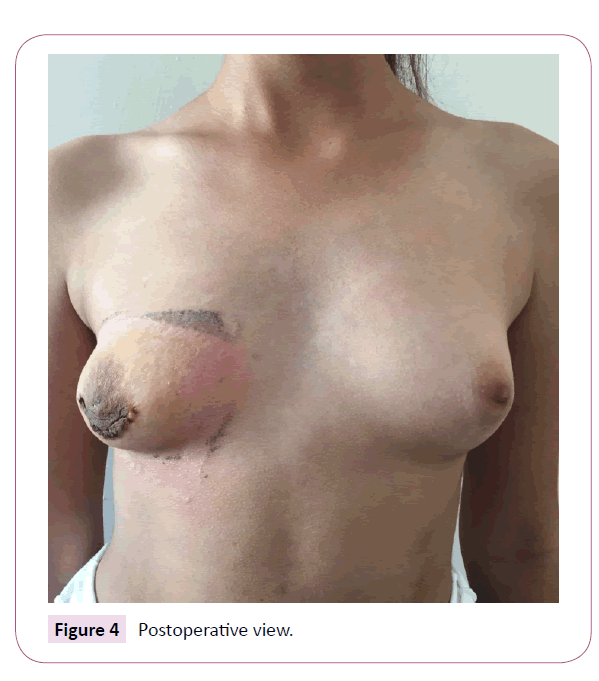
A true cut biopsy was performed for preliminary diagnosis and diagnosed as juvenil fibroadenoma. The mass was removed totally by periareolar incision. We did not made any attempt to provide nipple-areola complex symmetry since the patient's physical development continued. There were no complications in postoperative period. Histopathologic diagnosis was revealed as pericanalicular type Juvenil giant fibroadenoma (Figures 2 and 3). Postoperatively, cosmetic appearance was satisfactory (Figure 4).
Discussion and Conclusion
Giant juvenile fibroadenomas, composed of epithelium and/or stroma of the terminal lobule of the breast, represent only 0.5% of all fibroadenomas [1]. Fibroadenomas, which are well defined border and encapsulated, grow rapidly as they reach large sizes [3]. However, breast asymmetry, nipple irregularities, and congestion may occur with mass effect [4]. In our case, there was serious asymmetry reagrding the breast and nipple size.
Juvenile fibroadenomas usually present during puberty in the age range of 11-18 years and are usually painless lesions [5]. The youngest known case in the literature is a 13-month-old girl [6]. To date, there is a lack of specific guidelines regarding the optimal management of giant juvenile fibroadenomas likely due to conflicting diagnostic and treatment strategies. Breast surgeons, gynecologists, pediatricians, pediatric surgeons and plastic surgeons may encounter giant juvenile fibroadenoma. These patients should be referred to an experienced specialist and a more specific assessment and treatment strategy should be established on this issue.
Imaging methods should be performed after breast and axillary examination in every patient who comes with the mass complaint in breast. Mammography is not preferred due to increased densities in women under 40 years of age [7]. For this reason, the most common method is USG in young women. Smith et al. found that patients aged 25 and younger suspected to have a fibroadenoma on ultrasound had 78.8% accuracy in diagnosis based on histology [8]. Obtaining tissue is also required to differentiate between juvenile giant fibroadenomas and philloides tumors, malignant tumors. Care must be taken in terms of malignancy in the differential diagnosis and especially phylloides tumors should be considered. Philloides tumor is a rare fibroepithelial breast tumor that accounts for less than 1% of all primary breast neoplasms, 2-3% of all fibroepithelial tumors [9,10]. They are similar benign fibroadenoma but distinguished from benign fibroadenomas, histologically increased cellularity and clinically local recurrence and metastatic spread. Therefore, the patient who is diagnosed with breast mass should be evaluated in terms of physical examination, imaging and biopsy. There are studies in the literature that suggest that Fine Needle Aspiration (FNA) biopsies are not reliable. one of the largest series of over 1,400 FNAs of adolescent breast masses, Kapina et al. concluded FNA is not required [11]. However, sensitivity of the true-cut biopsy in the literature is reported to be 88-98%, specificity 94-100%, and accuracy 93-99% [12,13]. Thus, in our case, true-cut biopsy was performed instead of fine needle biopsy for tissue obtaining after imaging and histopathological preliminary diagnosis came as juvenile fibroadenoma.
The treatment of juvenile fibroadenoma is excision or observation. In cases of simple fibroadenoma, conservative treatment may be preferred as 10% of the lesions spontaneously resolve. However, in cases of giant fibroadenomas, surgical treatment should be performed and additional reconstructive procedures might be necessary. In the age of puberty, tumor excision and simultaneous breast reconstruction principles can be performed to protect the breast parenchyma, provide symmetry of the nipple-areola complex and avoid iatrogenic amastia [11,14]. Revision surgeries may be needed in order to provide a cosmetic appearance after the excision of the mass. In our case, we removed the mass by periareolar incision and the remaining breast tissue in the upper quadrant was sufficient to provide the symmetry when compared to the counter-breast. However, since the patient was in the age of growth, the possible revision operations for nipple–areolar complex symmetry were postponed after puberty.
References
- Sosin M, Pulcranoz M, Feldman ED, Patel KM, Nahabedian MY, et al. (2015) Giant juvenile fibroadenoma: A systemic review with diagnostic and treatment recommendation. Gland Surg 4: 312-321.
- Marchant DJ (2002) Benign breast disease. Obstet Gynecol Clin North Am 29: 1-20.
- ÇalÃÆââ¬Å¾ÃâñÃÆââ¬Â¦Ãâà ¸kan M, Acar A, Erdem H, Kurt MD, SubaÃÆââ¬Â¦Ãâà ¸ÃÆââ¬Å¾Ãâñ ÃÆââ¬Å¾ÃâðE, et al. (2011) Juvenile giant fibroadenoma: case report. Medical Journal of Umraniye 3: 17-19.
- Thuruthiyath N, Das PC, Avabratha KS, Mascarenhas V, Marla N (2012) Giant fibroadenoma of breast in anadolescent girl. Oman Med J 27: 314-315.
- Wechselberger G, Schoeller T, Piza-Katzer H (2002) Juvenile fibroadenoma of the breast. Surgery 132: 106-107.
- Jung YS, Lee KJ, Yoon TI (2005) Juvenile fibroadenoma in 13-month-old female child. J Paediatr Child Health 41: 78-79.
- Templeman C, Hertweck SP (2000) Breast disorders in the pediatric and adolescent patient. Obstet Gynecol Clin North Am 27: 19-34.
- Smith GE, Burrows P (2008) Ultrasound diagnosis of fibroadenoma-is biopsy always necessary? Clin Radiol 63: 511-515.
- Obuigbo W (2003) Breast fibroadenoma in teenage females. Turkish J Pediatr 45: 326-328.
- Parker SJ, Harries SA (2001) Phyllodes tumours. Postgrad Med J 77: 428-435.
- Kapila K, Pathan SK, Al-Mosawy FA (2008) Fine needle aspiration cytology of breast masses in children and adolescents: experience with 1404 aspirates. Acta Cytol 52: 681-686.
- Brunner AH, Sagmeister T, Kremer J, Riss P, Brustmann H (2009) The accuracy of frozen section analysis in ultrasound- guided core needle biopsy of breast lesions. BMC Cancer 24: 341.
- Homesh NA, Issa MA, El-Sofiani HA (2005) The diagnostic accuracy of fine needle aspiration cytology versus core needle biopsy for palpable breast lump(s). Saudi Med J 26: 42-46.
- Chang D, McGrath M (2007) Management of benign tumours of the adolescent breast. Plast Reconstr Surg 120: 13e-19e.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences