Insights from Submental Plication Four-Months Following Helium Plasma Radio Frequency Treatment
Suzanne A Trott*
Private Practice in Beverly Hills, CA, and attending physician at Cedars Sinai Medical Center, Los Angeles, CA
Suzanne A Trott*
Private Practice in Beverly Hills, CA, and attending physician at Cedars Sinai Medical Center, Los Angeles, CA
- *Corresponding Author:
- Suzanne A Trott
Private Practice in Beverly Hills, CA, and attending physician at Cedars Sinai Medical Center, Los Angeles, CA
E-mail: drtrott@drtrott.com
Received date: September 18, 2024, Manuscript No. IPARS-24-19662; Editor assigned date: September 20, 2024, PreQC No. IPARS-24-19662 (PQ); Reviewed date: October 04, 2024, QC No. IPARS-24-19662; Revised date: October 11, 2024, Manuscript No. IPARS-24-19662 (R); Published date: October 18, 2024, DOI: 10.36648/2472-1905.10.4.167
Citation: Trott SA (2024) Insights from Submental Plication Four-Months following Helium Plasma Radio Frequency Treatment. J Aesthet Reconstr Surg Vol.10 No.4:167.
Abstract
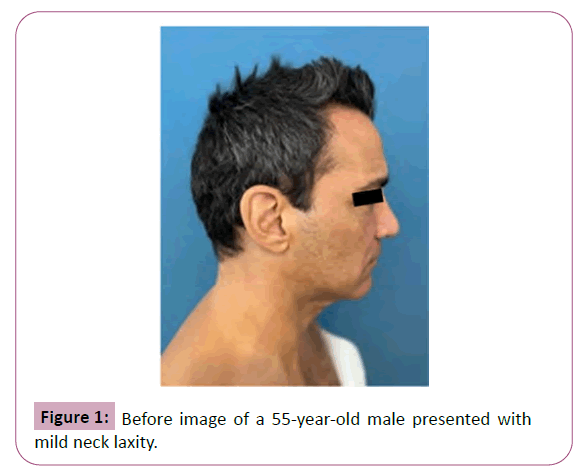
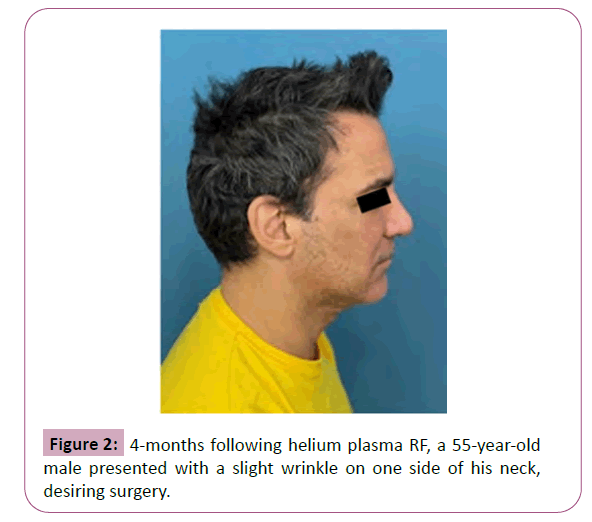
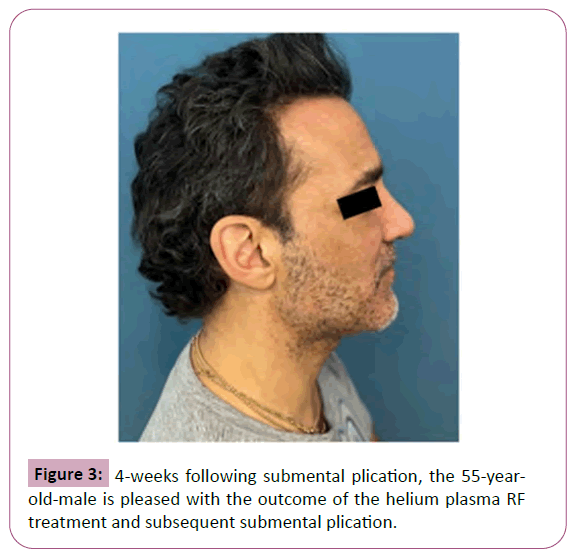
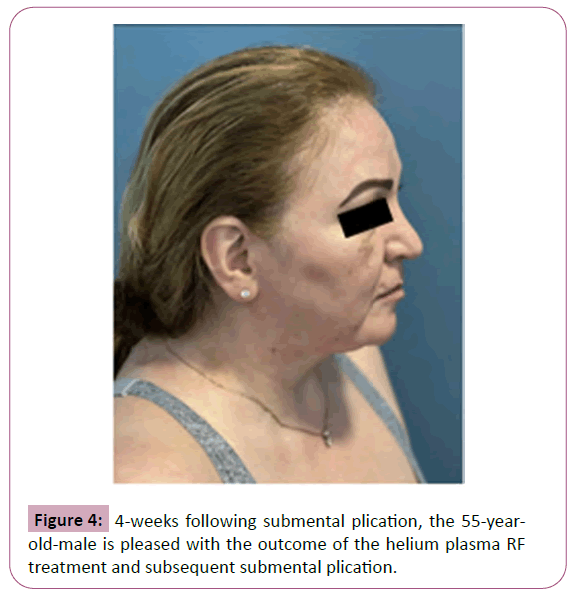
Plastic surgeons have experienced difficulties with surgeries following the use of some Energy-Based Devices (EBDs) which can cause dermal and subdermal planes to stick together from scar tissue and fibrosis. In contrast, we report on supple tissue and clean dissection planes during submental plication four months following the use of a helium plasma Radio Frequency (RF) device in our practice. Two cases are presented: A 55-year-old male patient with mild neck laxity and a 57-year-old female patient with significant submental and neck laxity. Both patients underwent helium plasma RF treatment followed by submental plication under local anesthesia four months later. At four months, post-procedure observations indicated that the helium plasma RF treated tissue remained supple with minimal scarring, clean dissection planes, and without fibrosis. The helium plasma RF treatment did not adversely affect subsequent surgery. The combined use of helium plasma RF followed by submental plication four months later provided significant improvements in neck contour with minimal downtime and was particularly effective for patients over 40. This approach offers an effective solution for those seeking subtle aesthetic enhancements while avoiding the costs and risks associated with general anesthesia and more-invasive procedures.
Keywords
Helium plasma RF; Submental plication; Renuvion; Fibrosis
Introduction
Plastic surgeons have voiced concerns over performing surgical procedures following the application of some Energy-Based Devices (EBD), particularly due to the risk of fibrosis or scar tissue [1,2]. Fibrosis is a recognized potential risk associated with all energy-based technologies that target subdermal tissue, including ultrasound, ultrasound-assisted liposuction, laser-assisted liposuction, monopolar and bipolar bulk tissue heating devices, as well as helium plasma Radio Frequency (RF) [2-6]. It typically occurs when tissue is overheated or over treated, which disrupts the local blood supply, leading to fibrosis. Additionally, the development of a seroma can also contribute to fibrosis formation [7]. In our experience, we have encountered cases where excessive energy from these devices impacted the tissue in a way that complicated later surgeries. Specifically, we performed a face and neck lift on a patient who had been treated for over 20 years with a Radio Frequency (RF) micro-needling device (Morpheus, InMode, Irvine, CA) and a non-invasive RF device (Thermage, Solta medical, Bothell, WA), resulting in dermal and subdermal planes that were adhered together, making the surgery more difficult. For the past nine months, we have been using a helium plasma radio frequency device (Renuvion, Apyx medical, Clearwater, FL) in our private practice and have observed notable improvements in neck and jawline laxity. The helium plasma RF device provides precise controlled heat for tissue contraction and may have different effects on tissue compared with other EBDs. While fibrosis remains a potential risk, data indicates that this risk is very low with helium plasma RF. In an analysis of real-world evidence from six Apyx Medical-sponsored retrospective studies, which included 483 patients and 1,184 treated body areas, only 3 cases of fibrosis were identified, yielding a rate of just 0.25% per treatment area [8]. In this report, we present two cases highlighting submental plication with no fibrosis observed four months following a helium plasma RF device procedure. As far as we are aware, there has been no prior publication documenting tissue pliability following a helium plasma RF procedure.
Case Presentation
Case 1
A 55-year-old male presented with mild neck laxity (Figure 1) and a helium plasma RF treatment was performed to the neck and jawline, procedure details were 60% power, 1.5 L of helium flow and 10 kJ to each side. Four months following the helium plasma RF treatment, the patient had a slight wrinkle on one side of the neck and expressed interest in surgery (Figure 2). Four months posthelium plasma RF, the patient underwent submental plication under local anesthesia. The procedure was straightforward with a clean dissection plane. There were no issues in the tissue from the previous helium plasma RF procedure. The patient was very pleased at four weeks post submental plication (Figure 3).
Case 2
A 57-year-old female presented with significant submental and neck laxity (Figure 4) and a helium plasma RF treatment was performed to the neck and jawline, procedure details were 60% power, 1.5 L of helium flow and 10 kJ to each side. The patient had a pre-existing scar under the chin from a childhood injury which had left a dog-ear and sought corrective surgery. Four months following Renuvion (Figure 5), submental plication was performed under local anesthesia. Intraoperatively, the tissue was clean, supple, of excellent quality and easy to dissect (Videos 1 and 2).
Video 1: Submental plication demonstrating ease of dissection, similar to a skin flap previously untreated with EBD.
Video 2: Submental plication demonstrating skin flap easily being dissected, the area free of fibrosis.
Both cases followed a similar postoperative care regimen following the helium plasma RF procedure and subsequently, the submental plication surgery:
• Compression garment immediately after the procedure.
• Chin strap/neck band for one week continuously, then at night for another week.
• Encouragement to wear the neck band as much as possible for additional weeks.
• For submental plication, netting sutures removed at 48 h and incision sutures removed at one week.
• Weekly Aspen ultrasound for swelling and lymphatic massage.
Results and Discussion
In plastic surgery, performing secondary procedures on tissue previously treated with EBD or liposuction is a well-known challenge. Cook reports a roundtable discussion on secondary liposuction, where physicians agree that these cases are often very difficult due to the presence of fibrotic scar tissue [9]. In a systematic review of subsurface radio frequency treatments in plastic surgery, Swanson noted that the most frequently reported complication of energy application with the BodyTite and ThermiTight EBDs was the hardening of the subcutaneous tissue, resulting in induration and nodules [5]. Historically, this concern was noted by Avelar in 1989, who reported that previously treated subcutaneous tissue often showed thick and hard fibrosis, leading to surface irregularities and waves [10]. This issue remains pertinent, as Mera-Cruz et al., reported in 2024 that current evidence on managing fibrosis after previous liposuction is still limited [11].
In this case-series, however the author observed that treatment with helium plasma RF in alignment with the instructions for use and the safe and effective use guidelines established did not result in residual fibrosis or hardening of the subcutaneous tissue that has been observed in other types of cosmetic surgeries. The precise and controlled heat applied by helium plasma RF may account for the absence of these complications, suggesting that it could be a superior alternative for tissue contraction without inducing fibrosis.
Conclusion
From the observations of these two cases, several key conclusions can be drawn. At four months post-helium plasma RF, the treated tissue remained supple with minimal scarring and clean dissection planes, absent of fibrosis. Subcutaneous and subplatysmal dissection in a neck treated with helium plasma RF was not adversely affected by scar tissue. Combining helium plasma RF with submental plication significantly improved the cervicomental angle and soft tissue neck laxity, providing effective results with minimal downtime. Helium plasma RF’s lateral tightening allows submental plication to be effective in patients over 40, who typically would not benefit from this procedure alone. This combined procedure is particularly beneficial for patients desiring subtler aesthetic improvements and avoiding general anesthesia and operating room expenses. Moreover, it does not preclude the possibility of future face or neck lifts.
Acknowledgement
This article was supported by Apyx Medical.
Conflict of Interest
Dr. Trott is a paid consultant for Apyx Medical.
References
- Skouras GA, Skouras AG, Skoura EA (2020) Revision and secondary facelift: Problems frequently encountered. Plast Reconstr Surg Glob Open 8: e2947.
[Crossref], [Google Scholar], [Indexed]
- Bray D (2024) Extended composite approach to deep plane face lifting with deep contouring of the neck and the nuances of secondary and tertiary facelifting: Principles for restoration of natural anatomy and aesthetically attractive face and neck contour. Facial Plast Surg.
[Crossref], [Google Scholar], [Indexed]
- Roustaei N, Masoumi LSJ, Chalian M, Chalian H, Bakhshandeh H (2009) Safety of ultrasound-assisted liposuction: A survey of 660 operations. Aesthetic Plast Surg 33: 213-218.
[Crossref], [Google Scholar], [Indexed]
- Ali YH (2018) Laser-assisted lipolysis burn safety: Proposed detailed parameters with assessment of their efficacy and safety. Plast Reconstr Surg Glob Open 6: e1934.
[Crossref], [Google Scholar], [Indexed]
- Swanson E (2022) A systematic review of subsurface radiofrequency treatments in plastic surgery. Ann Plast Surg 89: 274-285.
[Crossref], [Google Scholar], [Indexed]
- Ruff PG, Vanek P, Nykiel M (2022) Adverse events of soft tissue coagulation using a helium-based plasma technology alone and in combination with ultrasound-assisted liposuction. Aesthet Surg J Open Forum.
[Crossref], [Google Scholar], [Indexed]
- Mata C, Gadayev M, Ferrara GP, Kesserwani J (2022) Hi-def liposuction: My technique. In: Thomas M, D'silva J. eds. Manual of Cosmetic Surgery and Medicine. Springer Nature Singapore. 209–217.
[Crossref], [Google Scholar]
- Shridharani SM, Ruff PG, Doolabh VB, Zimmerman EM (2023) The safety of contraction of subcutaneous tissue following liposuction procedures. Aesthet Surg J Open Forum 6: ojad112.
[Crossref], [Google Scholar], [Indexed]
- Cook J, Pozner JN, Turer DM, DiBernardo BE, Bharti G, et al. (2021) Roundtable discussion: Making sense of current liposuction technologies. Aesthet Surg J Open Forum 4: ojab045.
[Crossref], [Google Scholar], [Indexed]
- Avelar J (1989) Regional distribution and behavior of the subcutaneous tissue concerning selection and indication for liposuction. Aesthet Plast Surg 13: 155-165.
[Crossref], [Google Scholar], [Indexed]
- Mera-Cruz G, Durán H, Murillo-Romero N, Pérez M, Rubiano V, et al. (2024) Fibrosis management algorithm in secondary liposculpture. Aesthet Surg J 44: 859-868.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences